Abstract
The use of immature oocytes subjected to in vitro maturation (IVM) opens interesting perspectives for fertility preservation where ovarian reserves are damaged by pathologies or therapies, as in PCO/PCOS and cancer patients. Human oocyte cryopreservation may offer some advantages compared to embryo freezing, such as fertility preservation in women at risk of losing fertility due to oncological treatment or chronic disease, egg donation and postponing childbirth. It also eliminates religious and/or other ethical, legal, and moral concerns of embryo freezing. In addition, a successful oocyte cryopreservation program could eliminate the need for donor and recipient menstrual cycle synchronization. Recent advances in vitrification technology have markedly improved the oocyte survival rate after warming, with fertilization and implantation rates comparable with those of fresh oocytes. Healthy live births can be achieved from the combination of IVM and vitrification, even if vitrification of in vivo matured oocytes is still more effective. Recently, attention is given to highlight whether vitrification procedures are more successful when performed before or after IVM, on immature GV-stage oocytes, or on in vitro matured MII-stage oocytes. In this review, we emphasize that, even if there are no differences in survival rates between oocytes vitrified prior to or post-IVM, reduced maturation rates of immature oocytes vitrified prior to IVM can be, at least in part, explained by underlying ultrastructural and biomolecular alterations.





Similar content being viewed by others
References
Trounson A, Wood C, Kausche A. In vitro maturation and the fertilization and developmental competence of oocytes recovered from untreated polycystic ovarian patients. Fertil Steril. 1994;62:35362.
Lim KS, Chae SJ, Choo CW, Ku YH, Lee HJ, Hur CY, et al. In vitro maturation: Clinical applications. Clin Exp Reprod Med. 2013;40(4):143–7.
Gremeau AS, Andreadis N, Fatum M, Craig J, Turner K, McVeigh E, et al. In vitro maturation or in vitro fertilization for women with polycystic ovaries? A case-control study of 194 treatment cycles. Fertil Steril. 2012;98(2):355–60.
Fadini R, Mignini Renzini M, Dal Canto M, Epis A, Crippa M, Caliari I, et al. Oocyte in vitro maturation in normo-ovulatory women. Fertil Steril. 2013;99:1162–9.
Edwards RG. Maturation in vitro of human ovarian oocytes. Lancet. 1965;2:926–9.
Cha KY, Koo JJ, Ko JJ, Choi DH, Han SY, Yoon TK. Pregnancy after in vitro fertilization of human follicular oocytes collected from nonstimulated cycles, their culture in vitro and their transfer in a donor oocyte program. Fertil Steril. 1991;55:109–13.
Konc J, Kanyó K, Kriston R, Somoskői B, Cseh S. Cryopreservation of embryos and oocytes in human assisted reproduction. Biomed Res Int. 2014;2014:307268.
Rall WF, Fahy GM. Ice-free cryopreservation of mouse embryos at −196°C by vitrification. Nature. 1985;313:573–5.
Rall WF, Fahy GM. Vitrification: an overview. In: Tucker MJ, Liebermann J, editors. Vitrification in assisted reproduction. London: Informa Healthcare; 2007.
Kuwayama M, Vajta G, Kato O, Leibo SP. Highly efficient vitrification method for cryopreservation of human oocytes. Reprod BioMed Online. 2005;11(3):300–8.
Lawson A, Ahmad H, Sambanis A. Cytotoxicity effects of cryoprotectants as single-component and cocktail vitrification solutions. Cryobiology. 2011;62(2):115–22.
Bogliolo L, Murrone O, Piccinini M, Ariu F, Ledda S, Tilocca S, et al. Evaluation of the impact of vitrification on the actin cytoskeleton of in vitro matured ovine oocytes by means of Raman microspectroscopy. J Assist Reprod Genet. 2015;32(2):185–93.
Coello A, Campos P, Remohí J, Meseguer M, Cobo A. A combination of hydroxypropyl cellulose and trehalose as supplementation for vitrification of human oocytes: a retrospective cohort study. J Assist Reprod Genet. 2016;33(3):413–21.
Choi JK, Huang H, He X. Improved low-CPA vitrification of mouse oocytes using quartz microcapillary. Cryobiology. 2015;70(3):269–72.
Molina I, Mari M, Martínez JV, Novella-Maestre E, Pellicer N, Pemán J. Bacterial and fungalcontamination risks in human oocyte and embryo cryopreservation: open versus closed vitrification systems. Fertil Steril. 2016;106(1):127–32.
Parmegiani L, Accorsi A, Bernardi S, Arnone A, Cognigni GE, Filicori M. A reliable procedure for decontamination before thawing of human specimens cryostored in liquid nitrogen: three washes with sterile liquid nitrogen (SLN2). Fertil Steril. 2012;98(4):870–5.
Sarandi S, Herbemont C, Sermondade N, Benoit A, Sonigo C, Poncelet C, et al. A prospective study to compare the efficiency of oocyte vitrification using closed or open devices. Gynecol Obstet Fertil. 2016;44(5):280–4.
Papatheodorou A, Vanderzwalmen P, Panagiotidis Y, Prapas N, Zikopoulos K, Georgiou I, et al. Open versus closed oocyte vitrification system: a prospective randomized sibling-oocyte study. Reprod BioMed Online. 2013;26(6):595–602.
De Munck N, Santos-Ribeiro S, Stoop D, Van de Velde H, Verheyen G. Open versus closed oocyte vitrification in an oocyte donation programme: a prospective randomized sibling oocyte study. Hum Reprod. 2016;31(2):377–84.
Chen Y, Zheng X, Yan J, Qiao J, Liu P. Neonatal outcomes after the transfer of vitrified blastocysts: closed versus open vitrification system. Reprod Biol Endocrinol. 2013;11:107.
Bonetti A, Cervi M, Tomei F, Marchini M, Ortoliani F, Manno M. Ultrastructural evaluation of human metaphase II oocytes after vitrification: closed versus open devices. Fertil Steril. 2011;95:928–35.
Cobo A, Meseguer M, Remohi J, Pellicer A. Use of cryo-banked oocytes in an ovum donation programme: a prospective, randomized, controlled, clinical trial. Hum Reprod. 2010;25:2239–46.
Herrero L, Martinez M, Garcia-Velasco JA. Current status of human oocyte and embryo cryopreservation. Curr Opin Obstet Gynecol. 2011;23:245–50.
Rienzi L, Romano S, Albricci L, Maggiulli R, Capalbo A, Baroni E, et al. Embryo development of fresh “versus” vitrified metaphase II oocytes after ICSI: a prospective randomized sibling-oocyte study. Hum Reprod. 2010;25:66–73.
Cobo A, García-Velasco JA, Coello A, Domingo J, Pellicer A, Remohí J. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil Steril. 2016;105(3):755–64. e8
Khalili MA, Maione M, Palmerini MG, Bianchi S, Macchiarelli G, Nottola SA. Ultrastructure of human mature oocytes after vitrification. Eur J Histochem. 2012;56(3):e38.
Khalili MA, Sultan AM, Mojibian M. Role of oocyte morphology on fertilization and embryo formation in assisted reproductive techniques. Mid East Fertil Soc J. 2005;10:72–7.
Gualtieri R, Mollo V, Barbato V, Fiorentino I, Iaccarino M, Talevi R. Ultrastructure and intracellular calcium response during activation in vitrified and slow-frozen human oocytes. Hum Reprod. 2011;26:2452–60.
Nikiforaki D, Vanden Meerschaut F, Qian C, De Croo I, Lu Y, Deroo T, et al. Oocyte cryopreservation and in vitro culture affect calcium signalling during human fertilization. Hum Reprod. 2014;29(1):29–40.
Chamayou S, Romano S, Alecci C, Storaci G, Ragolia C, Palagiano A, et al. Oocyte vitrification modifies nucleolar remodeling and zygote kinetics—a sibling study. J Assist Reprod Genet. 2015;32(4):581–6.
Leoni GG, Palmerini MG, Satta V, Succu S, Pasciu V, Zinellu A, et al. Differences in the kinetic of the first meiotic division and in active mitochondrial distribution between prepubertal and adult oocytes mirror differences in their developmental competence in a sheep model. PLoS One. 2015;10(4):e0124911.
Lei T, Guo N, Liu JQ, Tan MH, Li YF. Vitrification of in vitro matured oocytes: effects on meiotic spindle configuration and mitochondrial function. Int J Clin Exp Pathol. 2014;15(7(3)):1159–65.
Chen C, Han S, Liu W, Wang Y, Huang G. Effect of vitrification on mitochondrial membrane potential in human metaphase II oocytes. J Assist Reprod Genet. 2012;29(10):1045–50.
Ci Q, Li M, Zhang Y, Ma S, Gao Q, Shi Y. Confocal microscopic analysis of the microfilament configurations from human vitrification-thawed oocytes matured in vitro. Cryo-Letters. 2014;35(6):544–8.
Kim SS, Olsen R, Kim DD, Albertini DF. The impact of vitrification on immature oocyte cell cycle and cytoskeletal integrity in a rat model. J Assist Reprod Genet. 2014;31(6):739–47.
Mohsenzadeh M, Khalili MA, Nazari S, Jahromi VH, Agharahimi A, Halvaei I. Effect of vitrification on morphology and in vitro maturation outcome of human immature oocytes. Ital J Anat Embryol. 2012;117:190–8.
Brambillasca F, Guglielmo MC, Coticchio G, Mignini Renzini M, Dal Canto M, Fadini R. The current challenges to efficient immature oocyte cryopreservation. J Assist Reprod Genet. 2013;30(12):1531–9.
Combelles CM, Chateau G. The use of immature oocytes in the fertility preservation of cancer patients: current promises and challenges. Int J Dev Biol. 2012;56:919–29.
Wang H, Racowsky C, Combelles CM. Is it best to cryopreserve human cumulus-free immature oocytes before or after in vitro maturation? Cryobiology. 2012;65:79–87.
Coticchio G. IVM in need of clear definitions. Hum Reprod. 2016;31(7):1387–9.
Dahan MH, Tan SL, Chung J, Son WY. Clinical definition paper on in vitro maturation of human oocytes. Hum Reprod. 2016;31(7):1383–6.
De Vos M, Smitz J, Thompson JG, Gilchrist RB. The definition of IVM is clear-variations need defining. Hum Reprod. 2016;31(11):2411–5.
Fasano G, Demeestere I, Englert Y. In-vitro maturation of human oocytes: before or after vitrification? J Assist Reprod Genet. 2012;29(6):507–12.
Lee JA, Sekhon L, Grunfeld L, Copperman AB. In-vitro maturation of germinal vesicle and metaphase I eggs prior to cryopreservation optimizes reproductive potential in patients undergoing fertility preservation. Curr Opin Obstet Gynecol. 2014;26(3):168–73.
Mandelbaum J, Junca AM, Tibi C, Plachot M, Alnot MO, Rim H, et al. Cryopreservation of immature and mature hamster and human oocytes. Ann N Y Acad Sci. 1988;541:550–61.
Chian RC, Gilbert L, Huang JY, Demirtas E, Holzer H, Benjamin A, et al. Live birth after vitrification of in vitro matured human oocytes. Fertil Steril. 2009;91:372–6.
Cao Y, Xing Q, Zhang ZG, Wei ZL, Zhou P, Cong L. Cryopreservation of immature and in vitro matured human oocytes by vitrification. Reprod BioMed Online. 2009;19:369–73.
Cao YX, Chian RC. Fertility preservation with immature and in vitro matured oocytes. Semin Reprod Med. 2009;27(6):456–64.
Baka SG, Toth TL, Veeck LL, Jones HW Jr, Muasher SJ, Lanzendorf SE. Evaluation of the spindle apparatus of in vitro matured human oocytes following cryopreservation. Hum Reprod. 1995;10:1816–20.
Goud A, Goud P, Qian C, Van der Elst J, Van Maele G, Dhont M. Cryopreservation of human germinal vesicle stage and in vitro matured MII oocytes: influence of cryopreservation media on the survival, fertilization, and early cleavage divisions. Fertil Steril. 2000;74:487–94.
Nazari S, Khalili M, Esmaielzadeh F, Mohsenzadeh M. Maturation capacity, morphology and morphometric assessments of human immature oocytes after vitrification and in vitro maturation. Iran J Reprod Med. 2011;9:33–7.
Shahedi A, Hoseini A, Khalili MA, Norouzian M, Salehi M, Piraei, et al. The effect of vitrificationon ultrastructure of human in vitro matured germinal vesicle oocytes. Eur J Obstet Gynecol Reprod Biol. 2013;167:69–75.
Yazdanpanah F, Khalili MA, Eftekhar M, Karimi H. The effect of vitrification on maturation and viability capacities of immature human oocytes. Arch Gynecol Obstet. 2013;288(2):439–44.
Molina I, Gómez J, Balasch S, Pellicer N, Novella-Maestre E. Osmotic-shock produced by vitrification solutions improves immature human oocytes in vitro maturation. Reprod Biol Endocrinol. 2016;14(1):27.
Imesch P, Scheiner D, Xie M, Fink D, Macas E, Dubey R, et al. Developmental potential of human oocytes matured in vitro followed by vitrification and activation. J Ovarian Res. 2013;6:30.
Liu MH, Zhou WH, Chu DP, Fu L, Sha W, Li Y. Ultrastructural changes and methylation of human oocytes vitrified at the germinal vesicle stage and matured in vitro after thawing. Gynecol Obstet Investig. 2016;82(3):252–61.
Oliveira NP, Dutra CG, Frantz GN, Basso CG, Fortis MF, Frantz N. Embryos from in vitro maturation (IVM) technique can be successfully vitrified resulting in the birth of a healthy child. JBRA Assist Reprod. 2015;19(4):263–5.
Huang JY, Tulandi T, Holzer H, Tan SL, Chian RC. Combining ovarian tissue cryobanking with retrieval of immature oocytes followed by in vitro maturation and vitrification: an additional strategy of fertility preservation. Fertil Steril. 2008;89(3):567–72.
Segers I, Mateizel I, Van Moer E, Smitz J, Tournaye H, Verheyen G, et al. In vitro maturation (IVM) of oocytes recovered from ovariectomy specimens in the laboratory: a promising “ex vivo” method of oocyte cryopreservation resulting in the first report of an ongoing pregnancy in Europe. J Assist Reprod Genet. 2015;32(8):1221–31.
Yin H, Jiang H, Kristensen SG, Andersen CY. Vitrification of in vitro matured oocytes collected from surplus ovarian medulla tissue resulting from fertility preservation of ovarian cortex tissue. J Assist Reprod Genet. 2016;33(6):741–6.
Sifer C, Sellam-Chokron O, Sermondade N, Cedrin-Durnerin I, Sonigo C, Herbemont C, et al. Should metaphase 1 and 2 stages oocytes be vitrified in the same time for fertility preservation? Future Oncol. 2016;12(20):2297–305.
Sathananthan AH, Trounson AO. Effects of culture and cryopreservation on human oocyte and embryo ultrastructure and function. In: Van Blerkom J, Motta PM, editors. Ultrastructure of human gametogenesis and early embryogenesis. Boston: Kluwer Academic Publ; 1989. p. 181–99.
Wu C, Rui R, Dai J, Zhang C, Ju S, Xie B, et al. Effects of cryopreservation on the developmental competence, ultrastructure and cytoskeletal structure of porcine oocytes. Mol Reprod Dev. 2006;73:1454–62.
Fuku EJ, Liu J, Downey BR. In vitro viability and ultrastructural changes in bovine oocytes treated with a vitrification solution. Mol Reprod Dev. 1995;40(2):177–85.
Sprícigo JF, Morais K, Ferreira AR, Machado GM, Gomes AC, Rumpf R, et al. Vitrification of bovine oocytes at different meiotic stages using the Cryotop method: assessment of morphological, molecular and functional patterns. Cryobiology. 2014;69(2):256–65.
Turathum B, Saikhun K, Sangsuwan P, Kitiyanant Y. Effects of vitrification on nuclear maturation, ultrastructural changes and gene expression of canine oocytes. Reprod Biol Endocrinol. 2010;8:70.
Nottola SA, Coticchio G, Sciajno R, Gambardella A, Maione M, Scaravelli G, et al. Ultrastructural markers of quality in human mature oocytes vitrified using cryoleaf and cryoloop. Reprod BioMed Online. 2009;19(Suppl 3):17–27.
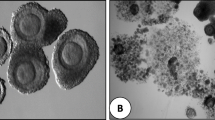
Palmerini MG, Antinori M, Maione M, Cerusico F, Versaci C, Nottola SA, et al. Ultrastructure of immature and mature human oocytes after Cryotop vitrification. J Reprod Dev. 2014;60(6):411–20.
Bianchi V, Macchiarelli G, Borini A, Lappi M, Cecconi S, Miglietta S, et al. Fine morphological assessment of quality of human mature oocytes after slow freezing or vitrification with a closed device: a comparative analysis. Reprod Biol Endocrinol. 2014;12:110.
Coticchio G, Dal Canto M, Fadini R, Mignini Renzini M, Guglielmo MC, Miglietta S, et al. Ultrastructure of human oocytes after in vitro maturation. Mol Hum Reprod. 2016;22(2):110–8.
Segovia Y, Victory N, Peinado I, García-Valverde LM, García M, Aizpurua J, et al. Ultrastructural characteristics of human oocytes vitrified before and after in vitro maturation. J Reprod Dev. 2017. doi:10.1262/jrd.2017-009.
Coticchio G, Borini A, Distratis V, Maione M, Scaravelli G, Bianchi V, Macchiarelli G, Nottola SA. Qualitative and morphometric analysis of the ultrastructure of human oocytes cryopreserved by two alternative slow cooling protocols. J Assist Reprod Genet. 2010;27(4):131–40.
Tong XH, Wu LM, Jin RT, Luo LH, Luan HB, Liu YS. Fertilization rates are improved after IVF if the corona radiata is left intact in vitrified-warmed human oocytes. Hum Reprod. 2012;27(11):3208–14.
Bianchi S, Macchiarelli G, Micara G, Linari A, Boninsegna C, Aragona C, et al. Ultrastructural markers of quality are impaired in human metaphase II aged oocytes: a comparison between reproductive and in vitro aging. J Assist Reprod Genet. 2015;32(9):1343–58.
Minasi MG, Fabozzi G, Casciani V, Ferrero S, Litwicka K, Greco E. Efficiency of slush nitrogen vitrification of human oocytes vitrified with or without cumulus cells in relation to survival rate and meiotic spindle competence. Fertil Steril. 2012;97(5):1220–5.
Tharasanit T, Colleoni S, Galli C, Colenbrander B, Stout TA. Protective effects of the cumulus-corona radiata complex during vitrification of horse oocytes. Reproduction. 2009;137(3):391–401.
Vandevoort CA, Shirley CR, Hill DL, Leibo SP. Effects of cryoprotectants and cryopreservation on germinal vesicle-stage cumulus-oocyte complexes of rhesus monkeys. Fertil Steril. 2008;90(3):805–16.
Trapphoff T, El Hajj N, Zechner U, Haaf T, Eichenlaub-Ritter U. DNA integrity, growth pattern, spindle formation, chromosomal constitution and imprinting patterns of mouse oocytes from vitrified pre-antral follicles. Hum Reprod. 2010;25(12):3025–42.
Ebrahimi B, Valojerdi MR, Eftekhari-Yazdi P, Baharvand H. Ultrastructural changes of sheep cumulus-oocyte complexes following different methods of vitrification. Zygote. 2012;20(2):103–15.
Modina S, Beretta M, Lodde V, Lauria A, Luciano AM. Cytoplasmic changes and developmental competence of bovine oocytes cryopreserved without cumulus cells. Eur J Histochem. 2004;48(4):337–46.
Auclair S, Uzbekov R, Elis S, Sanchez L, Kireev I, Lardic L, et al. Absence of cumulus cells during in vitro maturation affects lipid metabolism in bovine oocytes. Am J Physiol Endocrinol Metab. 2013;304(6):E599–613.
Tashima K, Kubo Y, Hirabayashi M, Hochi S. Downsizing cumulus cell layers to improve cryotolerance of germinal vesicle-stage bovine oocytes. Theriogenology. 2017;95:1–7.
Pennetier S, Uzbekova S, Perreau C, Papillier P, Mermillod P, Dalbie’s-Tran R. Spatio-temporal expression of the germ cell marker genes MATER, ZAR1, GDF9, BMP15, and VASA in adult bovine tissues, oocytes, and preimplantation embryos. Biol Reprod. 2004;71:1359–66.
Wu X, Viveiros MM, Eppig JJ, Bai Y, Fitzpatrick SL, Matzuk MM. Zygote arrest 1 (Zar1) is a novel maternal-effect gene critical for the oocyte-to-embryo transition. Nat Genet. 2003;33:187–91.
Tong ZB, Gold L, Pfeifer KE, Dorward H, Lee E, Bondy CA, et al. Mater, a maternal effect gene required for early embryonic development in mice. Nat Genet. 2000;26:267–8.
Hamatani T, Ko MS, Yamada M, Kuji N, Mizusawa Y, Shoji M, et al. Global gene expression profiling of preimplantation embryos. Hum Cell. 2006;19:98–117.
Dube JL, Wang P, Elvin J, Lyons KM, Celeste AJ, Matzuk MM. The bone morphogenetic protein 15 gene is X-linked and expressed in oocytes. Mol Endocrinol. 1998;12:1809–17.
Racowsky C, Kaufman ML. Nuclear degeneration and meiotic aberrations observed in human oocytes matured in vitro: analysis by light microscopy. Fertil Steril. 1992;58:750–5.
Cekleniak NA, Combelles CMH, Ganz DA, Fung J, Albertini DF, Racowsky C. A novel system for in vitro maturation of human oocytes. Fertil Steril. 2001;75:1185–93.
Palmerini MG, Nottola SA, Leoni GG, Succu S, Borshi X, Berlinguer F, et al. In vitro maturation is slowed in prepubertal lamb oocytes: ultrastructural evidences. Reprod Biol Endocrinol. 2014;12:115.
Magli MC, Ferraretti AP, Crippa A, Lappi M, Feliciani E, Gianaroli L. First meiosis errors in immature oocytes generated by stimulated cycles. Fertil Steril. 2006;86:629–35.
Nogueira D, Staessen C, Van de Velde H, Van Steirteghem A. Nuclear status and cytogenetics of embryos derived from in vitro-matured oocytes. Fertil Steril. 2000;74:295–8.
Jones GM, Cram DS, Song B, Magli MC, Gianaroli L, Lacham-Kaplan O, et al. Gene expression profiling of human oocytes following in vivo or in vitro maturation. Hum Reprod. 2008;23(5):1138–44.
Ebrahimi B, Valojerdi MR, Eftekhari-Yazdi P, Baharvand H. In vitro maturation, apoptotic gene expression and incidence of numerical chromosomal abnormalities following cryotop vitrification of sheep cumulus-oocyte complexes. J Assist Reprod Genet. 2010;27(5):239–46.
Dai JJ, Niu YF, Wu CF, Zhang SH, Zhang DF. Both death receptor and mitochondria mediated apoptotic pathways participated the occurrence of apoptosis in porcine vitrified MII stage oocytes. Cryo-Letters. 2016;37(2):129–36.
Niu Y, Dai J, Chen Y, Wu C, Zhang S, Zhang D. Positive effect of apoptotic inhibitor z-vad-fmk on vitrified-thawed porcine mii stage oocytes. Cryo-Letters. 2016;37(3):188–95.
Dhali A, Anchamparuthy V, Butler S, Pearson R, Mullarky I, Gwazdauskas F. Gene expression and development of mouse zygotes following droplet vitrification. Theriogenology. 2007;68:1292–8.
Tatemoto H, Sakurai N, Muto N. Protection of porcine oocytes against apoptotic cell death caused by oxidative stress during in vitro maturation: role of cumulus cells. Biol Reprod. 2000;63:805–10.
Spinaci M, Vallorani C, Bucci D, Tamanini C, Porcu E, Galeati G. Vitrification of pig oocytes induces changes in histone H4 acetylation and histone H3 lysine 9 methylation (H3K9). Vet Res Commun. 2012;36:165–71.
Zhao XM, Ren JJ, Du WH, Hao HS, Wang D, Qin T, et al. Effect of vitrification on promoter CpG island methylation patterns and expression levels of DNA methyltransferase 1o, histone acetyltransferase 1, and deacetylase 1 in metaphase II mouse oocytes. Fertil Steril. 2013;100:256–61.
Cheng KR, Fu XW, Zhang RN, Jia GX, Hou YP, Zhu SE. Effect of oocyte vitrification on deoxyribonucleic acid methylation of H19, Peg3, and Snrpn differentially methylated regions in mouse blastocysts. Fertil Steril. 2014;102:1183–90.
Hinck H, Smissen PVD, Heusterpreute M, Donnay I, Hertogh RD, Pampfer S. Identification of caspase 3 and caspase-activated deoxyribonuclease in rat blastocysts and their implication in the induction of chromatin degradation (but not nuclear fragmentation) by high glucose. Biol Reprod. 2001;64:555–62.
Palmerini MG, Nottola SA, Tunjung WA, Kadowaki A, Bianchi S, Cecconi S, et al. EGF-FSH supplementation reduces apoptosis of pig granulosa cells in co-culture with cumulus-oocyte complexes. Biochem Biophys Res Commun. 2016;481:159–64.
Morita Y, Perez GI, Paris F, Miranda S, Ehleiter D, Haimovitz-Friedman A, et al. Oocyte apoptosis is suppressed by disruption of the acid sphingomyelinase gene or by sphingosine-1-1phosphatetherapy. Nat Med. 2000;6:1109–14.
Anchamparuthy V, Pearson R, Gwazdauskas F. Expression pattern of apoptotic genes in vitrified-thawed bovine oocytes. Reprod Domest Anim. 2010;45:e83–90.
Shahedi A, Yeganeh F, Hosseini A, Khalili MA. Comparision of stress and apoptosis-related genes expression between vitrified and fresh human GV oocytes after in-vitro maturation. Iran J Reprod Med. 2014;12(1):29–30. Paper presented at the 20th National Congress on Infertility and Reproduction, Isfahan, Iran, 11-13 June 2014
Chian RC, Cao YX. In vitro maturation of immature human oocytes for clinical application. Methods Mol Biol. 2014;1154:271–88.
Nottola SA, Albani E, Coticchio G, Palmerini MG, Lorenzo C, Scaravelli G, et al. Freeze/thaw stress induces organelle remodeling and membrane recycling in cryopreserved human mature oocytes. J Assist Reprod Genet. 2016;33(12):1559–70.
Acknowledgements
We are very grateful to Dr. Giovanni Coticchio for his valuable comments and for critically reviewing this manuscript.
Author information
Authors and Affiliations
Contributions
MAK, AS and SA designed the study. MGP and MAK wrote the manuscript. SAN and GM critically revised the manuscript. All authors have read and approved the final version and submission of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Khalili, M.A., Shahedi, A., Ashourzadeh, S. et al. Vitrification of human immature oocytes before and after in vitro maturation: a review. J Assist Reprod Genet 34, 1413–1426 (2017). https://doi.org/10.1007/s10815-017-1005-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-1005-4