Abstract
Purpose
Does blastocyst morphology following euploid elective single embryo transfer (eSET) after preimplantation genetic testing for aneuploidies (PGT-A) via next generation sequencing impact clinical outcome?
Methods
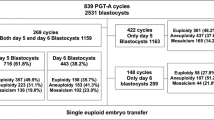
Two hundred ninety-six patients underwent PGT-A. Of 1549 blastocysts, 1410 blastocysts had a conclusive result after PGT-A and were included for analysis. An eSET policy was followed in a frozen embryo replacement cycle. A total of 179 euploid blastocysts were thawed and transferred. Clinical outcomes were categorized in four different embryo quality groups: excellent, good, average and poor.
Results
Euploidy rate was 19/36 (52.7%, 95% CI 37–68), 199/470 (42.3%, 95% CI 38–47), 156/676 (23.0%, 95% CI 20–26) and 39/228 (17.1%, 95% CI 13–23) in the excellent, good, average and poor quality blastocyst groups, respectively. Fitted logistic regression analysis taking into account the following covariables: female, age, embryo chromosomal status and day of blastocyst development/biopsy showed that morphology was predictive of the comprehensive chromosome screening result (p < 0.05). A logistic regression analysis was also performed on clinical outcomes taking into account the effect of blastocyst morphology and day of blastocyst development/biopsy. None of the parameters were shown to be significant, suggesting morphology and day of blastocyst development/biopsy do not reduce the competence of euploid embryos (p > 0.05).
Conclusions
After eSET, implantation rate was 80–86%; live birth rate per embryo transfer was 60–73% and clinical miscarriage rate was found to be < 10% and were not significantly affected by the embryo morphology. Results are concordant with those reported when using aCGH and highlights the competence of poor-quality euploid embryos.
Similar content being viewed by others
References
Alfarawati S, Fragouli E, Colls P, Stevens J, Gutierrez-Mateo C, Schoolcraft WB, et al. The relationship between blastocyst morphology, chromosomal abnormality, and embryo gender. Fertil Steril. 2011;95(2):520–4.
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26(6):1270–83.
Ben-Nagi J, Wells D, Doye K, Loutradi K, Exeter H, Drew E, et al. Karyomapping: a single centre’s experience from application of methodology to ongoing pregnancy and live-birth rates. Reprod BioMed Online. 2017;35:264–71.
Capalbo A, Rienzi L, Cimadomo D, Maggiulli R, Elliott T, Wright G, et al. Correlation between standard blastocyst morphology, euploidy and implantation: an observational study in two centers involving 956 screened blastocysts. Hum Reprod. 2014;29(6):1173–81.
ESHRE Special Interest Group of Embryology and Alpha Scientists in Reproductive Medicine. Electronic address: coticchio.biogenesi@grupposandonato.itThe Vienna consensus: report of an expert meeting on the development of ART laboratory performance indicators. Reprod BioMed Online. 2017;35(5):494–510.
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, et al. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril. 2013;100(1):100–7.e1.
Fragouli E, Alfarawati S, Daphnis DD, Goodall NN, Mania A, Griffiths T, et al. Cytogenetic analysis of human blastocysts with the use of FISH, CGH and aCGH: scientific data and technical evaluation. Hum Reprod. 2011;26(2):480–90.
Gardner DK, Schoolcraft WB. Culture and transfer of human blastocysts. Curr Opin Obstet Gynecol. 1999;11(3):307–11.
Garrisi JG, Colls P, Ferry KM, Zheng X, Garrisi MG, Munne S. Effect of infertility, maternal age, and number of previous miscarriages on the outcome of preimplantation genetic diagnosis for idiopathic recurrent pregnancy loss. Fertil Steril. 2009;92(1):288–95.
Harton GL, Munne S, Surrey M, Grifo J, Kaplan B, McCulloh DH, et al. Diminished effect of maternal age on implantation after preimplantation genetic diagnosis with array comparative genomic hybridization. Fertil Steril. 2013;100(6):1695–703.
Hodes-Wertz B, Grifo J, Ghadir S, Kaplan B, Laskin CA, Glassner M, et al. Idiopathic recurrent miscarriage is caused mostly by aneuploid embryos. Fertil Steril. 2012;98(3):675–80.
Irani M, Reichman D, Robles A, Melnick A, Davis O, Zaninovic N, et al. Morphologic grading of euploid blastocysts influences implantation and ongoing pregnancy rates. Fertil Steril. 2017;107(3):664–70.
Majumdar G, Majumdar A, Verma IC, Upadhyaya KC. Relationship between morphology, Euploidy and implantation potential of cleavage and blastocyst stage embryos. J Hum Reprod Sci. 2017;10(1):49–57.
Minasi MG, Colasante A, Riccio T, Ruberti A, Casciani V, Scarselli F, et al. Correlation between aneuploidy, standard morphology evaluation and morphokinetic development in 1730 biopsied blastocysts: a consecutive case series study. Hum Reprod. 2016;31(10):2245–54.
Munne S, Chen S, Fischer J, Colls P, Zheng X, Stevens J, et al. Preimplantation genetic diagnosis reduces pregnancy loss in women aged 35 years and older with a history of recurrent miscarriages. Fertil Steril. 2005;84(2):331–5.
Neal S, et al. Preimplantation gentic testing for aneuploidy is cost effective, shortens treatment time, and reduces the risk of failed embryo transfer and clinical miscarriage. Fertil Steril. 2018;110(5):896–904.
Rubio C, Simon C, Vidal F, Rodrigo L, Pehlivan T, Remohi J, et al. Chromosomal abnormalities and embryo development in recurrent miscarriage couples. Hum Reprod. 2003;18(1):182–8.
Scott RT Jr, Franasiak JM, Forman EJ. Comprehensive chromosome screening with synchronous blastocyst transfer: time for a paradigm shift. Fertil Steril. 2014;102(3):660–1.
Veeck L, Zaninovic N. Human blastocysts in vitro. In: Veeck L, Zaninovic N, editors. An atlas of human blastocysts. Boca Raton: Parthenon Publishing; 2009. p. 99–137.
Wirleitner B, Schuff M, Stecher A, Murtinger M, Vanderzwalmen P. Pregnancy and birth outcomes following fresh or vitrified embryo transfer according to blastocyst morphology and expansion stage, and culturing strategy for delayed development. Hum Reprod. 2016;31(8):1685–95.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Viñals Gonzalez, X., Odia, R., Naja, R. et al. Euploid blastocysts implant irrespective of their morphology after NGS-(PGT-A) testing in advanced maternal age patients. J Assist Reprod Genet 36, 1623–1629 (2019). https://doi.org/10.1007/s10815-019-01496-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01496-9