Abstract
Background and Aims
Lower urinary tract symptoms (LUTS) are frequently reported by constipated patients. Prospective studies investigating the association between defecatory disorders (DDs) and voiding dysfunction, predominantly in women, have reported conflicting results. This study investigated (1) the prevalence of LUTS in young men with DDs and (2) the association between objectively documented DDs and voiding dysfunction in constipated young men with LUTS.
Methods
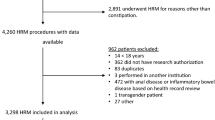
We reviewed the medical records, including validated questionnaires, of men aged 18–40 with confirmed DDs treated with pelvic floor physical therapy (PT) at our institution from May 2018 to November 2020. In a separate group of constipated young men with LUTS who underwent high-resolution anorectal manometry (HRM), rectal balloon expulsion test (BET), and uroflowmetry, we explored the relationship between DDs and voiding dysfunction.
Results
A total of 72 men were evaluated in the study. Among 43 men receiving PT for a proven DD, 82% reported ≥ 1 LUTS, most commonly frequent urination. Over half of these men experienced a reduction in LUTS severity after bowel-directed pelvic floor PT. Among 29 constipated men with LUTS who had undergone HRM/BET and uroflowmetry, 28% had concurrent defecatory and voiding dysfunction, 10% had DD alone, 14% had only voiding dysfunction, and 48% had neither. The presence of DD was associated with significantly increased odds of concurrent voiding dysfunction (odds ratio 9.3 [95% CI 1.7–52.7]).
Conclusions
Most young men with DDs experience LUTS, which may respond to bowel-directed physical therapy. Patients with DD and urinary symptoms have increased odds of voiding dysfunction.


Similar content being viewed by others
Abbreviations
- BET:
-
Balloon expulsion test
- CRADI-8:
-
Colorectal-Anal Distress Inventory 8
- DD:
-
Defecatory disorder
- HRM:
-
High-resolution anorectal manometry
- IQR:
-
Interquartile range
- LUTS:
-
Lower urinary tract symptoms
- OR:
-
Odds ratio
- PFIQ-7:
-
Pelvic Floor Impact Questionnaire
- PVR:
-
Post-void residual
- Qmax:
-
Maximum urine flow rate
- STROBE:
-
Strengthening the reporting of observational studies in epidemiology
- UDI-6:
-
Urinary Distress Inventory, Short Form
- UIQ-7:
-
Urinary Impact Questionnaire
References
Thurmon KL, Breyer BN, Erickson BA. Association of bowel habits with lower urinary tract symptoms in men: findings from the 2005–2006 and 2007–2008 National Health and Nutrition Examination Survey. J Urol 2013;189:1409–1414.
Coyne KS, Cash B, Kopp Z et al. The prevalence of chronic constipation and faecal incontinence among men and women with symptoms of overactive bladder. BJU Int 2011;107:254–261.
Hill WG. Control of urinary drainage and voiding. Clin J Am Soc Nephrol 2015;10:480–492.
Bharucha AE. Pelvic floor: anatomy and function. Neurogastroenterol Motil 2006;18:507–519.
Salducci J, Planche D, Naudy B. Physiological role of the internal anal sphincter and the external anal sphincter during micturition. In: Wienbeck M, ed. New York: Raven Press; 1982; 513–520.
Rao SSC, Bharucha AE, Chiarioni G et al. Anorectal Disorders. Gastroenterology 2016;150:1430-1442.e4.
Abrams P, Cardozo L, Fall M et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 2002;21:167–178.
Groutz A, Blaivas JG, Pies C, Sassone AM. Learned voiding dysfunction (non-neurogenic, neurogenic bladder) among adults. Neurourol Urodyn 2001;20:259–268.
Bannister JJ, Lawrence WT, Smith A, Thomas DG, Read NW. Urological abnormalities in young women with severe constipation. Gut 1988;29:17–20.
Thorpe AC, Williams NS, Badenoch DF, Blandy JP, Grahn MF. Simultaneous dynamic electromyographic proctography and cystometrography. Br J Surg 1993;80:115–120.
Klingele CJ, Lightner DJ, Fletcher JG, Gebhart JB, Bharucha AE. Dysfunctional urinary voiding in women with functional defecatory disorders. Neurogastroenterol Motil 2010;22:1094-e284.
von Elm E, Altman DG, Egger M et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–9.
Longstreth GF, Thompson WG, Chey WD et al. Functional bowel disorders. Gastroenterology 2006;130:1480–91.
Bharucha AE, Wald A, Enck P, Rao S. Functional anorectal disorders. Gastroenterology 2006;130:1510–8.
Barber MD, Kuchibhatla MN, Pieper CF, Bump RC. Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 2001;185:1388–95.
Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence impact questionnaire and the urogenital distress inventory. continence program for women research group. Neurourol Urodyn 1995;14:131–9.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 2005;193:103–13.
Barber MD, Spino C, Janz NK et al. The minimum important differences for the urinary scales of the pelvic floor distress inventory and pelvic floor impact questionnaire. Am J Obstet Gynecol 2009;200:e1-7.
Lee TH, Bharucha AE. How to perform and Interpret a High-resolution anorectal manometry test. J Neurogastroenterol Motil 2016;22:46–59.
Oblizajek NR, Gandhi S, Sharma M et al. Anorectal pressures measured with high-resolution manometry in healthy people-Normal values and asymptomatic pelvic floor dysfunction. Neurogastroenterol Motil 2019;31:e13597.
Chedid V, Vijayvargiya P, Halawi H, Park SY, Camilleri M. Audit of the diagnosis of rectal evacuation disorders in chronic constipation. Neurogastroenterol Motil 2019;31:e13510.
Minguez M, Herreros B, Sanchiz V et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology 2004;126:57–62.
Ratuapli S, Bharucha AE, Harvey D, Zinsmeister AR. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterol Motil 2013;25:e813-20.
Schafer W, Abrams P, Liao L et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 2002;21:261–74.
Haylen BT, Ashby D, Sutherst JR, Frazer MI, West CR. Maximum and average urine flow rates in normal male and female populations–the Liverpool nomograms. Br J Urol 1989;64:30–8.
Nitti VW. Pressure flow urodynamic studies: the gold standard for diagnosing bladder outlet obstruction. Rev Urol 2005;7:S14-21.
Kaplan SA, Ikeguchi EF, Santarosa RP et al. Etiology of voiding dysfunction in men less than 50 years of age. Urology 1996;47:836–9.
Nitti VW, Lefkowitz G, Ficazzola M, Dixon CM. Lower urinary tract symptoms in young men: videourodynamic findings and correlation with noninvasive measures. J Urol 2002;168:135–8.
Devreese AM, Nuyens G, Staes F et al. Do posture and straining influence urinary-flow parameters in normal women? Neurourol Urodynam 2000;19:3–8.
Cobreros C, Garcia Penela E, del Villar M et al. Low Urinary Obstructed Patients do not use Valsalva Maneuvre to Improve their Voiding Phase: Urodynamic Proof. In: International Continence Society. 2016.
Burgio KL, Engel BT, Quilter RE, Arena VC. The relationship between external anal and external urethral sphincter activity in continent women. Neurourology and Urodynamics 1991;10:555–562.
Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology 2006;130:657–64.
Liaw Y-M, Kuo H-C. Biofeedback pelvic floor muscle training for voiding dysfunction and overactive bladder. Incont Pelvic Floor Dysfunct 2007;1:13–15.
Oelrich TM. The urethral sphincter muscle in the male. Am J Anat 1980;158:229–46.
Oelrich TM. The striated urogenital sphincter muscle in the female. Anat Rec 1983;205:223–32.
Funding
None.
Author information
Authors and Affiliations
Contributions
BA White: Data curation, formal analysis, and writing (original draft). BJ Linder: Conceptualization, methodology, and writing (review & editing). LA Szarka: Conceptualization, methodology, and writing (review & editing). DO Prichard: Conceptualization, formal analysis, methodology, supervision, and writing (original draft, review & editing).
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
White, B.A., Linder, B.J., Szarka, L.A. et al. Urinary Symptoms and Bladder Voiding Dysfunction Are Common in Young Men with Defecatory Disorders: A Retrospective Evaluation. Dig Dis Sci 67, 3036–3044 (2022). https://doi.org/10.1007/s10620-021-07167-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07167-z