Abstract
Background
It is essential to accurately distinguish small benign hyperplastic colon polyps (HP) from sessile serrated lesions (SSL) or adenomatous polyps (TA) based on endoscopic appearances. Our objective was to determine the accuracy and inter-observer agreements for the endoscopic diagnosis of small polyps.
Methods
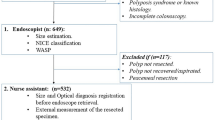
High-quality endoscopic images of 30 small HPs, SSLs, and TAs were used randomly to create two-timed PowerPoint slide sets—one with and another one without information on polyp size and location. Seven endoscopists viewed the slides on two separate occasions 90 days apart, identified the polyp type, and graded their confidence level. Overall and polyp-specific accuracies were assessed for the group and individual endoscopists. Chi-square tests and Kappa (κ) statistics were used to compare differences as appropriate.
Results
When polyp size and location were provided, overall accuracy was 67.1% for TAs, 50.0% for SSLs, and 41.4% for HPs; the corresponding accuracies were 60%, 44.3%, and 34.3% when polyp size and location were withheld (p < .001). Inter-observer agreement was moderate for TAs (κ = 0.50) and fair for SSLs (κ = 0.26) and HPs (κ = 0.29); the corresponding inter-observer agreements were 0.44, 0.31, and 0.17 with polyp size and location withheld. Accuracy was not affected by knowledge of polyp size, location, or confidence level. Endoscopists with ≥ 10 years (vs. < 10 years) of colonoscopy experience had marginally higher (56% vs. 40%, p = 0.05) accuracy for SSL diagnosis.
Conclusions
The ability to distinguish between small TAs, SSLs, and HPs on their endoscopic appearance is poor regardless of the endoscopists' knowledge of polyp size and location.

Similar content being viewed by others
References
Zauber AG, Winawer SJ, O’Brien MJ et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687–696.
Kaltenbach T, Anderson JC, Burke CA et al. Endoscopic Removal of Colorectal Lesions: Recommendations by the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2020;115:435–464.
Wang FW, Hsu PI, Chuang HY et al. Prevalence and risk factors of asymptomatic colorectal polyps in Taiwan. Gastroenterol Res Pract. 2014;2014:985205.
Spring KJ, Zhao ZZ, Karamatic R et al. High prevalence of sessile serrated adenomas with BRAF mutations: a prospective study of patients undergoing colonoscopy. Gastroenterology. 2006;131:1400–1407.
Crockett SD, Nagtegaal ID. Terminology, Molecular Features, Epidemiology, and Management of Serrated Colorectal Neoplasia. Gastroenterology. 2019;157:949–966.
Szylberg Ł, Janiczek M, Popiel A, Marszałek A. Large Bowel Genetic Background and Inflammatory Processes in Carcinogenesis-Systematic Review. Adv Clin Exp Med. 2015;24:555–563.
Myers DJ, Arora K. Villous Adenoma. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 10, 2021.
Hamilton SR, Aaltonen LA. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Digestive System. 3rd ed. IARC Press; 2000.
Rex DK, Ahnen DJ, Baron JA et al. Serrated lesions of the colorectum: review and recommendations from an expert panel. Am J Gastroenterol. 2012;107:1315–1330.
McCarthy AJ, O’Reilly SM, Shanley J et al. Colorectal Serrated Neoplasia: An Institutional 12-Year Review Highlights the Impact of a Screening Programme. Gastroenterol Res Pract. 2019;2019:1592306.
Burgess NG, Tutticci NJ, Pellise M, Bourke MJ. Sessile serrated adenomas/polyps with cytologic dysplasia: a triple threat for interval cancer. Gastrointest Endosc. 2014;80:307–310.
Kim SY, Kim TI. Serrated neoplasia pathway as an alternative route of colorectal cancer carcinogenesis. Intest Res. 2018;16:358–365.
Tadepalli US, Feihel D, Miller KM et al. A morphologic analysis of sessile serrated polyps observed during routine colonoscopy (with video). Gastrointest Endosc. 2011;74:1360–1368.
Ahadi M, Sokolova A, Brown I, Chou A, Gill AJ. The 2019 World Health Organization Classification of appendiceal, colorectal and anal canal tumours: an update and critical assessment. Pathology. 2021;53:454–461.
Yamada M, Sakamoto T, Otake Y et al. Investigating endoscopic features of sessile serrated adenomas/polyps by using narrow-band imaging with optical magnification. Gastrointest Endosc. 2015;82:108–117.
Vleugels JLA, Hazewinkel Y, Fockens P, Dekker E. Natural history of diminutive and small colorectal polyps: a systematic literature review. Gastrointest Endosc. 2017;85:1169–1176.
Rex DK, Kahi C, O’Brien M et al. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2011;73:419–422.
Yang HJ, Lee JI, Park SK et al. External Validation of the Endoscopic Features of Sessile Serrated Adenomas in Expert and Trainee Colonoscopists. Clin Endosc. 2017;50:279–286.
Olympus Medical Systems Group. (2021, March 15). FDA Clears Olympus' Narrow Band Imaging® (NBI) for Use in Assessing Colonic Lesions. CISION: PR Newswire. https://www.prnewswire.com/news-releases/fda-clears-olympus-narrow-band-imaging-nbi-for-use-in-assessing-colonic-lesions-301247362.html
Kaminski M, Hassan C, Bisschops R et al. Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2014;46:435–449.
Bhat Y, Abu Dayyeh B, Chauhan S et al. ASGE Technological Status Evaluation Report: High-definition and high-magnification endoscopes. Gastrointestinal Endoscopy. 2014;80:919–927.
Gupta N, Kaltenbach T, Sato T et al. Diagnosis time determines the accuracy of optical diagnosis of diminutive polyp histology. Gastrointest Endosc. 2013;77:AB553–AB554.
Anderson JC, Lisovsky M, Greene MA et al. Factors Associated With Classification of Hyperplastic Polyps as Sessile Serrated Adenomas/Polyps on Morphologic Review. J Clin Gastroenterol. 2018;52:524–529.
Gill P, Rafferty H, Munday D et al. Proximal colon cancer and serrated adenomas - hunting the missing 10%. Clin Med (Lond). 2013;13:557–561.
Singh H, Bay D, Ip S et al. Pathological reassessment of hyperplastic colon polyps in a city-wide pathology practice: implications for polyp surveillance recommendations. Gastrointest Endosc. 2012;76:1003–1008.
Farris AB, Misdraji J, Srivastava A et al. Sessile serrated adenoma: challenging discrimination from other serrated colonic polyps. Am J Surg Pathol. 2008;32:30–35.
Vennelaganti S, Cuatrecasas M, Vennalaganti P et al. Interobserver Agreement Among Pathologists in the Differentiation of Sessile Serrated From Hyperplastic Polyps. Gastroenterology. 2021;160:452–454.
Turner JK, Williams GT, Morgan M, Wright M, Dolwani S. Interobserver agreement in the reporting of colorectal polyp pathology among bowel cancer screening pathologists in Wales. Histopathology. 2013;62:916–924.
Hazewinkel Y, López-Cerón M, East JE et al. Endoscopic features of sessile serrated adenomas: validation by international experts using high-resolution white-light endoscopy and narrow-band imaging. Gastrointest Endosc. 2013;77:916–924.
Pereyra L, Gómez EJ, González R et al. Finding sessile serrated adenomas: is it possible to identify them during conventional colonoscopy? Dig Dis Sci. 2014;59:3021–3026.
Ijspeert JE, Bastiaansen BA, van Leerdam ME et al. Development and validation of the WASP classification system for optical diagnosis of adenomas, hyperplastic polyps and sessile serrated adenomas/polyps. J. Gut. 2016;65:963–970.
Maratt JK, Dickens J, Schoenfeld PS et al. Factors Associated with Surveillance Adenoma and Sessile Serrated Polyp Detection Rates. Dig Dis Sci. 2017;62:3579–3585.
Telford J, Gondara L, Pi S, Gentile L, Enns R. Higher adenoma detection, sessile serrated lesion detection and proximal sessile serrated lesion detection are associated with physician specialty and performance on Direct Observation of Procedural Skills. BMJ Open Gastroenterol. 2021;8:e000677.
Sarvepalli S, Garber A, Rothberg MB et al. Association of Adenoma and Proximal Sessile Serrated Polyp Detection Rate, s With Endoscopist. JAMA Surg. 2019;154:627–635.
Rex DK. Narrow-band imaging without optical magnification for histologic analysis of colorectal polyps. Gastroenterology. 2009;136:1174–1181.
Uraoka T, Higashi R, Horii J et al. Prospective evaluation of endoscopic criteria characteristic of sessile serrated adenomas/polyps. J Gastroenterol. 2015;50:555–563.
Vleugels JLA, Dijkgraaf MGW, Hazewinkel Y et al. Effects of Training and Feedback on Accuracy of Predicting Rectosigmoid Neoplastic Lesions and Selection of Surveillance Intervals by Endoscopists Performing Optical Diagnosis of Diminutive Polyps. Gastroenterology. 2018;154:1682–1693.
Funding
There are no financial disclosures.
Author information
Authors and Affiliations
Contributions
Planning the study: TK, AA, PT. Conducting the study: TK, AA. Collecting data: TK, AA. Interpreting data: TK, AA, FL, PT. Drafting the manuscript: TK. Revising the manuscript: TK, AA, SK, BC, MH, MH, AM, AR, EZ, PT. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
None declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An editorial commenting on this article is available at https://doi.org/10.1007/s10620-022-07645-y.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khuc, T., Agarwal, A., Li, F. et al. Accuracy and Inter-observer Agreement Among Endoscopists for Visual Identification of Colorectal Polyps Using Endoscopy Images. Dig Dis Sci 68, 616–622 (2023). https://doi.org/10.1007/s10620-022-07643-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07643-0