Abstract
Background
In constipated individuals, high-resolution anorectal manometry (HRM) may suggest the presence of a defecatory disorder. Despite known physiological differences between men and women, our understanding of functional anorectal pathophysiology is based upon predominantly female cohorts. Results are generalized to men.
Aims
To evaluate whether recto-anal pressure patterns in constipated men are similar to those in constipated women.
Methods
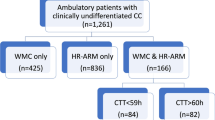
The electronic health records at Mayo Clinic, Rochester were used to identify constipated adult patients, without organic anorectal disease, who had undergone HRM and balloon expulsion testing (BET) in 2018, 2019, and 2020. Comparative analyses were performed.
Results
Among 3,298 constipated adult patients (2,633 women, 665 men), anal and rectal pressures were higher in men. Women more likely to have HRM findings suggestive of a defecatory disorder (39% versus 20%, P < 0.001). Women were more likely to exhibit a type 4 pattern (27% versus 14%, P < 0.001), and less likely to exhibit a type 1 pattern (14% versus 38%, P < 0.001), of dyssynergia. Men were more likely to have an abnormal balloon expulsion test (BET, 34% versus 29%, P = 0.006). Nominal logistic regression demonstrates that male sex, age over 50 years, reduced recto-anal gradient during simulated evacuation, and types 2 and 4 dyssynergia are associated with an abnormal BET.
Conclusions
In this large retrospective study, constipated men and women exhibited different patterns of dyssynergia both in the presence and absence of an abnormal BET. These findings were independent of sex-specific baseline physiological differences.

Similar content being viewed by others
Abbreviations
- BET:
-
Balloon expulsion test
- HRM:
-
High-resolution anorectal manometry
- OR:
-
Odds Ratio
- RAG:
-
Rectoanal gradient
- RST:
-
Rectal sensory testing
References
Rao SS. Dyssynergic defecation and biofeedback therapy. Gastroenterol Clin North Am 2008; 37(3):569–86, viii
Bharucha AE et al. American Gastroenterological Association medical position statement on constipation. Gastroenterology 2013;144:211–217.
Rao SSC et al. Anorectal disorders. Gastroenterology 2016;150:1430-1442.e4.
Wald A et al. ACG clinical guidelines: management of benign anorectal disorders. Am J Gastroenterol 2021;116:1987–2008.
Noelting J et al. The incidence rate and characteristics of clinically diagnosed defecatory disorders in the community. Neurogastroenterol Motil 2016;28:1690–1697.
Shin A et al. Interpretation of overall colonic transit in defecation disorders in males and females. Neurogastroenterol Motil 2013;25:502–508.
Ratuapli SK et al. Phenotypic identification and classification of functional defecatory disorders using high-resolution anorectal manometry. Gastroenterology 2013;144:314-322.e2.
Rao SS et al. Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus). Neurogastroenterol Motil 2004;16:589–596.
Minguez M et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology 2004;126:57–62.
Rao SSC et al. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Clin Gastroenterol Hepatol 2007;5:331–338.
Rao SSC et al. Home-based versus office-based biofeedback therapy for constipation with dyssynergic defecation: a randomised controlled trial. Lancet Gastroenterol Hepatol 2018;3:768–777.
Heymen S et al. Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type constipation. Dis Colon Rectum 2007;50:428–441.
Chiarioni G et al. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology 2006;130:657–664.
Chiarioni G, Salandini L, Whitehead WE. Biofeedback benefits only patients with outlet dysfunction, not patients with isolated slow transit constipation. Gastroenterology 2005;129:86–97.
Oblizajek NR et al. Anorectal pressures measured with high-resolution manometry in healthy people-Normal values and asymptomatic pelvic floor dysfunction. Neurogastroenterol Motil 2019;31:e13597.
Gundling F et al. Influence of gender and age on anorectal function: normal values from anorectal manometry in a large caucasian population. Digestion 2010;81:207–213.
Carrington EV et al. Traditional measures of normal anal sphincter function using high-resolution anorectal manometry (HRAM) in 115 healthy volunteers. Neurogastroenterol Motil 2014;26:625–635.
Tirumanisetty P et al. Normal values for assessment of anal sphincter morphology, anorectal motion, and pelvic organ prolapse with MRI in healthy women. Neurogastroenterol Motil 2018;30:e13314.
Skomorowska E, Hegedüs V. Sex differences in anorectal angle and perineal descent. Gastrointest Radiol 1987;12:353–355.
Feuerhak K et al. Sex differences in anorectal pressures and mechanisms of defecation in healthy people. Gastroenterology 2017;152:S318–S319.
McCrea GL et al. A review of the literature on gender and age differences in the prevalence and characteristics of constipation in North America. J Pain Symptom Manag 2009;37:737–745.
Jutras G et al. Do age and sex influence anorectal manometry parameters? J Can Assoc Gastroenterol 2021;4:235–241.
Zakari M et al. Gender differences in chronic constipation on anorectal motility. Neurogastroenterol Motil 2017;29:e12980.
White BA et al. Urinary Symptoms and bladder voiding dysfunction are common in young men with defecatory disorders: a retrospective evaluation. Dig Dis Sci 2021;8:3.
von Elm E et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453–1457.
Lee TH, Bharucha AE. How to perform and interpret a high-resolution anorectal manometry test. J Neurogastroenterol Motil 2016;22:46.
Chen SY, Feng Z, Yi X. A general introduction to adjustment for multiple comparisons. J Thorac Dis 2017;9:1725–1729.
Bharucha AE, Pemberton JH, Locke GR 3rd. American Gastroenterological Association technical review on constipation. Gastroenterology 2013;144:218–238.
Grossi U et al. Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut 2016;65:447–455.
Patcharatrakul T et al. Factors associated with response to biofeedback therapy for dyssynergic defecation. Clin Gastroenterol Hepatol 2018;16:715–721.
Banasiuk, M., et al., Comparison of Anorectal Function as Measured with High-Resolution and High-Definition Anorectal Manometry. Dig Dis, 2021.
Suares NC, Ford AC. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol 2011;106:1582–91 (quiz 1581).
Choung RS et al. Cumulative incidence of chronic constipation: a population-based study 1988–2003. Aliment Pharmacol Ther 2007;26:1521–1528.
Shim LS et al. Predictors of outcome of anorectal biofeedback therapy in patients with constipation. Aliment Pharmacol Ther 2011;33:1245–1251.
Gilliland R et al. Outcome and predictors of success of biofeedback for constipation. Br J Surg 1997;84:1123–1126.
Andrianjafy C et al. Three-dimensional high-resolution anorectal manometry can predict response to biofeedback therapy in defecation disorders. Int J Colorectal Dis 2019;34:1131–1140.
Byrne CM et al. Biofeedback for fecal incontinence: short-term outcomes of 513 consecutive patients and predictors of successful treatment. Dis Colon Rectum 2007;50:417–427.
Ratuapli S et al. Comparison of rectal balloon expulsion test in seated and left lateral positions. Neurogastroenterol Motil 2013;25:e813–e820.
Prichard D et al. Relationship among anal sphincter injury, patulous anal canal, and anal pressures in patients with anorectal disorders. Clin Gastroenterol Hepatol 2015;13:1793-1800.e1.
Acknowledgments
The authors would like to acknowledge the assistance of the AGILE team in extracting the data for this research.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Prichard, D.O., Fetzer, J. Recto-anal Pressures in Constipated Men and Women Undergoing High-Resolution Anorectal Manometry. Dig Dis Sci 68, 922–930 (2023). https://doi.org/10.1007/s10620-022-07590-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07590-w