Abstract
Purpose
To describe diagnostic results following re-biopsy of blastocysts with inconclusive results on preimplantation genetic screening for aneuploidy (PGT-A) and to evaluate the reproductive potential of re-biopsied blastocysts.
Methods
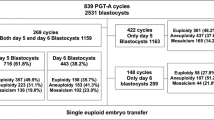
This retrospective cohort study included all trophectoderm biopsies submitted for PGT-A by a large in vitro fertilization center to a single genetics laboratory from June 2016 to October 2018. PGT-A was performed using next-generation sequencing (NGS). No-result blastocysts that underwent re-biopsy were subsequently classified as euploid, aneuploid, mosaic/segmental, or no-result. Ongoing pregnancy and clinical loss rates were assessed following transfer of re-biopsied blastocysts. Logistic regressions were conducted to account for age and blastocyst morphology.
Results
Of the trophectoderm biopsies submitted for PGT-A, 635/25,199 (2.5%) were categorized as no-result. Those that underwent re-biopsy (n = 250) had a 95.2% diagnostic rate with 140 (56.0%) receiving euploid diagnoses. Thirty-six re-biopsied blastocysts deemed euploid were subsequently transferred, resulting in 18 (50.0%) ongoing pregnancies and 5 (13.9%) clinical losses. After adjusting for age and blastocyst morphology, there remained a lower ongoing pregnancy rate and a trend towards higher clinical loss rate following transfer of a re-biopsied blastocyst. When compared to blastocysts that underwent the same number of vitrification-warming cycles but only one biopsy, there were no differences in outcomes.
Conclusions
Failure to obtain an analytical result does not change the probability that a given blastocyst is euploid. Pregnancy outcomes following transfer of re-biopsied blastocysts are favorable, but further data must be accrued for an adequately powered comparison with outcomes after transfer of blastocysts biopsied once.



Similar content being viewed by others
References
Cimadomo D, Rienzi L, Romanelli V, Alviggi E, Levi-Setti PE, Albani E, et al. Inconclusive chromosomal assessment after blastocyst biopsy: prevalence, causative factors and outcomes after re-biopsy and re-vitrification. A multicenter experience. Hum Reprod Oxf Engl. 2018;33(10):1839–46.
Brower M, Hill D, Danzer H, Surrey M, Ghadir S, Chang W, et al. “No diagnosis” embryos after PGS should not be discarded: rebiopsy and reanalysis demonstrate the majority are euploid. Fertil Steril. 2014;102(3):e31.
Kaing A, Kroener L, Brower M, Hill D, Danzer H, Barritt J. Rebiopsy and preimplanation genetic screening (PGS) reanalysis demonstrate the majority of originally “no diagnosis” embryos are euploid with comparable pregnancy rates. Fertil Steril. 2015;104(3):e277.
Lee H, McCulloh DH, Olivares R, Goldstein-Tufaro A, McCaffrey C, Grifo J. Live births after transfer of rebiopsy and revitrification of blastocyst that had “no diagnosis” following trophectoderm biopsy. Fertil Steril. 2016;106(3):e164.
Neitzel D, Alouf CA, Robinson K, Zhu M, Faulkner N. Re-biopsied pgs embryos yield actionable results. Fertil Steril. 2017;108(3):e290.
Priner S, Altarescu G, Schonberger O, Holzer H, Rubinstein E, Dekel N, et al. The effect of repeated biopsy on pre-implantation genetic testing for monogenic diseases (PGT-M) treatment outcome. J Assist Reprod Genet. 2018.
Heitmann RJ, Hill MJ, Richter KS, DeCherney AH, Widra EA. The simplified SART embryo scoring system is highly correlated to implantation and live birth in single blastocyst transfers. J Assist Reprod Genet. 2013;30(4):563–7.
Zhang S, Tan K, Gong F, Gu Y, Tan Y, Lu C, et al. Blastocysts can be rebiopsied for preimplantation genetic diagnosis and screening. Fertil Steril. 2014;102(6):1641–5.
Swain JE, Schoolcraft WB, Katz-Jaffe M. Dual trophectoderm biopsy on the same blastocyst does not impair clinical outcomes. Fertil Steril. 2015;104(3):e186.
Bradley CK, Livingstone M, Traversa MV, McArthur SJ. Impact of multiple blastocyst biopsy and vitrification-warming procedures on pregnancy outcomes. Fertil Steril. 2017;108(6):999–1006.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Neal, S.A., Sun, L., Jalas, C. et al. When next-generation sequencing-based preimplantation genetic testing for aneuploidy (PGT-A) yields an inconclusive report: diagnostic results and clinical outcomes after re biopsy. J Assist Reprod Genet 36, 2103–2109 (2019). https://doi.org/10.1007/s10815-019-01550-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01550-6