Abstract
Purpose of Review
Defecatory dysfunction is infrequently considered a gynaecological problem. However, obstructed defecation (OD) more commonly affects women than men and is associated with pelvic floor dysfunction. Therefore, we set out to write a review from a urogynaecologists’ prospective focusing on OD as it relates to the pelvic floor.
Recent Findings
Literature on this topic remains sparse and the studies tend to have a low sample size. It is clear that OD is associated with pelvic floor dysfunction including urinary incontinence and structural dysfunction; however, it is less clear which is the primary pathology. Management of OD needs to be considered in treatment of pelvic floor dysfunctions.
Summary
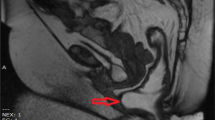
OD effects 14% of the general population. Ninety percent of the patients with OD will have a rectocele, enterocele or even intussusception. The pathophysiology is multifactorial and still not fully comprehended. Aetiology of constipation is classified as primary or secondary. The former includes slow transit or normal constipation and defecation disorders. The latter includes constipation caused by medications, diet and medical conditions. The Rome IV criteria are used to define functional constipation globally. Defecation disorders of the pelvic floor are categorised as structural disorders, pudendal neuropathy and dyssynergic defecation. First-line management includes treating the primary causes, dietary modification and laxatives. We stress the importance of posture whilst defecating is of utmost importance. A full squatting position with a slight forward tilt results in the broadening of the anorectal angle thereby facilitating emptying. Biofeedback therapy is still considered first-line treatment for dyssynergic defecation. Finally, surgical management of advanced stage prolapse is often unavoidable but is not a cure of OD. The increasing use of translabial ultrasound as a diagnostic modality will hopefully help facilitate research in this area.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Enck P, Leinert J, Smid M, Köhler T, Schwille-Kiuntke J. Prevalence of constipation in the German population—a representative survey (GECCO). United European Gastroenterol J. 2016;4(3):429–37. A population study that discusses prevalence of constipation and its impact on quality of life.
WALD A, SCARPIGNATO C, MUELLER-LISSNER S, KAMM MA, HINKEL U, HELFRICH I, et al. A multinational survey of prevalence and patterns of laxative use among adults with self-defined constipation. Aliment Pharmacol Ther. Blackwell Publishing Ltd. 2008;2(Suppl. 7):1095–14.
Berghmans B, Nieman F, Leue C, Weemhoff M, Breukink S, van Koeveringe G. Prevalence and triage of first-contact complaints on pelvic floor dysfunctions in female patients at a Pelvic Care Centre. Neurourol Urodyn. 2015;35(4):503–8.
• Podzemny V. Management of obstructed defecation. WJG. 2015;21(4):1053–9. Provides overview of management for obstructed defecation and highlights its presentation as pelvic organ prolapse to be the iceberg syndrome.
Raizada V, Mittal RK. Pelvic floor anatomy and applied physiology. Gastroenterol Clin N Am. 2008;37(3):493–509. vii
Hicks CW, Weinstein M, Wakamatsu M, Pulliam S, Savitt L, Bordeianou L. Are rectoceles the cause or the result of obstructed defaecation syndrome? A prospective anorectal physiology study. Color Dis. 2013;15(8):993–9.
Amselem C, Puigdollers A, Azpiroz F, Sala C, Videla S, Ndez-Fraga XF, et al. Constipation: a potential cause of pelvic floor damage? Neurogastroenterology & Motility. 2010;22(2):150–e48.
Bove A. Consensus statement AIGO/SICCR diagnosis and treatment of chronic constipation and obstructed defecation (part II: treatment). WJG. 2012;18(36):4994–20.
DeLancey JO. Structural anatomy of the posterior pelvic compartment as it relates to rectocele. Am J Obstet Gynecol. 1999;180(4):815–23.
Tamilselvi A, Rane A. In: Tamilselvi A, Rane A, editors. Principles and practice of urogynaecology. New Delhi: Springer; 2015. 1 p.
Palit S, Lunniss PJ, Scott SM. The physiology of human defecation. Dig Dis Sci. 2012;57(6):1445–64.
Stricker C. Physiology of defecation and mechanisms of constipation. 2017. pp. 1–28.
Andrews CN, Storr M. The pathophysiology of chronic constipation. Can J Gastroenterol. 2011;25(Suppl B):16B–21B.
Bush M, Petros P, Swash M, Fernandez M, Gunnemann A. Defecation 2: internal anorectal resistance is a critical factor in defecatory disorders. Tech Coloproctol Springer Milan. 2012;16(6):445–50.
Bove A. Consensus statement AIGO/SICCR: diagnosis and treatment of chronic constipation and obstructed defecation (part I: diagnosis). WJG. 2012;18(14):1555–10.
Soligo M, Salvatore S, Emmanuel AV, De Ponti E, Zoccatelli M, Cortese M, et al. Patterns of constipation in urogynecology: clinical importance and pathophysiologic insights. Am J Obstet Gynecol Elsevier. 2006;195(1):50–5.
Simren M, Palsson OS, Whitehead WE. Update on Rome IV criteria for colorectal disorders: implications for clinical practice. Current Gastroenterology Reports. Springer US. 2017;19(4):1257.
Schmulson MJ, Drossman DA. What is new in Rome IV. J Neurogastroenterol Motil. 2017;23(2):151–63.
Pescatori M, Spyrou M, Pulvirenti d'Urso A. A prospective evaluation of occult disorders in obstructed defecation using the ‘iceberg diagram’. Color Dis. 2007;9(5):452–6.
Vaccaro CA, Cheong DM, Wexner SD, Nogueras JJ, Salanga VD, Hanson MR, et al. Pudendal neuropathy in evacuatory disorders. Dis Colon rectum. 1995;38(2):166–71.
Vaccaro CA, Wexner SD, Teoh TA, Choi SK, Cheong DM, Salanga VD. Pudendal neuropathy is not related to physiologic pelvic outlet obstruction. Dis Colon rectum. 1995;38(6):630–4.
Baek HN, Hwang YH, Jung YH. Clinical significance of perineal descent in pelvic outlet obstruction diagnosed by using defecography. J Korean Soc Coloproctol. 2010;26(6):395–401.
Rao SSC, Valestin J, Brown CK, Zimmerman B, Schulze K. Long-term efficacy of biofeedback therapy for dyssynergic defecation: randomized controlled trial. Am J Gastroenterol. Nature Publishing Group. 2010;105(4):890–6.
Rao SSC, Patcharatrakul T. Diagnosis and treatment of dyssynergic defecation. J Neurogastroenterol Motil. 2016;22(3):423–35.
Rao SSC, Kavlock R, Rao S. Influence of body position and stool characteristics on defecation in humans. Am J Gastroenterol. 2006;101(12):2790–6.
Coyne KS, Cash B, Kopp Z, Gelhorn H, Milsom I, Berriman S, et al. The prevalence of chronic constipation and faecal incontinence among men and women with symptoms of overactive bladder. BJU Int. 2011;107(2):254–61.
Wyndaele M, De Winter BY, Pelckmans P, Wyndaele JJ. Lower bowel function in urinary incontinent women, urinary continent women and in controls. Neurourol Urodyn. Wiley Subscription Services, Inc., A Wiley Company. 2011;30(1):138–43.
Maeda T, Tomita M, Nakazawa A, Sakai G, Funakoshi S, Komatsuda A, et al. Female functional constipation is associated with overactive bladder symptoms and urinary incontinence. Biomed Res Int. Hindawi Publishing Corporation. 2017;2017(2):2138073–5.
Spence-Jones C, KAMM MA, Henry MM, Hudson CN. Bowel dysfunction: a pathogenic factor in uterovaginal prolapse and urinary stress incontinence. Br J Obstet Gynaecol. 1994;101(2):147–52.
Charach G, Greenstein A, Rabinovich P, Groskopf I, Weintraub M. Alleviating constipation in the elderly improves lower urinary tract symptoms. Gerontology. 2001;47(2):72–6.
Stone DE, Quiroz LH. Ultrasound imaging of the pelvic floor. Obstet Gynecol Clin N Am. 2016;43(1):141–53.
Dietz HP, Beer GM. Ultrasound in the investigation of posterior compartment vaginal prolapse and obstructed defecation. Ultrasound Obstet Gynecol. John Wiley & Sons, Ltd. 2012;40(1):14–27.
Martellucci J, Naldini G. Clinical relevance of transperineal ultrasound compared with evacuation proctography for the evaluation of patients with obstructed defaecation. Color Dis. 2011;13(10):1167–72.
Takano S, Sands DR. Influence of body posture on defecation: a prospective study of “‘the thinker’” position. Tech Coloproctol. Springer Milan. 2015;20(2):117–21.
Sikirov D. Comparison of straining during defecation in three positions: results and implications for human health. Dig Dis Sci. 2003;48(7):1201–5.
Shafik A, El-Sibai O. Study of the levator ani muscle in the multipara: role of levator dysfunction in defecation disorders. J Obstet Gynaecol. 2002;22(2):187–92.
• Iyer J, Rane A. Effects of posture and squatting on the dynamics of micturition: response to Bush and Liedl. Int Urogynecol J. 2015;26(5):781–1. Highlights the effect of posture and squatting on both micturition and defecation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sapna Dilgir declares no conflict of interest.
Ajay Rane is the chairman of and has a patent for Duneze.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Urogynecology
Rights and permissions
About this article
Cite this article
Rane, A., Dilgir, S. Defecatory Dysfunction and the Pelvic Floor. Curr Obstet Gynecol Rep 6, 237–242 (2017). https://doi.org/10.1007/s13669-017-0218-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-017-0218-y