Abstract
It is well established that innervation is one of the updated hallmarks of cancer and that psychological stress promotes the initiation and progression of cancer. The breast tumor environment includes not only fibroblasts, adipocytes, endothelial cells, and lymphocytes but also neurons, which is increasingly discovered important in breast cancer progression. Peripheral nerves, especially sympathetic, parasympathetic, and sensory nerves, have been reported to play important but different roles in breast cancer. However, their roles in the breast cancer progression and treatment are still controversial. In addition, the brain is one of the favorite sites of breast cancer metastasis. In this review, we first summarize the innervation of breast cancer and its mechanism in regulating cancer growth and metastasis. Next, we summarize the neural-related molecular markers in breast cancer diagnosis and treatment. In addition, we review drugs and emerging technologies used to block the interactions between nerves and breast cancer. Finally, we discuss future research directions in this field. In conclusion, the further research in breast cancer and its interactions with innervated neurons or neurotransmitters is promising in the clinical management of breast cancer.
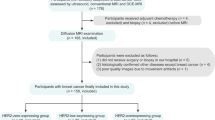
Similar content being viewed by others
1 Introduction
Breast cancer is currently one of the leading cancer types worldwide [1, 2]. Despite the improvement in therapeutic strategies, approximately 35% of patients experience recurrence, metastasis, and drug resistance [3]. Neuro-oncology plays important roles in the progression of various tumors, including breast cancer [4]. Approximately 20% of cancer patients eventually develop brain metastases [5, 6]. In tumor microenvironment, innervation and perineural invasion have recently been identified as one of the latest hallmarks of tumors [7]. Tumor innervation refers to breast tumor parenchyma infiltrated by sympathetic, parasympathetic, and sensory nerves and perineural invasion refers to tumor cell growth and invasion along the neural fibers. A study of 369 breast cancer patients with primary invasive ductal carcinoma showed that 28% of cases had nerve invasion, according to the isolated nerve fibers or axons [8].
Nerves within tumors, also called perineural infiltration or innervation, play an important role in solid and hematological malignancies [9,10,11]. In the solid tumor microenvironment, nerve fibers usually originate from the peripheral nervous system [12, 13]. Tumor innervation is associated with the progression of multiple tumors [14], including breast cancer [15, 16]. It has been demonstrated that nerves promote breast cancer tumorigenesis and that innervation is associated with a poor prognosis (overall and disease-free survival) [17].
The innervation of tumors is mainly derived from the autonomic nervous system, including sympathetic, parasympathetic, and sensory nerves. It is well known that the sympathetic and parasympathetic/vagal nerves control the function of almost any organ, maintaining systemic homeostasis under physiological conditions [18]. The autonomic nervous system plays an important role in the regulation of cancer cell proliferation, differentiation, apoptosis, migration, and invasion [19].
In this review, we focus mainly on the innervation of breast cancer, aiming to review the role and functional mechanisms of nerves in breast cancer progression and brain metastasis. A more comprehensive understanding of the role of innervations in breast tumors will provide promising therapeutic strategies for breast cancer.
2 Nerve distribution in the breast (cancer)
2.1 Nerve system in normal breast tissues
The human breast is a modified cutaneous exocrine gland consisting of skin and subcutaneous tissue, breast parenchyma (ducts and lobules), and a supporting matrix that includes fat and lymphatic vessels inserted in a complex network of ligaments, including nerves, arteries, and veins [20].
Breasts are innervated by sympathetic and sensory fibers from the 4th–6th thoracic nerves [21]. Scientists have examined the mammary gland innervation in rabbits via anatomical, electrophysiological, and histochemical staining of catecholamine and cholinesterase, which mainly reflect sympathetic adrenergic fibers. Sympathetic nerves were observed to innervate the papillary smooth muscle and were present between the media and adventitia of all arteries, without supplying any glandular tissue. In addition, butyrylcholinesterase (bChE)-containing nerve fibers, but not acetylcholinesterase (AChE)-containing nerve fibers, also innervate blood vessels and papillae. The distribution of adrenergic fibers in the papilla and blood vessels is closely correlated with the distribution of bChE-containing fibers, suggesting that a large proportion of the latter is sympathetically derived. Most mammary nerves follow arteries and arterioles. In addition, some sensory nerve fibers leave the arterial network and are located near the walls of the mammary ducts to sense milk pressure (Fig. 1). Currently, there is no evidence of a neural supply for secretory cells or myoepithelial cells or of an innervated sphincter at the duct orifice [22]. In contrast, numerous adrenergic and sensory nerves exist surrounding mammary glands.
2.2 Different roles of sympathetic, parasympathetic, and sensory nerves in breast cancer
Sympathetic and parasympathetic innervations have distinct roles in breast cancer. Sympathetic nerves promote breast cancer progression. The parasympathetic and vagus nerves have tumor-suppressive effects on breast cancer. In a human breast cancer mouse xenograft model and a carcinogen-induced mammary tumor model, breast cancer growth was accelerated after stimulation of sympathetic nerves in the tumor but decreased after stimulation of parasympathetic nerves [16]. Consistently, a retrospective analysis of breast cancer specimens from 29 patients showed that increased sympathetic nerve density and decreased parasympathetic nerve density in tumors were associated with poor clinical outcomes [23]. These neural functions are attribute to β-adrenergic or muscarinic receptors (one type of cholinergic receptor, Chrm1), as well as the tumor microenvironment, and include angiogenesis, tumor-associated macrophages, and adaptive antitumor immunoresponses [24]. α-Adrenergic or β-adrenergic receptor blockers showed tumor-specific denervation, inhibited tumor growth, and downregulated immune checkpoint molecules (programmed death 1 (PD-1), programmed death ligand 1 (PD-L1), and FOXP3), while tumor parasympathetic innervation decreased PD-1 and PD-L1 expression [16].
Additionally, sensory nerves are involved in the tumorigenesis and metastasis of breast cancer. When the brain metastatic breast cancer cells (4TBM) were injected into the mammary pads of BALB/c mice, olvanil, a TRPV1 agonist, activated sensory nerves and significantly inhibited lung and liver metastasis. This process was mainly achieved through enhancement of CD8 + T cell recruitment and increasing IFN-γ responses to irradiated cancer cells by effectively consuming sensory neuropeptides [25]. However, some studies have reported that sensory nerves promote tumorigenesis and metastasis. Co-injection of sensory neurons isolated from the dorsal root ganglia (DRG) of adult female mice with human triple-negative breast cancer (TNBC) cells increased the incidence of lung metastases in immunocompromised mice [26]. These contradictory findings may be explained by the systemic sensory fiber activation due to postnerve injury or the local heterogeneity of sensory fibers. However, when the aggressiveness and inflammatory response increase, the protective role of sensory nerve fibers becomes apparent due to the neuroimmune response. Hence, sympathetic, parasympathetic, and sensory nerves play different roles in breast tumor progression (Table 1).
2.3 Innervation differs in breast cancer subtypes
The expression of adrenergic receptors and gamma-aminobutyric acid (GABA) receptors is different in breast cancer subtypes. β-Adrenergic receptor 2 is highly expressed in the luminal A and human epidermal growth factor receptor 2 (HER2) + /estrogen receptor (ER) − subtypes of breast cancer [27, 28]. β-Blockers were found to be associated with a favorable prognosis and improved trastuzumab benefit in patients with HER2-positive early-stage breast cancer [29]. Consistently, β-blockers, such as propranolol, inhibited breast cancer growth and enhanced HER2 therapy sensitivity in preclinical mouse models [27, 30].
Moreover, nerve genes are usually upregulated in TNBC compared with levels in non-TNBC according to The Cancer Genome Atlas (TCGA) database [31]. The pi subunit of the GABA-A receptor (GABRP), GABA transporters, and glutamate decarboxylase (GAD) expression were detected in the normal mammary gland [32]. GAD is the enzyme responsible for catalyzing the synthesis of GABA. GABRP was reported to be highly expressed in the basal-like breast cancer (BLBC) subtype and correlated with poorer outcomes [33], especially breast cancer brain metastasis (BCBM). Depletion of GABRP reduced tumorigenic potential and migration in vitro. Mechanistically, GABRP silencing decreased the phosphorylation of extracellular signal–regulated kinase 1/2 (ERK1/2) [33]. Furthermore, GABA enhances the function of aldehyde dehydrogenase (ALDH)1A3, a cancer stem cell (CSC) marker in TNBC [34]. In mice harboring MDA-MB-231 tumors overexpressing ALDH1A3, GABA treatment increased breast cancer metastasis [34]. In addition, breast cancer patient datasets from TCGA, Molecular Taxonomy of Breast Cancer International Consortium (METABRIC), and the Gene Expression Omnibus (GEO) support the co-expression of ALDH1A3 and GABA pathway genes and the corresponding increased risk of metastasis [34].
3 Interaction between nerves and breast cancer cells
3.1 Innervation promotes breast cancer progression
The neuro-malignancy-promoting circuit is initiated by cancer cells that release axonal neurotrophic axonal factors, which directly link the tumor stroma to the peripheral nervous system (PNS) (Fig. 2). In return, nerve endings in the tumor microenvironment (which can be of adrenergic, cholinergic, or sensory original nerves) release neurotransmitters that stimulate corresponding receptors in stromal cells, immune cells, and cancer cells, thereby modulating cancer growth and metastasis. In brain metastatic breast cancer, gap junctions are formed between breast cancer cells and astrocytes, transferring cGAMPs from cancer cells to astrocytes and producing cytokines, such as tumor necrosis factor alpha (TNF-α) and interferon alpha (IFN-α). These factors further stimulate the NF-κB and STAT1 signaling pathways in brain metastatic cells, thereby promoting cancer growth and chemotherapy resistance [35, 36].
Interactions among breast cancer, innervation, and brain metastasis. Workflow of how stress or other stimulations interact with the peripheral nervous system (sympathetic and parasympathetic nerves), including through the HPA axis, leading to the release of several neurotransmitters and hormones and promoting breast cancer growth and brain metastasis. In turn, the tumor cells in the metastatic site promote tumor growth directly or indirectly through neurons
Metastasis is one of the hallmarks of cancer. In a clinical study, nerve infiltration was observed in 28% of lymph node–positive patients, demonstrating a potential role of innervation in breast tumor metastasis [8]. In several preclinical mouse studies, neural infiltration was reported to promote breast cancer bone metastasis [37, 38]. Additionally, epinephrine (E) and norepinephrine (NE) are involved in breast cancer metastasis through α- or β-adrenergic receptors. Adrenergic signaling–driven innervation promotes breast cancer metastasis by accelerating bone degradation and bone vasculature and remodeling processes. Native bone vasculature and remodeling processes are involved in driving breast cancer cell engraftment in bone [39].
3.2 Innervation promotes breast cancer brain metastasis
Most breast cancer patients, especially those with an aggressive basal-like subtype, die from metastasis to the lung, bone, liver, and especially, the brain [40]. Breast cancer is one of the top five primary tumors that develop brain metastases. Brain metastasis has a 5-year cumulative incidence in 7% of breast cancer patients [41]. Brain metastasis patients have only a 20% probability of surviving more than a year [42]. Most brain metastatic sites occur in the parenchyma area, mainly due to the hematogenous spread, while rare metastases in the leptomeningeal and vertebral areas mostly spread along nerves or perineural lymphatics [43].
The successful colonization of breast cancer cells in the brain is quite challenging due to the harsh environment in the brain. The following steps are required for the habitation and colonization:
-
1.
Crossing the blood–brain barrier (BBB): Exosomes from highly metastatic cells increase BBB permeability in vitro and in BBB models [44].
-
2.
Dormancy after colonization: Most disseminated tumor cells undergo a variable period of dormancy before relapsing in the brain [45].
-
3.
Habitation of tumor cell behavior and nutrition: Synapses of tumor cells have been observed at metastatic sites [46].
Specifically, breast cancer cells in the brain microenvironment express GABA-related genes, enabling them to utilize GABA as a metabolite for a proliferative advantage [47]. Since metastatic cells cannot obtain enough glutamate in the brain environment, metastatic cancer cells have been found to activate the N-methyl-d-aspartate receptor (NMDAR), forming a pseudotriad synapse between cancer cells and glutamatergic neurons [48]. The activation of NMDAR-mediated colonization and the reprogrammed metastatic-innervated niche contribute to cancer cell survival [14]. In addition, the brain metastasis mechanism was reported to be mediated by astrocyte-derived miR-19a through inhibition of phosphatase and tensin homolog (PTEN) expression in breast cancer and melanoma, thereby promoting brain metastasis. When passing through the BBB, the metastatic tumor cells successfully reverse the brain metastatic microenvironment to facilitate the growth of tumor cells after a long dormant period [49].
3.2.1 HER2 amplification promotes brain metastasis
HER2 gene amplification is an important risk factor for brain metastasis. The HER2 gene encodes a transmembrane receptor tyrosine kinase that is elevated in 20–30% of human breast cancers [50]. In approximately 40% of patients with HER2 + breast cancer or TNBC, the cancer cells metastasize to the brain [51]. The association between HER2 overexpression in primary breast cancer and subsequent brain metastasis is 97% [52]. Approximately 90% of HER2 + patients will die from brain metastases [42]. In detail, the invasiveness of HER2 + breast cancer was reported to be associated with upregulated CXCR4, increasing the permeability of brain endothelial cells and promoting breast cancer cell invasion. Although HER2-directed therapy can target HER2 + breast cancer in the metastatic site [53], HER2-targeted therapies failed to reduce brain metastasis in several studies [54, 55]. Lapatinib is an irreversible tyrosine kinase inhibitor targeting HER2 with the ability to penetrate the BBB [47]. In addition, pyrotinib is an alternative strategy for the treatment of brain metastatic breast cancer, especially HER2-positive breast cancer, and has been verified to improve overall survival when combined with surgery and radiotherapy [56].
3.2.2 Immune regulation involved in brain metastasis
The brain metastasis oncogenic lncRNA (BMOR) gene promotes specific distal brain metastasis. Mechanistic studies have been revealed that cancer cells are prevented from being killed by immunity in the brain microenvironment through the BMOR-IFR3 pathway [57]. Central nervous system (CNS) myeloid cells, namely microglia and border-associated macrophages, are the major immune cell population in brain homeostasis and contribute significantly to brain disease. CNS myeloid cells promote BCBM by downregulating the expression of CX3CR1, which in turn upregulates the expression of the chemokine ligand CXCL10. Remarkably, neutralization of CXCL10 was reported to decrease BCBM, whereas CXCL10 overexpression increased BCBM by recruiting VISTAHi PD-L1+ CNS marrow to metastatic lesions. Inhibition of VISTA and PD-L1 signaling has been shown to alleviate immunosuppression and reduce BCBM [58].
In BCBM, PD-L1 and PD-L2 expression is approximately 53% and 36%, respectively [59]. In several clinical studies, PD-L1 expression was found to be significantly correlated with better survival. The survival relationship between PD-L1 expression in breast cancer and better outcomes can be explained by the presence of a strong antitumor immune response, including a high number of CD8 + T cells [60] and IFN-γ release, leading to PD-L1 upregulation [61]. Therefore, PD-L1 expression on tumor-infiltrating lymphocytes is a beneficial biomarker in prognosis and antitumor immunity, indicating the effectiveness of immune checkpoint inhibitors in BCBM [59]. Consistently, in operable breast cancer cases, a high CD8 + /PD-1 + ratio was significantly correlated with long overall survival, although tumor-infiltrating PD-1 + levels were associated with shorter overall survival [62]. Moreover, strong expression of PD-L1 and PD-L2 in the cell membrane of breast cancer cells mainly results from the alteration of several signaling pathways, including PTEN, phosphoinositide 3-kinase (PI3K), and mechanistic target of rapamycin (mTOR) [63]. PTEN loss and PI3K activation were reported to upregulate PD-L1 in the breast cancer cell membrane [64].
The BBB is often compromised with the development of brain metastases, allowing multiple immunosuppressive cells to infiltrate from periphery circulation [65]. As a type of brain cell, astrocytes regulate the brain response to inflammation [66]. In recent years, astrocytes have been reported to drive the spread of cancer to the brain by secreting interleukins (ILs) and chemokines, such as CCL2 and CXCL12/SDF1 [67], as well as by activating PPARγ, which in turn helps cancer cells gain a foothold in the brain [68, 69]. In addition, cancer cells that metastasize to the brain can interact with astrocytes by releasing different cytokines and inflammatory mediators [70], including IL-6, transforming growth factor beta (TGF-β), insulin-like growth factor 1 (IGF-1), and CXCL12α. Meanwhile, brain metastatic breast cancer can recruit type 2 tumor-associated macrophages [71,72,73,74], which play a negative role in antitumor immune responses by reducing the key molecules (including CD80, CD86, CD40, and so on) involved in T cell activation [75].
3.3 Nerves drive tumor angiogenesis and lymphangiogenesis
Tumor angiogenesis is one of the major prerequisites for tumor growth, which relies on an adequate supply of oxygen and nutrients. Likewise, new lymphatic vessels are developed in tumors to facilitate tumor cell metastasis [76]. Neuronal markers observed in tumor tissue are prognostic cancer markers [77]. Neurotransmitters and growth factors released from nerve terminals not only stimulate the proliferation of cancer cells but also promote angiogenesis [23]. In breast cancer cell lines, direct activation of β-adrenergic signaling amplifies the expression of vascular endothelial growth factor (VEGF), IL-6, and IL-8, which stimulate angiogenesis [78]. Nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF) released from breast cancer cells were reported to induce the growth of nerve fibers along breast ducts, blood vessels, and lymphatic vessels in breast tumor tissues. Notably, neurotransmitters released from adrenergic nerves stimulate angiogenesis, which promotes breast tumor growth and metastasis [79].
3.4 Innervation modulates the immune response in breast cancer
3.4.1 Adrenergic nerves promote breast cancer progression through immune suppression
Crosstalk between neural and immune cells is important in cancer immunity and inflammation [80]. Adrenergic signaling is necessary for the generation, infiltration, and activation of immune cells in the tumor microenvironment (TME), resulting in lung and lymph node metastasis [81]. In addition, stress-related catecholamines regulate lung colonization by recruiting immune cells. β-Adrenergic signaling increases the infiltration of CD11b + F4/80 + macrophages into the primary tumor parenchyma, which upregulates prometastatic gene expression and M2 macrophage infiltration [81]. In addition, β-adrenergic signaling promotes lung metastatic colonization by increasing monocyte export and macrophage infiltration. Pharmacological inactivation of β-adrenergic signaling with propranolol reversed stress-induced macrophage infiltration and inhibited tumor progression to distant tissue spread in mice [81].
Activation of the sympathetic nervous system (SNS), release of neurotransmitters, and adrenergic receptor (AR) signaling regulate solid tumor growth and metastasis [18]. A retrospective analysis of 29 breast cancer patients showed that increased sympathetic nerve density and decreased parasympathetic nerve density in tumors were associated with higher expression of immune checkpoint molecules and poor clinical outcomes [16]. Specific inhibition of the sympathetic nerve significantly inhibited tumor growth and downregulated immune checkpoint molecules (PD-1, PD-L1, and FOXP3), which was far more effective than pharmacological blockade of the α- or β-adrenergic receptor. All these findings suggest that autonomic innervation of tumors regulates breast cancer through the immune system.
3.4.2 Vagal nerves inhibit breast cancer through anti-inflammatory activity
Vagal nerves play key roles in regulating the visceral homeostasis and are beneficial for tumor development through the anti-inflammatory hypothalamic–pituitary–adrenal (HPA) axis [82]. Several clinical trials (NCT01569503, NCT02311660, NCT01552941, NCT01572155, NCT02425774) found that the vagal nerve stimulation therapy reduced chronic inflammation [82] due to its anti-inflammatory properties through acetylcholine (ACh) and the α-7-nicotinic ACh receptor (α7nAChR), since α7nAChRs are widely expressed in a variety of immune cells, including lymphocytes, macrophages, mast cells, dendritic cells, and lymphoid and myeloid cells [83]. ACh binds to α7nAChR in macrophages to inhibit the release of TNF-α. Additionally, substance P (SP) is a neuropeptide found in vagal afferent (sensory) fibers [84] and was found to inhibit cancer initiation and progression and modulate immune responses.
Vagal nerve activity and inactivation of sensory neurons have been shown to enhance visceral metastasis in 4THM breast cancer. In a 4THM breast cancer cell mouse model, vagotomy or semapimod (CNI-1493) can activate the vagal nerve. Semapimod treatment reduced lung and liver metastasis compared with vagotomized animals, and the SP levels were increased in sensory nerve endings as well [85]. Consistently, breast cancer metastasis can be promoted by surgical removal of vagal activity (vagotomy). Systemic inhibition of sensory nerve activity by high-dose capsaicin increases lung and cardiac breast cancer metastasis [86]. Therefore, vagal nerve activity is important in controlling the visceral metastasis of breast cancer.
4 Cancer cells trigger innervation through neurotransmitters and intrinsic neural expression
The transmission of information between neurons and effector cells, such as muscle cells and gland cells, occurs mainly through neurotransmitters. Neurotransmitters can be divided into cholines (ACh [87]), monoamines (catecholamines, including NE, E [88], dopamine [16], and 5-hydroxytryptamine (5-HT) [89], and histamine [90]), amino acids (excitatory transmitters, such as glutamate [91] and aspartic acid [92]; inhibitory transmitters, such as GABA [93], glycine [94], and taurine [95]), polypeptides (neuropeptides [96]), purines [97] (adenosine, adenosine triphosphate), and gaseous substances (such as nitric oxide [98]). When a neuron is stimulated by signals from the environment or other neurons, the transmitters stored in the presynaptic vesicles can be released to the synaptic cleft and act on the postsynaptic membrane, a process which is quite fast and ends when transmitters are digested or degraded by corresponding hydrolases or re-take up by presynaptic membrane-specific transmitter transporters [48]. Tumor cells were found to be able to synthesize and release a variety of neurotransmitters to induce different biological effects through their receptors [14, 96] (Table 2). Therefore, through the transmitters released and intrinsic neural genes and receptors expressed, cancer progression drives axonogenesis and neurogenesis, stimulates neural reprogramming, and has a crosstalk among the tumor, microenvironment, and nerves [99].
4.1 Catecholamines and β-adrenergic receptors
Catecholamines are monoamine neurotransmitters synthesized and secreted by the adrenal medulla, adrenal neurons, and extra-adrenal chromaffin bodies. Catecholamines include dopamine, E, and NE. E and NE have been reported to directly promote tumor cell proliferation, survival, and migration. Increased E and NE caused by psychological stress and depression favor cancer development [100]. Adrenergic receptors include α receptors and β receptors; the former cause vasoconstriction and mydriasis, while the latter cause cardiac excitation, vascular changes and bronchiectasis, and metabolic changes. The α1 receptor, located on the cell membrane (postsynaptic membrane) of noradrenergic innervated effector organs, is agonized by phenylephrine and methoxyamine and blocked by piprazole. α2 Receptors are activated by clonidine and blocked by yohimbine and are located on the presynaptic membrane, the membranes of adipocytes, and the membranes of some visceral and vascular smooth muscle cells. β Receptors, including β1, β2, and β3, bind to G proteins and activate adenylate cyclase to convert adenosine triphosphate (ATP) into cyclic adenosine monophosphate (cAMP), which in turn activates protein kinase A (PKA) [101].
The tumor-promoting activities of catecholamines predominantly depend on the activation of β-ARs. Increased expression of β-ARs for catecholamines is associated with poor prognosis in breast cancer [102]. β-AR activation promotes breast cancer cell migration and metastasis [81] and angiogenesis via the secretion of VEGF and IL-6 in various cancer cell lines [103]. The β-adrenergic signaling pathway activated by stress caused the infiltration of macrophages into tumor lesions, promoting metastasis in an orthotopic breast cancer model in BALB/c mice [81]. β-Blocker treatment suppresses metastasis and disease recurrence and improves breast cancer patient survival [104]. Moreover, β-blockers have a preventive effect on cancer development in different models [105]. Several population-based studies suggest that patients taking adrenergic antagonists for cardiovascular disease may have a significantly lower incidence of breast cancer [106]. The β1-blocker nebivolol specifically blocks oxidative phosphorylation in cancer cells by synergistically inhibiting complex I and ATP synthase activity [107]. Endothelial cells express β1-AR, and nebivolol significantly reduces glycolytic flux in endothelial cells [108] and further prevents endothelial cell proliferation and tumor angiogenesis [107].
However, there is an opposing view on the function of β2-AR in breast cancer prognosis. Positive β2-AR expression, being associated with inhibition of cell proliferation, angiogenesis, and the immune response, showed a good prognosis value in HER2-positive breast cancer patients [29]. In the 4T1 model, activation of α2-ARs increased tumor growth and metastases [109]. In contrast, blocking α-ARs in the absence of stress increased distant metastasis in an orthotopic mouse model of breast cancer [110].
4.2 ACh and cholinergic receptors
The parasympathetic system plays an important role in tumor innervation apart from the sympathetic systems. ACh is a neurotransmitter of the parasympathetic nervous system, and its biological activity is mediated by a nicotinic ACh receptor (nAChR) and muscarinic ACh receptor (mAChR) in the central nervous system and PNSs. Nicotine binds to nAChRs to promote cancer cell proliferation and invasion, including breast cancer cells. NAChRs can also regulate the synthesis and release of catecholamines in the adrenal medulla and sympathetic nerve endings. Therefore, combining cigarette smoke exposure with stress stimulation can accelerate tumor growth more than smoking or stress alone [111]. Nicotine pretreatment can stimulate the activation of α9-nAChR, promoting MCF-7 and MDA-MB-231 breast cancer cell migration [112]. MAChRs are another family of ACh receptors that activate MAPK to induce cell proliferation and protein synthesis in human breast cancer cells [113].
The vagus nerve is an important part of the parasympathetic system. The vagus nerve mainly inhibits tumorigenesis directly through a cholinergic mechanism in breast cancer. When adeno-associated virus (AAV) was injected into both human breast xenograft and transgenic mouse models to express long-acting bacterial sodium channels in tumor cholinergic nerves, the breast tumor growth was reduced [16]. Consistently, cholinergic stimulation also inhibits breast cancer by reducing PD-1 expression levels in CD4 + and CD8 + lymphocytes [114].
4.3 Dopamine and dopaminergic receptors
Dopamine is an extremely important neurotransmitter in the brain, accounting for approximately 80% of the catecholamine content in the brain. Five dopamine receptors have been identified and are divided into D1-type receptors (including D1 and D5) and D2-type receptors (D2, D3, and D4). Dopamine receptors are G protein–coupled receptors (GPCRs). Elevated D2 expression was detected in breast cancer [115]. According to the TCGA database, D1, D2, and D5 are highly expressed in adjacent normal tissues but expressed at low levels in breast cancer, while D4 is highly expressed in breast cancer but expressed at low levels in adjacent tissues. There is no such difference in D3 between breast cancer and adjacent tissue [116].
Moreover, dopamine or dopamine receptor agonists seem to exert inhibitory effects on breast cancer growth [117, 118]. Dopamine antagonists were found to be associated with an increased risk of cancer, with a dose–response relationship between a larger cumulative dose and a higher risk. Consistently, the use of antipsychotic dopamine antagonists may be associated with a small but significant risk of breast cancer [119]. The combination of dopamine or dopamine receptor agonists with anticancer drugs (such as doxorubicin or 5-fluorouracil, 5-FU) [120] can inhibit the growth of various cancer types, including breast cancer. Nonetheless, dopamine itself does not affect cancer growth. The major anticancer effects are related to the inhibition of tumor endothelial cell proliferation and migration by inhibiting VEGF receptor 2 phosphorylation and MAPK activation. These effects are mainly mediated by the D2 receptor expressed in tumor endothelial cells [121, 122].
However, dopaminergic receptors (DRs) were also observed to be highly expressed in CSCs [123] and can be targeted by DR antagonists to inhibit the proliferation of CSCs. Normal human pluripotent stem cells do not express DRs, while CSCs express all five DRs. CD44 + CD24 − CSCs express DRs in TNBC [123]. The DR antagonist thioridazine acts on the D2 receptor expressed on CSCs, specifically inhibiting CSC proliferation but not affecting normal human stem cells [124]. The D2R antagonists trifluoperazine and thioridazine eradicate CSCs in breast cancers resistant to conventional therapy [122]. Mechanistically, D2R antagonists reduce CSC proliferation and invasion by inhibiting the ERK and AKT pathways and by downregulating the expression of matrix metalloproteinase (MMP)-9 and octamer-binding transcription factor 4 (Oct-4) [125]. Additionally, D4 has also been found to be overexpressed in breast cancer, while D5 was in a low level of both breast cancer and normal breast tissues. D5 was reported to promote autophagy by increasing ROS production and inhibiting the mTOR pathway in a subset of breast cancers [126].
4.4 Serotonin and serotonin receptors
Serotonin, also known as 5-HT, is an inhibitory neurotransmitter with high content in the cerebral cortex and synapses. Serotonin receptors are located in the cell membranes and mediate the functions of serotonin and several neurotransmitters. Thus, serotonin receptors affect a variety of biological and neurological processes and are targets of a wide variety of drugs, including antidepressants and antipsychotics. Except for the 5-HT3 receptor, which is a ligand-gated ion channel, all other serotonin receptors are GPCRs that activate intracellular second messenger cascades [127, 128].
5-HT is a key local regulator of epithelial homeostasis in the breast. Human breast cancer induces complex changes in the mammary serotonin system. In normal mammary glands, 5-HT acts as a physiological regulator of lactation and involution, promoting growth arrest and cell death. However, in breast cancer cells, especially in TNBC cells, tryptophan hydroxylase (TPH)1 expression is increased, causing resistance to 5-HT-induced apoptosis [129]. For example, in MDA-MB-231 cells, 5-HT increased TPH1 and VEGF protein expression and promoted proliferation and invasion through the 5-HT7 receptor. In addition, 5-HT was found to have a stronger effect in the early stage of metastasis than in the later stage [89], showing an important role in breast cancer progression.
In addition, enzymes, such as monoamine oxidase A (MAOA) [130] that degrade catecholamines and serotonin, play an important role in cancer metastasis. Several studies have reported that a low level of MAOA is correlated with breast cancer invasion and that the inhibition of MAOA stimulates the malignant behavior of MDA-MB-231 cells [131, 132]. In contrast, MAOA was also reported to promote tumor sphere formation and might drive breast tumor–initiating cells [133]. While serotonin reuptake transporter inhibitors and serotonin receptor inhibitors were found to inhibit mouse breast cancer–initiating cell activity, serotonin transporter antagonists were found to target tumor-initiating cells in a transgenic mouse model of breast cancer [134]. The selective serotonin reuptake inhibitor (SSRI) sertraline (Zoloft) was reported to promote the efficiency of docetaxel in controlling breast tumor growth [134]. In addition, studies of 6959 consecutive newly diagnosed breast cancer patients in northern Israel showed that selective SSRI use within 5 years prior to breast cancer diagnosis was associated with a 66% increase in overall mortality, while after diagnosis, the use of SSRIs was associated with an 81% increase in mortality [135].
Depression is common in breast cancer patients, approximately 32.8% have depressive symptoms, and 42% of recurrent cases were diagnosed with depression [136]. A recent study reported the antitumor potential of 5-HT receptor 1A (HTR1A) in breast cancer cells [137]. HTR1A interacts with TRIM21 to inhibit the TGF-β pathway [137]. Thus, HTR1A is an independent predictive factor for breast cancer patients and might provide a new approach for TNBC treatment. Therefore, 5-HT, its receptors, and the related enzyme MAOA can play both promotive and inhibitory roles in breast cancer progression. However, the underlying mechanisms behind are still unclear.
4.5 GABA and GABAergic receptors
GABA is a major inhibitory neurotransmitter synthesized from glutamine, glutamate, and glucose by GAD65 and GAD67. GABA binds to GABA-A, GABA-B, and GABA-C receptors with different functions. GAD is only expressed in normal nervous tissues; however, recent studies have shown that GABA can also be secreted by cancer cells, dendritic cells, T cells, natural killer (NK) cells, macrophages, and B cells [138].
GABA levels are positively correlated with breast cancer metastasis. The expression of GABA-A receptors, GABA transporters, and GABA transaminases was found to be significantly upregulated in brain metastatic breast cancer cells compared with primary breast cancer cell lines. GAD and GABRP were also upregulated [139]. Almost 50% of all breast cancer types exhibit high GABRP levels [139], which are usually elevated both in circulating breast cancer cells and in metastatic lymph nodes isolated from breast cancer patients [140]. Patients with metastatic breast cancer express eightfold higher GABRP levels than stage II–IV patients without evidence of metastasis [141] and 30-fold higher levels than stage I patients without evidence of metastasis, suggesting that the GABRP expression level increases with metastasis. Elevated GABRP expression levels were also effective in detecting circulating tumor cells in stage I (65%), stages II–IV without evidence of metastasis (72%), and metastatic (88.5%) breast cancer patients. Since circulating tumor cells are an important indicator of overall survival in breast cancer patients [142], detection of GABRP could be used to monitor disease progression.
GABRP could be a promising marker and therapeutic target for BLBC [33]. Normal mammary luminal progenitor cells, which give rise to BLBC cells during carcinogenesis, express high levels of GABRP [143], further suggesting a strong link between GABRP and BLBC subtypes [144, 145]. GABRP knockdown inhibited TNBC cell proliferation in vitro and inhibited the growth of MDA-MB-468 xenografts in nude mice [33]. Knockdown of GABRP in BLBC cell lines decreased the phosphorylation of ERK1/2 [33]. Similarly, antitumor properties were observed when knocking down GABRP gene expression or employing a GABRP antibody [146], further underscoring the prospective role of GABRP as a therapeutic target in breast cancer.
Elevated expression of GABA and GABA-A receptors reshapes brain metastatic breast cancer cells to behave like neurons. BLBC patients often develop distant metastasis in the lung, liver, and brain [147, 148]. Breast-to-brain metastatic cells display a GABAergic phenotype similar to that of neuronal cells. GABA-A receptors, GABA transporters, GABA transaminases, parvalbumin, and reelin are all highly expressed in brain metastatic breast cancer cells so that these cancer cells can take up GABA and catabolize it to succinate, which serves as a biosynthetic source, thereby gaining a proliferation advantage [32]. Nevertheless, metastatic breast cancer cells mimic neuron-like cells, allowing breast cancer cells to adapt to the brain microenvironment and use GABA as a metabolite [149].
GABA promotes breast cancer metastasis through ALDH1A3. High ALDH activity (due to ALDH1A3 isoform activity) is a well-known feature of breast CSCs and is associated with a poorer prognosis, including tumor growth, invasion, metastasis, and chemoresistance [150, 151]. High expression of both ALDH1A3 and GABA resulted in increased lung and brain metastasis in mice bearing orthotopic MDA-MB-231 tumors [33]. Metabolite analysis of patient tumor samples demonstrated that GABA promotes breast cancer metastases through GABA metabolism, which is associated with ALDH1A3. High levels of ALDH1A3 in breast tumor cells convert GABA into N-acetylputrescine and glutamate [34]. N-Acetylputrescine is a polyamine metabolized by amino acids such as l-ornithine, lysine, and l-arginine. An increasing number of reports in the literature have now identified polyamine catabolism as a contributory factor in the development of many cancer types, including breast cancer [152, 153].
Additionally, GABA promotes breast tumor progression by regulating the immune response. Abundant glutamine is available in the tumor environment to synthesize GABA [154]. Blockage of GABA can activate the expression of specific cytokines (such as Ccl4 and Ccl5) in the tumor, which promotes the infiltration of dendritic cells and T cells. When B cells are activated, they release GABA to promote monocyte differentiation into anti-inflammatory macrophages and suppress antitumor CD8 + T cell responses through IL-10. GABA can bind to and activate GABA type A receptors (GABA-A-Rs) on nearby immune cells, such as macrophages and CD8 + T cells. In breast cancer, the GABA-B receptor was reported to interact with CXCR4, a receptor for the chemokine CXCL12 (stromal cell–derived factor 1α). Furthermore, both GABAB antagonists and agonists can block CXCL12-elicited chemotaxis, possibly by influencing high-threshold Ca2+ channels [155].
4.6 Glutamate and NMDARs
Glutamate, a nonessential amino acid, is both a major bioenergetic substrate in cells and an excitatory neurotransmitter involved in biosynthesis, bioenergetics, metabolism, and oncogenic signaling [156]. Interestingly, there is growing evidence that glutamate can function through its receptors in human malignancies. Dysregulation of glutamate transporters, such as excitatory amino acid transporters and the cystine/glutamate antitransport system, in turn activates glutamate receptors on cancer cells and leads to malignant growth [157]. According to a metabolic analysis of 270 clinical breast cancer samples and 97 normal breast tissues, 56% of ER + tumor tissues and 88% of ER − tumor tissues are glutamate rich [158]. A higher glutamate-to-glutamine ratio was significantly correlated with ER status, a higher tumor grade, and prolonged overall survival. A possible explanation is that patients with glutamate-enriched tumors could be more sensitive to cytotoxic chemotherapy. And, this is a retrospective cohort analysis with a limited median follow-up time of 40 months in 249 patients (28 deaths). ER-negative and selective ER-positive breast cancers are more sensitive to the recently discovered glutaminase inhibitors (BPTES and 968) [158].
Moreover, breast cancer cells secrete high levels of glutamate and frequently metastasize to bone. Exogenous glutamate disrupts normal bone turnover and may contribute to cancer-induced bone pain (CIBP). Scientists have identified effective inhibitors of glutamate secretion in MDA-MB-231 and MCF-7 cells [159]. These inhibitors targeting glutamate release may provide a novel strategy for inhibiting pain propagation by blocking the mechanism causing the pain, especially those caused by metastases.
Neuronal and non-neuronal brain cells express different classes of glutamate receptors, which are divided into ionotropic glutamate receptors (iGluRs) and metabotropic glutamate receptors (mGluRs/Grms) [160]. iGluRs are quaternary ligand-gated ion channels classified into 3 subfamilies: N-methyl-d-aspartate (NMDA) receptors, α-amino-3-hydroxy-5-methyl-4-isooxazole propionate (AMPA) receptors, and kainic acid receptors [161]. As glutamate-gated ion channel receptors, NMDARs have been detected in different tumors [162]. NMDARs are activated by binding to glutamate or glycine, resulting in calcium ion entry and membrane depolarization. Activation of NMDARs promotes breast cancer metastasis to the brain [48]. NMDAR subunits are highly expressed in brain metastatic breast cancer cell lines. Knockdown of an NMDAR subunit suppressed tumor growth and increased brain metastasis-free survival in subjects but did not affect their primary tumor burden or lung metastases [99]. Furthermore, NMDAR activation limits the duration of signaling by ERK1/2, which dampens mTOR signaling activity [163]. NMDAR antagonists (MK-801 or dizocilpine) inhibit breast cancer cell proliferation and invasion through the mTOR and ERK signaling pathways [163]. Given the antiproliferative effects of NMDAR agonists, clinical trials and precise patient selection may validate the therapeutic potential of these emerging antineoplastic agents [164].
Glutamate antagonists have shown potential enhancing effects when combined with cytostatic drug therapy in breast cancer [91]. AMPA antagonists (GYKI52466) inhibit breast cancer cell proliferation and invasion. Breast cancer cells were sensitive to the antiproliferative effect of NMDAR antagonists (dizocilpine) and GYKI52466. Glutamate antagonists contribute to antiproliferation through Ca2+ channels and altered Ca2+ concentrations. Tumor cell morphology can also be changed because of reduced membrane ruffling and pseudopodial protrusions. Therefore, both NMDAR and AMPA antagonists have potential therapeutic effects in breast cancer treatment [91].
mGluR1 is a member of the GPCR superfamily that participates in synaptic transmission and neuronal excitability. Aberrant mGluR1 expression was detected and explored as a novel target for breast cancer treatment in a clinical study. In a microarray containing 394 consecutive primary breast cancer tissues, approximately 56% (n = 219) of breast cancer tissues showed mGluR1 expression. mGluR1 expression (31% (n = 18/58)) was significantly associated with metastasis-free survival (MFS) in ER-negative tumors. mGluR1 expression (11/44) in TNBC was significantly associated with shorter MFS and with poor OS. In conclusion, mGluR1 is frequently expressed and plays a role as an unfavorable prognostic marker in TNBC [165]. There were 131 genes differentially expressed in mGluR1-silenced MDA-MB-231 cells compared with control cells. Four major canonical pathways associated with acute inflammation (such as upregulation of CXCL1, IL-6, and IL-8) were included. Therefore, mGluR1 was identified as a novel endogenous regulator of inflammation in TNBC [166].
In addition, mGluR1-expressing immature mammary epithelial cells exhibited delayed lumen formation. The implantation of mGluR1-expressing immature mammary epithelial cells into nude mouse mammary fat pads resulted in mammary tumor formation. Consistently, mGluR1 was observed to be expressed in human breast cancer cell lines and breast tumor biopsies. Furthermore, the glutamate release inhibitor and an AKT inhibitor led to tumor growth inhibition in MCF-7 xenografts. Therefore, mGluR1 plays an oncogenic role in breast cancer and could be a potential therapeutic target [167].
4.7 Neprilysin
Neprilysin is a cell surface peptidase that is able to degrade angiotensin II, endothelin I, and substance P, among others. Neprilysin is expressed in various tissues including the breast; however, neprilysin is downregulated in breast tumor tissues. The tumor-suppressor mechanisms of neprilysin mainly rely on its peptidase activity and its protein–protein interaction with PTEN, focal adhesion kinase, ezrin/radixin/moesin, and PI3K. Neprilysin can be downregulated by histone deacetylation and hypermethylation of the neprilysin gene promoter region, resulting in angiogenesis, cell survival, and cell migration [168].
4.8 Endorphins
Endorphins are mood elevators that can be stimulated by physical activity [169]. A home-based physical activity intervention was found to be related to fewer mood disturbances among breast cancer survivors [170]. Similarly, breast cancer survivors were observed to have more positive moods after completing an exercise intervention. In addition, physical activity prevents survivors from experiencing disease stress, provides them opportunities for social interactions, and improves self-confidence and body image. A clinical study used an adaptive cognitive-behavioral stress management intervention to treat 114 women diagnosed with breast cancer (any stage of disease, any type of breast cancer) and found that physical activity interventions may improve quality of life and mood in this population [171].
4.9 Melatonin
Melatonin, an indoleamine that is highly available during darkness, is a hormone derived from tryptophan and secreted by the pineal gland. Melatonin is naturally occurring in mammals and has been shown to have a variety of antitumor effects targeting different molecules and signaling pathways, such as angiogenesis, remodeling of the extracellular matrix, migration, and epithelial-to-mesenchymal transition (EMT) in many cancer types, including breast cancer [172]. Melatonin treatment in the daytime in human breast cancer xenografts regulated plasma metabolites and thus controlled the aggressiveness at an early stage [173].
In addition, melatonin treatment caused the upregulation of Bax expression but the downregulation of Bcl-2 expression, thus inhibiting the growth of breast cancer cells by inducing cell death in both MCF-7 and MDA-MB-231 cells [174]. In addition, in breast cancer, melatonin was reported to play a role in cancer-inhibitory processes through epigenetic modifications, such as DNA methylation [175].
Melatonin plays an important role as a sensitizer to both irradiation and chemotherapy breast cancer treatments. Melatonin behaves as a radiosensitizer in breast cancer through the upregulation of PTEN and NME/NM23 nucleoside diphosphate kinase 1 (NME1) and the downregulation of SNAI2, HER2, and AKT. In addition, the cancer suppressor miR-34a can be enhanced by melatonin [176]. Furthermore, melatonin is a potent antioxidant, chemotherapeutic, and chemopreventive agent against breast cancer. Melatonin has potential in breast cancer treatment applications.
However, the recent research reached the surprising conclusion that the production of circulating tumor cells (CTCs) with a high metastatic tendency mainly occurs in the sleep stage and is not continuous [177]. Hematogenous dissemination of CTCs is a vital method for cancer metastasis. In breast cancer patients and mouse models, the generation of CTCs mainly occurs in the sleep stage, and these cells have a greater tendency to metastasize. Single-cell RNA sequencing analysis revealed a marked upregulation of mitotic genes, including melatonin, testosterone, and glucocorticoids during the rest period of the study [177]. Researchers have found that testosterone, glucocorticoids, and insulin play the main roles in promoting metastasis and proliferation during sleep, but the role of melatonin in this process is still not clear.
4.10 Neurotrophic factor
Neurotrophins (NTs) are one of the most studied trophic factors and play an important role in neuronal development, survival, and apoptosis. Neurotrophic factors are growth factors and include NGF, BDNF, NT-3, and NT-4/5, and possibly NT-6 [178]. Cellular responses to NTs are elicited through two types of cell membrane receptors: the common NT receptor (NTR) p75NTR and the tyrosine kinase (Trk) receptor [15, 179]. Proneurotrophin interacts with receptor p75 (a member of the TNF receptor superfamily) or a co-receptor complex, p75, and sortilin, a transmembrane protein containing the Vps10p domain. The mature form acts by binding to specific Trks (Trk A, Trk B, and Trk C). NTs and their receptors regulate cell proliferation, migration, differentiation, survival, apoptosis, and synaptic plasticity [180, 181]. A two-protein hybrid formed by the p75NTR and Trk A monomer can enhance the specific binding affinity of NGF. However, when the homodimer formed by the polymerization of two p75 NTRs binds to NT, it can cause the opposite effect and even induce apoptosis.
Trk A receptors have higher affinity for NGF. Trk B receptors have higher affinity for BDNF and NT-4/5. Trk C receptors primarily bind to NT-3. Various receptors exist in the form of dimers, and the activation of receptors can trigger the phosphorylation of tyrosine protein kinases in the cytoplasm. By interacting with the extracellular domains of these receptors, neurotrophic factors transmit signals related to the survival and apoptosis of nerve cells to the interior of cells, thereby regulating cell behaviors. p75NTR can bind to all neurotrophic factors. In addition, there are both synergistic and antagonistic effects between p75NTR and Trk.
4.10.1 Nerve growth factor
The discovery of NGF was a milestone in the study of growth factors. NGF is necessary for the growth and survival of sympathetic and sensory neurons. Since sensory fibers supply the papilla and skin, sympathetic fibers innervate blood vessels and ducts. In particular, breast cancer cells can produce and secrete NGF, which stimulates the growth of sympathetic and sensory nerves. Likewise, there is a correlation between nerve fibers and NGF expression in breast cancer cells [8]. Axogenesis is correlated with tumor aggressiveness and is driven by NGF [182]. Axon formation can be partially reversed by blocking NGF [8]. NGF receptor (NGFR) is expressed in a variety of cancer types. BLBC shows a higher level than other subtypes [183]. NGF signaling through NGFR in CSCs may drive cancer growth in vitro [99].
4.10.2 Brain-derived neurotrophic factor
BDNF is the most studied and well-characterized neurotrophic factor in the CNS. In mammals, BDNF plays a role in neuronal activity, including proper growth, development, synaptic plasticity [184], neuronal differentiation [185], and neurotransmission [186], through Trk B and the low-affinity p75NTR [187]. In addition, BDNF protein is detectable in several non-neural tissues, such as endothelial cells [188] and vascular smooth muscle cells [189]. Thus, BDNF may act through angiogenesis. Recent studies have shown that cancer cell–derived BDNF promotes axon formation, which in turn promotes tumor cell invasion [99]. BDNF has been reported to be aberrantly expressed in human breast cancer, and elevated levels of BDNF are associated with poor clinical outcomes and decreased survival [190]. Knockdown of BDNF in the MDA-MB-231 and MCF-7 cell lines resulted in reduced cell proliferation and survival.
Aberrant activation of the BDNF/Trk B pathway can modulate multiple signaling pathways, including the PI3K/AKT, Jak/STAT, NF-κB, uPA/uPAR, Wnt/β-catenin and VEGF pathways, and ER receptors. BDNF can act in an autocrine or paracrine manner to increase the migratory capacity of MDA-MB-231 cells and HUVECs. BDNF-induced migration activity was blocked by inhibitors of Trk B, PI3K, and ERK in MDA-MB-231 cells. Overexpression of Trk B, but not BDNF, was significantly associated with poor survival outcomes in TNBC patients [191]. Several approaches have been developed to target this pathway, such as Trk inhibitors (AZD6918, CEP-701) and RNA interference, which can sensitize the xenograft tumors to etoposide, a topoisomerase II inhibitor [192]. One study found that estradiol (E2) treatment upregulated BDNF expression in astrocytes and later Trk B expression in breast cancer cells to promote brain metastasis of TNBC cell xenografts [193]. Interestingly, the brain metastatic process induced by E2 could be rescued by treatment with ANA-12, a BDNF/Trk B inhibitor.
However, in hormone receptor-positive mammary tumor models, BDNF overexpression in the hypothalamus of mice through a recombinant AAV vector resulted in anticancer phenotypes [194]. The above BDNF gene therapy was further reported to inhibit breast cancer cell growth by reducing inflammatory markers [194]. Therefore, BDNF might also play protumorigenic and antitumorigenic roles through different pathways in different breast cancer subtypes.
4.10.3 Neurotrophin
Various NTs have different roles in protecting neurons from apoptosis. Both NT-3 and NT-4/5 can bind to p75NTR to stimulate breast cancer cell survival [195]. NT-3 enhances breast cancer brain metastasis by promoting the transition of breast cancer cells from mesenchymal-epithelial cells to a more epithelioid phenotype and by increasing the ability of these cells to proliferate in the brain [196]. NT-4/5 is also expressed and secreted by breast cancer cells, and anti-NT-4/5 antibody treatment resulted in tumor growth inhibition characterized by increased apoptosis but no change in proliferation. NT-4/5 contributes to breast cancer cell survival and may serve as a potential target for suppressing tumor growth [197].
4.10.4 Tyrosine kinase receptors
The Trk family consists of Trk A, Trk B, and Trk C. NTs that bind to Trks are known to activate their kinase domains to trigger various downstream Ras signaling pathways involving MAPK, PI3K, and PLCγ-PKC [162]. This has primarily been established in neuronal models. Various non-neuronal cells have been reported to respond to neurotrophic factors in healthy tissues and in disease states [198]. p75NTR and Trks, two types of NTRs, have been discovered in numerous cancer types, including breast tumors [199]. Activated p75NTR, which traditionally acts as an inhibitor, induces variable effects, from inhibition to stimulation of cell proliferation in cancers, dependent on its direct or coordinated/indirect mechanism(s) of action. Trk B was reported to stimulate cell proliferation, aggressiveness, and metastasis in cancer. Anti-Trk drugs have been investigated both in vitro and in living mice for their effects on various cancer cells, and some are in clinical trials [199]. p75NTR and Trks were also expressed in various cancers, including breast, lung, colon-rectum, pancreas, prostate, glioblastoma, neuroblastoma, myeloma, and lymphoid tumors [199]. The potent pan-Trk inhibitor entrectinib is a promising agent targeted against many cancers including mammary carcinomas [200] Besides, a series of novel 7-azaindole-based Trk inhibitors exhibited antiangiogenic activity in breast cancer [201]. At present, the potential of LOXO-101, another anti-Trk drug, applied in soft-tissue sarcoma and colorectal cancer is in phase 2 trials [202, 203]. Other Trk inhibitors (GNF-5837, MGCD516, PLX7486, DS7486, DS6051b, and TSR-011) are underway [202].
4.11 Netrin-1, an axon guidance factor
Netrin-1 is a laminin-related protein involved in nervous system development and regulates neurite outgrowth. In addition, netrin-1 is also involved in cell adhesion, motility, proliferation, differentiation, apoptosis, and angiogenesis. Netrin-1 and its receptors have been reported to promote tumorigenesis in a variety of cancer types [204]. By comparing 300 plasma samples from different cancer patients compared to 138 plasma samples from healthy donors, plasma netrin-1 levels were found to be significantly elevated in breast, kidney, prostate, and liver cancer and in meningiomas, pituitary adenomas, and glioblastomas. Therefore, plasma netrin-1 can be used as a diagnostic biomarker for human cancers [205]. Since netrin-1 co-localizes with endothelial CD31 in breast tumors, netrin-1 expression can be assessed via ultrasound molecular imaging (USMI), which is used to visualize vascular endothelial targets. The USMI signal of anti-netrin-1 was significantly increased in human SKBR7 mammary tumors [206].
The netrin-1 receptors, including deleted in colorectal cancer (DCC) and uncoordinated 5 homologs (UNC5H), belong to a family of dependent receptors that induce apoptosis in the absence of netrin-1, conferring the tumor suppressor activity. However, most metastatic breast cancers overexpress netrin-1. When netrin-1 was knocked down or DCC and UNC5H were overexpressed, the apoptosis of mammary metastatic tumor cell lines was increased [207]. In addition, death-associated protein kinase (DAPK)1 is a serine-threonine kinase known to transduce the proapoptotic pathway of netrin-1-dependent receptors. A considerable number of human breast tumors show a loss of DNA methylation–dependent expression of DAPK1, while inhibition of DNA methylation (such as decitabine) can restore DAPK1 expression [208]. Therefore, combining DNA methylation inhibitors with netrin-1 neutralizers may be a valuable strategy against cancer.
4.12 Others
Neurogenic SP is an 11-amino acid peptide that belongs to the tachykinin family and is widely expressed in the central, peripheral, and enteric nervous systems of vertebrates. SP and its high-affinity receptor (neurokinin-1 receptor) have been shown to be involved in several physiological and pathophysiological processes, such as respiration, thermoregulation, immune regulation, inflammation, and tumorigenesis [209]. Both SP and neurokinin-1 are overexpressed in breast cancer and other cancer types [210]. SPs have been shown to exert anticancer functions by inducing the immune responses of T cells and NK cells [211]. However, in breast cancer, SP and its receptors have been implicated in oncogenic transformation and myeloid metastasis formation [212]. Neurokinin-1 receptor antagonists can block the mitogenic effects of SP and produce proapoptotic effects in vitro and in vivo. Therefore, the neurokinin-1 receptor is a candidate therapeutic target for cancer therapy [213]. In breast cancer cells, SP activates MMPs through neurokinin-1 receptors and turn on HER2 through Src, promoting proliferation and invasion [214, 215]. In fact, cancer cells activate autocrine circuits by releasing SP. In tumor models of breast cancer cells (MDA-MB-231 and MDA-MB-453), a neurokinin-1 antagonist (L-733,060) inhibited tumor growth and showed a synergistic effect with anti-HER2 therapy (AG825, AG1478, or lapatinib).
Neuropeptide Y enhances VEGF expression, promoting angiogenesis and breast cancer progression [216]. Neurotensin promotes metastasis by binding to neurotensin receptor 1 (NTSR1). In breast cancer, NTSR1 expression is associated with lymph node metastasis [217]. These studies demonstrate the important role of neuropeptide signaling in breast cancer metastasis (Fig. 3).
Signaling pathways of innervation and therapeutic targets in primary or metastatic breast cancer microenvironment. In the microenvironment of primary or metastatic breast cancer sites, there are complicated interactions among synapses from surrounding nerves, metastatic breast cancer cells, breast cancer cells, and immune cells. Neurotransmitter release, related receptors, and signaling pathways are included in this model. Furthermore, several effective drugs mentioned in the text are shown in red text
5 Psychological stress promotes breast cancer progression
Chronic psychological stress is reported to be correlated with poor clinical outcomes in cancer patients [218]. The communication between neural, endocrine, and immune factors transmits various signals that induce cancer cell proliferation, invasion, metabolism reprogramming, and therapy resistance [219]. A large number of studies have demonstrated that psychosocial factors are associated with a higher incidence and lower survival in patients with different cancer types, including breast cancer [220]. Anxiety and depression are closely related to tumor development and progression due to the sustained secretion of stress-related hormones and neurotransmitters [18]. Specifically, the SNS and the HPA axis are activated when exposed to stress, releasing several neurotransmitters and hormones that promote cancer progression [221].
Preclinical breast cancer mouse models have shown that chronic restraint stress promoted breast cancer progression via catecholamine and α-AR signaling [110]. The nonselective α-adrenergic blocker phentolamine was found to inhibit tumor growth and metastasis caused by stress exposure. Interestingly, phentolamine increased primary tumor size and distant metastasis under nonstress conditions. Chronic stress–related tumor metastasis also depends on the activation of β2-AR [222]. Selective sympathetic destruction by the neurotoxin 6-hydroxydopamine (6-OHDA) decreased tumor NE concentrations by approximately 50% [223]. When exposed to stressors, tumor NE turnover was increased compared to spleen and nonstressed tumor NE turnover in mice. Ablation of sympathetic nerve function by 6-OHDA or blockade of β-adrenergic signaling by propranolol significantly inhibited stress-induced lung metastasis [224]. Depletion of circulating monocytes or lung macrophages strongly abrogated stress-induced tumor cell lung dissimilation, whereas treatment of mice with the β-adrenergic agonist isoproterenol (ISO) during the premetastatic phase promoted the infiltration of macrophages into the lung. β-Adrenergic signaling upregulates multiple genes that contribute to tumor progression and metastasis, while glucocorticoid-regulated genes can promote cancer cell survival and resistance to chemotherapy [224].
Chronic stress was reported to activate the SNS and drive malignancy. In immunodeficient murine models, chronic stress–induced E was found to promote breast cancer stem-like properties via lactate dehydrogenase A (LDHA)-dependent metabolic rewiring. Chronic stress–induced E activated LDHA to generate lactate, and the adjusted pH directed USP28-mediated deubiquitination and stabilization of MYC, promoting SLUG expression and breast cancer stem-like trait development. The LDHA-lowering agent vitamin C can be a potential approach for combating stress-associated breast cancer [225].
In a mouse model, social defeat was observed to cause anxiety-like behaviors and reduce therapeutic responses against carcinogen-induced neoplasia and transplantable tumors. Stress elevated plasma corticosterone and upregulated the expression of glucocorticoid-inducible factor Tsc22d3, which blocked type I IFN responses in dendritic cells and IFN-γ + T cell activation. Administration of a glucocorticoid receptor (GR) antagonist or DC-specific Tsc22d3 deletion reversed the negative impact of stress or glucocorticoid supplementation on therapeutic outcomes [226].
Dexamethasone (DEX) was reported to promote breast cancer cell metastasis by activating the PI3K signaling pathway and upregulating serum glucocorticoid-inducible kinase 1 (SGK1) expression. In a standard breast cancer treatment regimen with paclitaxel and DEX, DEX was found to promote lung metastasis [227]. In addition, DEX induces docetaxel and cisplatin resistance in TNBC cells by upregulating KLF5 expression, a prosurvival transcription factor, and this regulation is dependent on GR [228]. Glucocorticoid treatment facilitated GR-dependent nuclear accumulation and transcriptional activation of TEAD4, the activation of which promoted breast CSC maintenance, cell survival, metastasis, and chemoresistance both in vitro and in vivo [229].
Therefore, psychological and social factors can modulate tumor cell gene expression, reconfirming that stress promotes cancer progression by activating the SNS to release E and NE and activating the HPA axis to release cortisol. Stress reduction is an important breast cancer therapy.
Pharmacological strategies include eliminating the β2-AR signaling pathway to block the effects of E and NE [230]. Clinical trials showed that treatment with β-blockers reduced stress-related signaling, prolonging cancer patient survival [231, 232]. In addition, nonpharmacological methods such as meditation [233], yoga [234], acupuncture [235], exercise [236], support groups, counseling, natural products, and herbal compounds [237] have been reported to inhibit breast cancer [238]. Although coffee and tea can regulate the nervous system, epidemiological studies suggest that the relationship between drinking coffee or tea and breast cancer is controversial [239, 240].
Regular exercise, also called physical activity and recommended by the World Health Organization, has been observed to be associated with a 7% decrease in overall cancer risk. Among cancer types, breast cancer shows one of the strongest associations [241]. When compared with the least active women, the physically active women have a 25% average risk decrease [242]. Furthermore, increased physical activity is associated with increased overall survival of breast cancer patients [243].
All these effects are induced by regular exercise through the systemic control of energy homeostasis and metabolism, which have important effects on the inflammatory and immune mediators in breast cancer tumor microenvironment [244], including metabolic factors (IGF-1 or its binding protein IGFBP-3, insulin, glucose, C-peptide, leptin), immune and inflammatory factors (NK cell cytotoxicity, pro-inflammatory and anti-inflammatory cytokines), and oxidative stress (8-oxo-dG, F2-isoprostane) [245].
Exercise-induced TNBC prevention is mainly based on the inhibition of PI3K-AKT-mTOR signaling [244]. First, physical activity induces changes in inflammatory and immune mediators that contribute to beneficial effects on breast cancer outcomes, including tumor growth reduction, metastasis inhibition, and survival improvement. Commonly measured immune factors include splenic cell number and function, circulating inflammatory cytokines, intratumoral immune cells, and inflammatory markers. The results from preclinical and clinical studies suggest that PA exerts heterogeneous effects on inflammatory cytokines but may alter the gene expression profile and immune infiltrates in the tumor, which may result in a reduction in immunosuppressive factors [246]. Furthermore, regular exercise can upregulate oncostatin M (OSM) and myokine [247]. The exercise-inducible myokine irisin was reported to reduce the risk and improve the prognosis of breast cancer [248].
6 Targeting innervation in breast cancer treatment
6.1 Drugs targeting β-adrenergic signaling
Catecholamine-mediated activation of β-adrenergic signaling plays critical roles in cancer proliferation, invasion, metastasis, and angiogenesis. β-Blockers are commonly used in hypertension and arrhythmia treatments. In an analysis of 46,265 patients, the use of β-blockers improved cancer-specific survival [249]. β-Blocker use reduces the risk of breast cancer–related death in women with breast cancer [250] and reduces the risk of recurrence in women with breast cancer and hypertension [251]. In addition, propranolol reduces restraint stress–induced distant metastasis of orthotopic xenografts by inhibiting tumor-associated macrophage infiltration in breast cancer [81]. However, not all β-blockers are effective in breast cancer. The β1-specific blocker atenolol had no such effect [252]. In contrast, ISO, a nonselective β-AR agonist, promotes tumor invasion and metastasis [253].
The timing of β-blocker application is related to the therapeutic efficiency. Patients who used β-blockers before cancer diagnosis had a 57% lower risk of metastasis and a 71% reduction in breast cancer mortality after 10 years. Tumor recurrence was significantly reduced [104]. The use of β-blockers at the start of neoadjuvant therapy was associated with slightly better recurrence-free survival but not overall survival [254, 255]. Preoperative use of β-blockers (propranolol) is associated with decreased EMT and decreased prometastatic/proinflammatory transcription factor activity in early breast cancer [255].
Concomitant preoperative use of β-blockers (propranolol) reduces mesenchymal gene expression in primary early breast cancer tumors. Nonselective β-blockers employed in patients with early breast cancer may lead to reduced tumor proliferation [256]. In general, β-blockers may improve immune surveillance a few days before surgery [257]. This may be correlated with increased catecholamine-mediated immunosuppressive activity after surgery, possibly attributable to psychological distress. In addition, pharmacologic (propranolol) and genetic (β2-AR knockout) inhibition reduced tumor growth implanted under chronic cold stress [114]. Therefore, the introduction of β-blockers in breast cancer treatment requires strict control of disease progression, treatment timing, and basic health regulation of patients to achieve the best results (Table 3 and Fig. 3) [24].
6.2 Drugs targeting GABA and the 5-HT transporter
The use of the intravenous anesthetic propofol in breast cancer surgery is reported to be significantly associated with breast cancer prognosis by both promoting and inhibiting breast cancer growth and metastasis [258]. On the one hand, propofol was observed to increase MDA-MB-468 cell migration [259] by increasing intracellular calcium and altering the actin cytoskeleton organization [260]. One possible explanation is that propofol increases breast cancer cell migration by activating GABA-A receptors, a process that increases intracellular reorganization of L-type calcium channels and the calcium-related actin cytoskeleton [260]. Consistently, the GABABR agonist baclofen significantly promoted 4T1 cell migration and invasion, which was attenuated by the GABABR antagonist CGP55845 [261]. In addition, the proliferation and migration of MDA-MB-231 cells were increased by propofol treatment, which was explained by the correlation with upregulation of nuclear factor E2-related factor 2 and downregulation of p53 expression [262]. On the other hand, propofol significantly suppressed the migration and invasion of MDA-MB-231 cells [263] by reducing MMP-2 and MMP-9 expression and decreasing neuroepithelial cell–transforming gene 1 (NET1) [264], which are important in promoting migration. In addition, the propofol also downregulated miR-24 and increased p27 expression and cleaved caspase-3 expression in MDA-MB-435 cells, leading to induced cell death [265]. In another study, MDA-MB-231 cells were incubated with serum from patients after propofol/paravertebral block anesthesia group, resulting in decreased viability due to increased apoptosis compared to that of cells incubated with serum from patients receiving sevoflurane/opioid anesthesia [266]. Similarly, when ER + /PR + breast cancer cells (HCC1500) were co-cultured with NK cells obtained from healthy donors in the presence of the above serum, HCC1500 cells underwent apoptosis. Concomitantly, CD107a is upregulated in stimulated NK cells and results in NK cell–mediated lysis of target cells [267]. The inconsistent effects of propofol in breast cancer cells were correlated with different breast cancer subtypes and the dosage and exposure time. This might be explained by the fact that when combined with paravertebral block, propofol causes serum composition changes, affecting breast cancer cell behavior and NK cell activity [258].
However, there are uncertain results concerning the application of SSRIs in breast cancer treatments. Since nearly 50% of breast cancer patients suffer from depression or anxiety, first-line antidepression drugs have been implicated in breast cancer progression through increased prolactin levels and tamoxifen metabolism inhibition. SSRIs and serotonin receptor inhibitors were found to inhibit breast cancer–initiating cell activity in mice [134]. Sertraline (Zoloft) promoted the efficiency of docetaxel in controlling breast tumor growth [134] and contributed to the relief of hot flashes in breast cancer survivors taking tamoxifen and to controlling the accompanying depression [268]. However, selective SSRI use, either before or after breast cancer diagnosis, was observed to be co-related with an increase in overall mortality [135].
6.3 Nerve-specific blocking virus
It is well known that sympathetic nerves are cancer-promoting in breast cancer, while parasympathetic/vagal nerves play a tumor-suppressing role in breast cancer. These neural effects may be mediated by β-adrenergic or muscarinic receptors and may be explained by changes in cancer cell behavior, angiogenesis, tumor-associated macrophages, and adaptive antitumor immunity. A recently developed viral vector-based genetic localized neural engineering technique is a powerful approach to selectively manipulate specific types of nerve fibers that innervate the cancer microenvironment, thereby inhibiting cancer progression [16]. The technology will enable the creation of “cancer neurotherapies” that are individually tailored to different cancer types [24]. AAV vector-based gene deletion or local tumor sympathetic nerve stimulation greatly reduced or increased primary tumor growth and distant metastasis of orthotopic xenografts and chemo-induced tumors [16] and was more efficient than the β-blockers because of the immune-suppression function [24]. Thus, cancer-specific and nerve-specific manner would be more accurate while pharmacological blockade would target different organs with α- or β-adrenergic receptor expression. In detail, tumor-specific sympathetic denervation downregulated the expression of immune checkpoint molecules (PD-1, PD-L1, and FOXP3) while genetically simulated parasympathetic innervation decreased PD-1 and PD-L1 expression in immune-competent breast cancer models. These neural effects may be mediated by the M1 Chrm, since the M1-specific antagonist pirenzepine decreased these effects [16].
6.4 Relieve pressure strategies
The development of breast cancer is associated with a variety of factors, including stress, anxiety, depression, sleep disturbance, and fatigue. Stress promotes cancer progression by activating the SNS to release E and NE and by activating the HPA axis to release cortisol. The National Center for Complementary and Alternative Medicine, an initiative of the National Institutes of Health (NIH) [269], recommends the use of health care, including mind–body medicine, nutritional supplements, herbal products, exercise, and other energy-based techniques and practice programs, for disease treatment. A European study that included 11 countries reported complementary and alternative medicine (CAM) use in 44.7% of breast cancer patients [270], resulting in high levels of satisfaction, while only 6.5% of the women reported no benefits. In a US study, 86.1% of patients used CAM after breast cancer diagnosis: 47.5% used botanical supplements, 47.2% used other natural products, 28.8% used special diets, 64.2% used mind–body therapy, and 26.5% used body/energy/other treatments [271]. Other CAMs used by breast cancer patients include spiritual methods such as prayer, meditation, and psychotherapy [272]. Spiritual and religious practice has been one of the coping strategies used by breast cancer patients [273]. After assessing the quality of related reviews of CAM studies, CAM could be concluded to be helpful for treating specific symptoms related in breast cancer patients [274] and thus should be considered before clinical treatment. In addition, methods such as therapeutic massage in breast cancer patients have shown beneficial effects on the neuroendocrine and immune systems, reducing anxiety levels, depression, anger, fear, and stress and improving NK and lymphocyte counts.
In the past decade, the development of neuro-oncology has achieved milestones, and numerous studies from different aspects have verified that the nervous system plays an active role in the occurrence and development of breast cancer. Furthermore, ablation of specific nerve types (parasympathetic, sympathetic, or sensory) can eliminate tumor growth in a tissue-specific manner, showing a promising prospective role in breast cancer treatment.
7 Conclusions and perspectives
Neuro-oncology has undoubtedly developed into an independent emerging discipline, with several ensured conclusions:
-
1.
Peripheral nerves and solid tumors support each other’s growth directly or indirectly. It is important to elucidate the signaling pathways initiated by neurotransmitters, neuropeptides, and their associated receptors. Global characterization of the neurotransmitters or neuropeptides present in the tumor microenvironment will provide insight into the true biological impact of neuronal organization on tumor progression. Cancer cells can take advantage of factors released by nerve fibers to create a microenvironment for cancer cell survival and proliferation. Cancer cells can also behave like nerves in a microenvironment stimulated by nerves and their neurotransmitters or neuropeptides, which can be both released from both nerves in the microenvironment and cancer cells as well. In return, the secretion of neurotrophic factors and axon-guiding molecules by breast cancer cells stimulates synapse formation, and newly formed adrenergic nerve fibers promote tumor growth.
-
2.
Breast cancer neural invasion not only leads to breast cancer treatment resistance but also promotes distant metastasis and increases the mortality of breast cancer patients. According to a large number of clinical and preclinical studies, innervation in breast cancer alters gene expression, which is co-related with chemotherapy resistance, tumor angiogenesis, lymphangiogenesis, and brain metastasis. In addition, innervation can also modulate the immune response mediated by cytokines and immunocytes in the breast cancer microenvironment.
-
3.
Furthermore, multiple clinical strategies such as pharmacological and genetic approaches could be applied to block neuronal signaling pathways in the TME, showing a promising therapeutic potential for the treatment of breast cancer. The ensured pharmacological drugs are mainly β-blockers. Genetic technology specifically aimed at different nerve types is still under development.
-
4.
The SNS and the HPA axis are activated by stress to promote breast cancer progression. Nonpharmacological methods to relieve pressure, such as meditation, yoga, acupuncture, physical activity, support groups, counseling, natural products, and herbal compounds, would benefit breast cancer patients.
Therefore, in-depth exploration of the mechanisms of neural infiltration and its important contribution to the synergistic network among tumors, the immune system, and endocrine cells is conducive to targeted intervention. Further understanding of the network would overcome the unfavorable factors in breast cancer treatment and improve the survival of breast cancer patients. Currently, the most ensured and effective treatments that are beneficial in breast cancer patients, aside from the standard regimen, are pharmacological methods to reduce stress, such as taking β-blockers, and other methods such as exercising and relaxing. Therefore, understanding the role of nerves played in breast cancers is promising for future cancer therapies, and nerves could be valuable targets alone or in combination with the currently available standard therapeutic regimens.
However, further studies are required to solve the unknown aspects of current studies. The exact role of each nerve in the complex neuronal network and their interaction with each other in the face of the changeable breast cancer environment according to different development and treatment stages and even the psychological stress levels in each patient need to be clearly elucidated. Although the immune checkpoint molecules can be regulated by innervation or denervation through pharmacological or genetic techniques in preclinical animals, they need to be improved before being applied safely and efficiently in clinical managements.
In addition, the nervous system is quite sophisticated, and mature neuron’ culture in vitro is challenging. The development of appropriate models to investigate the interaction of nerves and tumor cells in vitro and in vivo is currently limited. Researchers usually investigate nerve roles through mouse models that are genetically edited and transplanted with tumors with or without metastatic sites. Physical activity and CAM strategies can be observed in human beings.
Furthermore, although it has been confirmed that physical and relaxing activity can benefit cancer patient survival, it is significant to elucidate the detailed mechanisms and the specific way the highest efficiency can be obtained when combined with clinical treatments. In addition, clinicians should also pay attention to the CAM employed by patients before and after regimen therapies, and it would be helpful to make standard guidelines as supplementation for clinical therapies.
Therefore, a good and appropriate mouse model or special clinical cases with innervation in the primary site or with brain metastasis would be a good opportunity to discover more about the neuro-malignancy circuit.
Data availability
There is no data relevant to be presented in this work.
Abbreviations
- 5-FU:
-
5-Fluorouracil
- 5-HT:
-
5-Hydroxytryptamine
- 6-OHDA:
-
Neurotoxin 6-hydroxydopamine
- AAV:
-
Adeno-associated virus
- ACh:
-
Acetylcholine
- AChE:
-
Acetylcholinesterase
- ALDH:
-
Aldehyde dehydrogenase
- AMPA:
-
α-Amino-3-hydroxy-5-methyl-4-isooxazole propionate
- AR:
-
Adrenergic receptor
- ATP:
-
Adenosine triphosphate
- BBB:
-
Blood-brain barrier
- BCBM:
-
Breast cancer brain metastasis
- bChE:
-
Butyrylcholinesterase
- BDNF:
-
Brain-derived neurotrophic factor
- BLBC:
-
Basal-like breast cancer
- BMOR:
-
Brain metastasis oncogenic lncRNA
- CAM:
-
Complementary and alternative medicine
- cAMP:
-
Cyclic adenosine monophosphate
- Chrm1:
-
Cholinergic receptor 1
- CIBP:
-
Cancer-induced bone pain
- CNS:
-
Central nervous system
- CSC:
-
Cancer stem cell
- CTC:
-
Circulating tumor cell
- CXCL:
-
Chemokine ligand
- DAPK:
-
Death-associated protein kinase
- DCC:
-
Deleted in colorectal cancer
- DEX:
-
Dexamethasone
- DR:
-
Dopaminergic receptor
- DRG:
-
Dorsal root ganglia
- E:
-
Epinephrine
- E2:
-
Estradiol
- EMT:
-
Epithelial-to-mesenchymal transition
- ER:
-
Estrogen receptor
- ERK:
-
Extracellular signal–regulated kinase
- GABA:
-
Gamma-aminobutyric acid
- GABRP:
-
Pi subunit of the GABA-A receptor
- GAD:
-
Glutamate decarboxylase
- GEO:
-
Gene Expression Omnibus
- GPCR:
-
G protein–coupled receptor
- GR:
-
Glucocorticoid receptor
- HER2:
-
Human epidermal growth factor receptor 2
- HPA:
-
Hypothalamic-pituitary-adrenal
- HTR1A:
-
5-HT receptor 1A
- IFN:
-
Interferon
- IGF:
-
Insulin-like growth factor
- iGluR:
-
Ionotropic glutamate receptor
- IL:
-
Interleukin
- ISO:
-
Isoproterenol
- LDHA:
-
Lactate dehydrogenase A
- mAChR:
-
Muscarinic acetylcholine receptor
- MAOA:
-
Monoamine oxidase A
- MAPK:
-
Mitogen-activated protein kinase
- METABRIC:
-
Molecular Taxonomy of Breast Cancer International Consortium
- MFS:
-
Metastasis-free survival
- mGluR1/Grm1:
-
Metabotropic glutamate receptor 1
- mTOR:
-
Mechanistic target of rapamycin
- nAChR:
-
Nicotinic acetylcholine receptor
- NE:
-
Norepinephrine
- NET:
-
Neuroepithelial cell–transforming gene
- NGF:
-
Nerve growth factor
- NK:
-
Natural killer
- NMDAR:
-
N-Methyl-d-aspartate receptor
- NT:
-
Neurotrophin
- NTR:
-
Neurotrophin receptor
- NTSR1:
-
Neurotensin receptor 1
- Oct-4:
-
Octamer-binding transcription factor 4
- OSM:
-
Oncostatin M
- PD-1:
-
Programmed death 1
- PD-L1:
-
Programmed death ligand 1
- PI3K:
-
Phosphoinositide 3-kinase
- PKA:
-
Protein kinase A
- PNS:
-
Peripheral nervous system
- PTEN:
-
Phosphatase and tensin homolog
- SGK1:
-
Serum glucocorticoid-inducible kinase 1
- SNS:
-
Sympathetic nervous system
- SP:
-
Substance P
- SSRI:
-
Selective serotonin reuptake inhibitor
- TCGA:
-
The Cancer Genome Atlas
- TGF-β:
-
Transforming growth factor beta
- TME:
-
Tumor microenvironment
- TNBC:
-
Triple-negative breast cancer
- TNF:
-
Tumor necrosis factor
- TPH:
-
Tryptophan hydroxylase
- Trk:
-
Tyrosine kinase
- TRPV1:
-
Transient receptor potential vanilloid 1
- UNC5H:
-
Uncoordinated 5 homolog
- USMI:
-
Ultrasound molecular imaging
- VEGF:
-
Vascular endothelial growth factor
- α7nAChR:
-
α-7-Nicotinic acetylcholine receptor
References
Breast Cancer Association, C., Dorling, L., Carvalho, S., Allen, J., Gonzalez-Neira, A., Luccarini, C., Wahlstrom, C., Pooley, K. A., Parsons, M. T., Fortuno, C., Wang, Q., Bolla, M. K., Dennis, J., Keeman, R., Alonso, M. R., Alvarez, N., Herraez, B., Fernandez, V., Nunez-Torres, R., … Easton, D. F. (2021). Breast cancer risk genes - Association analysis in more than 113,000 women. New England Journal of Medicine, 384(5), 428–439. https://doi.org/10.1056/NEJMoa1913948
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209–249. https://doi.org/10.3322/caac.21660
Zhao, S., Ma, D., Xiao, Y., Li, X. M., Ma, J. L., Zhang, H., Xu, X. L., Lv, H., Jiang, W. H., Yang, W. T., Jiang, Y. Z., Zhang, Q. Y., & Shao, Z. M. (2020). Molecular subtyping of triple-negative breast cancers by immunohistochemistry: Molecular basis and clinical relevance. The Oncologist, 25(10), e1481–e1491. https://doi.org/10.1634/theoncologist.2019-0982
Monje, M., Borniger, J. C., D’Silva, N. J., Deneen, B., Dirks, P. B., Fattahi, F., Frenette, P. S., Garzia, L., Gutmann, D. H., Hanahan, D., Hervey-Jumper, S. L., Hondermarck, H., Hurov, J. B., Kepecs, A., Knox, S. M., Lloyd, A. C., Magnon, C., Saloman, J. L., Segal, R. A., … Winkler, F. (2020). Roadmap for the emerging field of cancer neuroscience. Cell, 181(2), 219–222. https://doi.org/10.1016/j.cell.2020.03.034
Valiente, M., Ahluwalia, M. S., Boire, A., Brastianos, P. K., Goldberg, S. B., Lee, E. Q., Le Rhun, E., Preusser, M., Winkler, F., & Soffietti, R. (2018). The evolving landscape of brain metastasis. Trends Cancer, 4(3), 176–196. https://doi.org/10.1016/j.trecan.2018.01.003
Achrol, A. S., Rennert, R. C., Anders, C., Soffietti, R., Ahluwalia, M. S., Nayak, L., Peters, S., Arvold, N. D., Harsh, G. R., Steeg, P. S., & Chang, S. D. (2019). Brain metastases. Nature Reviews Disease Primers, 5(1), 5. https://doi.org/10.1038/s41572-018-0055-y
Hanahan, D. (2022). Hallmarks of cancer: New dimensions. Cancer Discovery, 12(1), 31–46. https://doi.org/10.1158/2159-8290.CD-21-1059
Pundavela, J., Roselli, S., Faulkner, S., Attia, J., Scott, R. J., Thorne, R. F., Forbes, J. F., Bradshaw, R. A., Walker, M. M., Jobling, P., & Hondermarck, H. (2015). Nerve fibers infiltrate the tumor microenvironment and are associated with nerve growth factor production and lymph node invasion in breast cancer. Molecular Oncology, 9(8), 1626–1635. https://doi.org/10.1016/j.molonc.2015.05.001
Zahalka, A. H., & Frenette, P. S. (2020). Nerves in cancer. Nature Reviews Cancer, 20(3), 143–157. https://doi.org/10.1038/s41568-019-0237-2
Liebig, C., Ayala, G., Wilks, J. A., Berger, D. H., & Albo, D. (2009). Perineural invasion in cancer: A review of the literature. Cancer, 115(15), 3379–3391. https://doi.org/10.1002/cncr.24396
Hanoun, M., Maryanovich, M., Arnal-Estape, A., & Frenette, P. S. (2015). Neural regulation of hematopoiesis, inflammation, and cancer. Neuron, 86(2), 360–373. https://doi.org/10.1016/j.neuron.2015.01.026
Magnon, C., Hall, S. J., Lin, J., Xue, X., Gerber, L., Freedland, S. J., & Frenette, P. S. (2013). Autonomic nerve development contributes to prostate cancer progression. Science, 341(6142), 1236361. https://doi.org/10.1126/science.1236361
Ayala, G. E., Dai, H., Powell, M., Li, R., Ding, Y., Wheeler, T. M., Shine, D., Kadmon, D., Thompson, T., Miles, B. J., Ittmann, M. M., & Rowley, D. (2008). Cancer-related axonogenesis and neurogenesis in prostate cancer. Clinical Cancer Research, 14(23), 7593–7603. https://doi.org/10.1158/1078-0432.CCR-08-1164
Jin, M. Z., & Jin, W. L. (2020). The updated landscape of tumor microenvironment and drug repurposing. Signal Transduction and Targeted Therapy, 5(1), 166. https://doi.org/10.1038/s41392-020-00280-x
Hondermarck, H. (2012). Neurotrophins and their receptors in breast cancer. Cytokine & Growth Factor Reviews, 23(6), 357–365. https://doi.org/10.1016/j.cytogfr.2012.06.004
Kamiya, A., Hayama, Y., Kato, S., Shimomura, A., Shimomura, T., Irie, K., Kaneko, R., Yanagawa, Y., Kobayashi, K., & Ochiya, T. (2019). Genetic manipulation of autonomic nerve fiber innervation and activity and its effect on breast cancer progression. Nature Neuroscience, 22(8), 1289–1305. https://doi.org/10.1038/s41593-019-0430-3
Gruet, M., Cotton, D., Coveney, C., Boocock, D. J., Wagner, S., Komorowski, L., Rees, R. C., Pockley, A. G., Garner, A. C., Wallis, J. D., Miles, A. K., & Powe, D. G. (2020). β2-Adrenergic signalling promotes cell migration by upregulating expression of the metastasis-associated molecule LYPD3. Biology (Basel), 9(2). https://doi.org/10.3390/biology9020039
Cole, S. W., Nagaraja, A. S., Lutgendorf, S. K., Green, P. A., & Sood, A. K. (2015). Sympathetic nervous system regulation of the tumour microenvironment. Nature Reviews Cancer, 15(9), 563–572. https://doi.org/10.1038/nrc3978
Zhang, L., Wu, L. L., Huan, H. B., Chen, X. J., Wen, X. D., Yang, D. P., & Xia, F. (2017). Sympathetic and parasympathetic innervation in hepatocellular carcinoma. Neoplasma, 64(6), 840–846. https://doi.org/10.4149/neo_2017_605
Jesinger, R. A. (2014). Breast anatomy for the interventionalist. Techniques in Vascular and Interventional Radiology, 17(1), 3–9. https://doi.org/10.1053/j.tvir.2013.12.002
Sarhadi, N. S., Shaw-Dunn, J., & Soutar, D. S. (1997). Nerve supply of the breast with special reference to the nipple and areola: Sir Astley Cooper revisited. Clinical Anatomy, 10(4), 283–288. https://doi.org/10.1002/(SICI)1098-2353(1997)10:4%3c283::AID-CA12%3e3.0.CO;2-G
Hebb, C., & Linzell, J. L. (1970). Innervation of the mammary gland. A histochemical study in the rabbit. Histochemical Journal, 2(6), 491–505. https://doi.org/10.1007/BF01003127
Hondermarck, H., Huang, P. S., & Wagner, J. A. (2021). The nervous system: Orchestra conductor in cancer, regeneration, inflammation and immunity. FASEB BioAdvances, 3(11), 944–952. https://doi.org/10.1096/fba.2021-00080
Kamiya, A., Hiyama, T., Fujimura, A., & Yoshikawa, S. (2021). Sympathetic and parasympathetic innervation in cancer: Therapeutic implications. Clinical Autonomic Research, 31(2), 165–178. https://doi.org/10.1007/s10286-020-00724-y
Erin, N., Akman, M., Aliyev, E., Tanriover, G., & Korcum, A. F. (2022). Olvanil activates sensory nerve fibers, increases T cell response and decreases metastasis of breast carcinoma. Life Sciences, 291, 120305. https://doi.org/10.1016/j.lfs.2022.120305
Le Madeleine, T. T., & Oudin, M. J. (2021). Abstract PO047: Sensory nerves enhance breast cancer migration through plexinB3 signaling. Cancer Research, 81(5). https://doi.org/10.1158/1538-7445.Tme21-Po047
Shi, M., Liu, D., Duan, H., Qian, L., Wang, L., Niu, L., Zhang, H., Yong, Z., Gong, Z., Song, L., Yu, M., Hu, M., Xia, Q., Shen, B., & Guo, N. (2011). The β2-adrenergic receptor and Her2 comprise a positive feedback loop in human breast cancer cells. Breast Cancer Research and Treatment, 125(2), 351–362. https://doi.org/10.1007/s10549-010-0822-2
Gargiulo, L., May, M., Rivero, E. M., Copsel, S., Lamb, C., Lydon, J., Davio, C., Lanari, C., Luthy, I. A., & Bruzzone, A. (2017). A novel effect of β-adrenergic receptor on mammary branching morphogenesis and its possible implications in breast cancer. Journal of Mammary Gland Biology and Neoplasia, 22(1), 43–57. https://doi.org/10.1007/s10911-017-9371-1
Caparica, R., Richard, F., Brandao, M., Awada, A., Sotiriou, C., & de Azambuja, E. (2020). Prognostic and predictive impact of beta-2 adrenergic receptor expression in HER2-positive breast cancer. Clinical Breast Cancer, 20(3), 262-273 e267. https://doi.org/10.1016/j.clbc.2020.01.007
Liu, D., Deng, Q., Sun, L., Wang, T., Yang, Z., Chen, H., Guo, L., Liu, Y., Ma, Y., Guo, N., & Shi, M. (2015). A Her2-let-7-β2-AR circuit affects prognosis in patients with Her2-positive breast cancer. BMC Cancer, 15, 832. https://doi.org/10.1186/s12885-015-1869-6
Tan, R., Li, H., Huang, Z., Zhou, Y., Tao, M., Gao, X., & Xu, Y. (2020). Neural functions play different roles in triple negative breast cancer (TNBC) and non-TNBC. Science and Reports, 10(1), 3065. https://doi.org/10.1038/s41598-020-60030-5
Neman, J., Termini, J., Wilczynski, S., Vaidehi, N., Choy, C., Kowolik, C. M., Li, H., Hambrecht, A. C., Roberts, E., & Jandial, R. (2014). Human breast cancer metastases to the brain display GABAergic properties in the neural niche. Proceedings of the National Academy of Sciences, 111(3), 984–989. https://doi.org/10.1073/pnas.1322098111
Sizemore, G. M., Sizemore, S. T., Seachrist, D. D., & Keri, R. A. (2014). GABA(A) receptor pi (GABRP) stimulates basal-like breast cancer cell migration through activation of extracellular-regulated kinase 1/2 (ERK1/2). Journal of Biological Chemistry, 289(35), 24102–24113. https://doi.org/10.1074/jbc.M114.593582
Dahn, M. L., Walsh, H. R., Dean, C. A., Giacomantonio, M. A., Fernando, W., Murphy, J. P., Walker, O. L., Wasson, M. C. D., Gujar, S., Pinto, D. M., & Marcato, P. (2022). Metabolite profiling reveals a connection between aldehyde dehydrogenase 1A3 and GABA metabolism in breast cancer metastasis. Metabolomics, 18(1). https://doi.org/10.1007/s11306-021-01864-6
Mao, X. Y., Li, Q. Q., Gao, Y. F., Zhou, H. H., Liu, Z. Q., & Jin, W. L. (2016). Gap junction as an intercellular glue: Emerging roles in cancer EMT and metastasis. Cancer Letters, 381(1), 133–137. https://doi.org/10.1016/j.canlet.2016.07.037
Chen, Q., Boire, A., Jin, X., Valiente, M., Er, E. E., Lopez-Soto, A., Jacob, L. S., Patwa, R., Shah, H., Xu, K., Cross, J. R., & Massague, J. (2016). Carcinoma-astrocyte gap junctions promote brain metastasis by cGAMP transfer. Nature, 533(7604), 493–498. https://doi.org/10.1038/nature18268
Campbell, J. P., Karolak, M. R., Ma, Y., Perrien, D. S., Masood-Campbell, S. K., Penner, N. L., Munoz, S. A., Zijlstra, A., Yang, X., Sterling, J. A., & Elefteriou, F. (2012). Stimulation of host bone marrow stromal cells by sympathetic nerves promotes breast cancer bone metastasis in mice. PLoS Biology, 10(7), e1001363. https://doi.org/10.1371/journal.pbio.1001363
Wu, R., Li, K., Yuan, M., & Luo, K. Q. (2021). Nerve growth factor receptor increases the tumor growth and metastatic potential of triple-negative breast cancer cells. Oncogene. https://doi.org/10.1038/s41388-021-01691-y
Conceicao, F., Sousa, D. M., Paredes, J., & Lamghari, M. (2021). Sympathetic activity in breast cancer and metastasis: Partners in crime. Bone Res, 9(1), 9. https://doi.org/10.1038/s41413-021-00137-1
Lin, N. U., Amiri-Kordestani, L., Palmieri, D., Liewehr, D. J., & Steeg, P. S. (2013). CNS metastases in breast cancer: Old challenge, new frontiers. Clinical Cancer Research, 19(23), 6404–6418. https://doi.org/10.1158/1078-0432.CCR-13-0790
Schouten, L. J., Rutten, J., Huveneers, H. A., & Twijnstra, A. (2002). Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer, 94(10), 2698–2705. https://doi.org/10.1002/cncr.10541
Lin, N. U., & Winer, E. P. (2007). Brain metastases: The HER2 paradigm. Clinical Cancer Research, 13(6), 1648–1655. https://doi.org/10.1158/1078-0432.CCR-06-2478
Kesari, S., & Batchelor, T. T. (2003). Leptomeningeal metastases. Neurol Clin, 21(1):25-+. Pii S0733–8619(02)00032–4. https://doi.org/10.1016/S0733-8619(02)00032-4
Morad, G., Carman, C. V., Hagedorn, E. J., Perlin, J. R., Zon, L. I., Mustafaoglu, N., Park, T. E., Ingber, D. E., Daisy, C. C., & Moses, M. A. (2019). Tumor-derived extracellular vesicles breach the intact blood-brain barrier via transcytosis. ACS Nano, 13(12), 13853–13865. https://doi.org/10.1021/acsnano.9b04397
Neman, J., Somlo, G., & Jandial, R. (2010). Classification of genomic changes in breast cancer brain metastasis. Neurosurgery, 67(2), N18-19. https://doi.org/10.1227/01.NEU.0000386966.69913.79
Lu, H., Chen, I., Shimoda, L. A., Park, Y., Zhang, C., Tran, L., Zhang, H., & Semenza, G. L. (2021). Chemotherapy-induced Ca2+ release stimulates breast cancer stem cell enrichment. Cell Reports, 34(1), 108605. https://doi.org/10.1016/j.celrep.2020.108605
Lin, N. U., Bellon, J. R., & Winer, E. P. (2004). CNS metastases in breast cancer. Journal of Clinical Oncology, 22(17), 3608–3617. https://doi.org/10.1200/JCO.2004.01.175
Zeng, Q., Michael, I. P., Zhang, P., Saghafinia, S., Knott, G., Jiao, W., McCabe, B. D., Galvan, J. A., Robinson, H. P. C., Zlobec, I., Ciriello, G., & Hanahan, D. (2019). Synaptic proximity enables NMDAR signalling to promote brain metastasis. Nature, 573(7775), 526–531. https://doi.org/10.1038/s41586-019-1576-6
Zhang, L., Zhang, S., Yao, J., Lowery, F. J., Zhang, Q., Huang, W. C., Li, P., Li, M., Wang, X., Zhang, C., Wang, H., Ellis, K., Cheerathodi, M., McCarty, J. H., Palmieri, D., Saunus, J., Lakhani, S., Huang, S., Sahin, A. A., … Yu, D. (2015). Microenvironment-induced PTEN loss by exosomal microRNA primes brain metastasis outgrowth. Nature, 527(7576), 100–104. https://doi.org/10.1038/nature15376
Slamon, D. J., Godolphin, W., Jones, L. A., Holt, J. A., Wong, S. G., Keith, D. E., Levin, W. J., Stuart, S. G., Udove, J., Ullrich, A., & Press, M. F. (1989). Studies of the Her-2/Neu proto-oncogene in human-breast and ovarian-cancer. Science, 244(4905), 707–712. https://doi.org/10.1126/science.2470152
Wolff, A. C., Hammond, M. E., Schwartz, J. N., Hagerty, K. L., Allred, D. C., Cote, R. J., Dowsett, M., Fitzgibbons, P. L., Hanna, W. M., Langer, A., McShane, L. M., Paik, S., Pegram, M. D., Perez, E. A., Press, M. F., Rhodes, A., Sturgeon, C., Taube, S. E., Tubbs, R., … American Society of Clinical Oncology/College of American P. (2007). American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Archives of Pathology and Laboratory Medicine, 131(1), 18–43. https://doi.org/10.1043/1543-2165(2007)131[18:ASOCCO]2.0.CO;210.5858/2007-131-18-ASOCCO
Fuchs, I. B., Loebbecke, M., Buhler, H., Stoltenburg-Didinger, G., Heine, B., Lichtenegger, W., & Schaller, G. (2002). HER2 in brain metastases: Issues of concordance, survival, and treatment. Journal of Clinical Oncology, 20(19), 4130–4133. https://doi.org/10.1200/JCO.2002.04.016
Cheng, X., & Hung, M. C. (2007). Breast cancer brain metastases. Cancer and Metastasis Reviews, 26(3–4), 635–643. https://doi.org/10.1007/s10555-007-9083-x
Pestalozzi, B. C., Holmes, E., de Azambuja, E., Metzger-Filho, O., Hogge, L., Scullion, M., Lang, I., Wardley, A., Lichinitser, M., Sanchez, R. I., Muller, V., Dodwell, D., Gelber, R. D., Piccart-Gebhart, M. J., & Cameron, D. (2013). CNS relapses in patients with HER2-positive early breast cancer who have and have not received adjuvant trastuzumab: A retrospective substudy of the HERA trial (BIG 1–01). The lancet Oncology, 14(3), 244–248. https://doi.org/10.1016/S1470-2045(13)70017-2
von Minckwitz, G., Huang, C. S., Mano, M. S., Loibl, S., Mamounas, E. P., Untch, M., Wolmark, N., Rastogi, P., Schneeweiss, A., Redondo, A., Fischer, H. H., Jacot, W., Conlin, A. K., Arce-Salinas, C., Wapnir, I. L., Jackisch, C., DiGiovanna, M. P., Fasching, P. A., Crown, J. P., … Investigators, K. (2019). Trastuzumab emtansine for residual invasive HER2-positive breast cancer. New England Journal of Medicine, 380(7), 617–628. https://doi.org/10.1056/NEJMoa1814017
Anwar, M., Chen, Q., Ouyang, D., Wang, S., Xie, N., Ouyang, Q., Fan, P., Qian, L., Chen, G., Zhou, E., Guo, L., Gu, X., Ding, B., Yang, X., Liu, L., Deng, C., Xiao, Z., Li, J., Wang, Y., … Yi, W. (2021). Pyrotinib treatment in patients with HER2-positive metastatic breast cancer and brain metastasis: Exploratory final analysis of real-world, multicenter data. Clinical Cancer Research, 27(16), 4634–4641. https://doi.org/10.1158/1078-0432.CCR-21-0474
Liu, W., Sun, P., Xia, L., He, X., Xia, Z., Huang, Y., Liu, W., Li, L., & Chen, L. (2022). A brain-enriched lncRNA shields cancer cells from immune-mediated killing for metastatic colonization in the brain. Proc Natl Acad Sci U S A, 119(22), e2200230119. https://doi.org/10.1073/pnas.2200230119
Guldner, I. H., Wang, Q., Yang, L., Golomb, S. M., Zhao, Z., Lopez, J. A., Brunory, A., Howe, E. N., Zhang, Y., Palakurthi, B., Barron, M., Gao, H., Xuei, X., Liu, Y., Li, J., Chen, D. Z., Landreth, G. E., & Zhang, S. (2020). CNS-native myeloid cells drive immune suppression in the brain metastatic niche through Cxcl10. Cell, 183(5), 1234-1248 e1225. https://doi.org/10.1016/j.cell.2020.09.064
Duchnowska, R., Peksa, R., Radecka, B., Mandat, T., Trojanowski, T., Jarosz, B., Czartoryska-Arlukowicz, B., Olszewski, W. P., Och, W., Kalinka-Warzocha, E., Kozlowski, W., Kowalczyk, A., Loi, S., Biernat, W., Jassem, J., & Polish Brain Metastasis, C. (2016). Immune response in breast cancer brain metastases and their microenvironment: The role of the PD-1/PD-L axis. Breast Cancer Research, 18(1), 43. https://doi.org/10.1186/s13058-016-0702-8
Spranger, S., Spaapen, R. M., Zha, Y., Williams, J., Meng, Y., Ha, T. T., & Gajewski, T. F. (2013). Up-regulation of PD-L1, IDO, and T(regs) in the melanoma tumor microenvironment is driven by CD8(+) T cells. Sci Transl Med, 5(200), 200ra116. https://doi.org/10.1126/scitranslmed.3006504
Kinter, A. L., Godbout, E. J., McNally, J. P., Sereti, I., Roby, G. A., O’Shea, M. A., & Fauci, A. S. (2008). The common gamma-chain cytokines IL-2, IL-7, IL-15, and IL-21 induce the expression of programmed death-1 and its ligands. The Journal of Immunology, 181(10), 6738–6746. https://doi.org/10.4049/jimmunol.181.10.6738
Sun, S., Fei, X., Mao, Y., Wang, X., Garfield, D. H., Huang, O., Wang, J., Yuan, F., Sun, L., Yu, Q., Jin, X., Wang, J., & Shen, K. (2014). PD-1(+) immune cell infiltration inversely correlates with survival of operable breast cancer patients. Cancer Immunology, Immunotherapy, 63(4), 395–406. https://doi.org/10.1007/s00262-014-1519-x
Akcakanat, A., Sahin, A., Shaye, A. N., Velasco, M. A., & Meric-Bernstam, F. (2008). Comparison of Akt/mTOR signaling in primary breast tumors and matched distant metastases. Cancer, 112(11), 2352–2358. https://doi.org/10.1002/cncr.23456
Mittendorf, E. A., Philips, A. V., Meric-Bernstam, F., Qiao, N., Wu, Y., Harrington, S., Su, X., Wang, Y., Gonzalez-Angulo, A. M., Akcakanat, A., Chawla, A., Curran, M., Hwu, P., Sharma, P., Litton, J. K., Molldrem, J. J., & Alatrash, G. (2014). PD-L1 expression in triple-negative breast cancer. Cancer Immunology Research, 2(4), 361–370. https://doi.org/10.1158/2326-6066.CIR-13-0127
Quail, D. F., & Joyce, J. A. (2017). The microenvironmental landscape of brain tumors. Cancer Cell, 31(3), 326–341. https://doi.org/10.1016/j.ccell.2017.02.009
Kim, S. J., Kim, J. S., Park, E. S., Lee, J. S., Lin, Q., Langley, R. R., Maya, M., He, J., Kim, S. W., Weihua, Z., Balasubramanian, K., Fan, D., Mills, G. B., Hung, M. C., & Fidler, I. J. (2011). Astrocytes upregulate survival genes in tumor cells and induce protection from chemotherapy. Neoplasia, 13(3), 286–298. https://doi.org/10.1593/neo.11112
Sarvaiya, P. J., Guo, D., Ulasov, I., Gabikian, P., & Lesniak, M. S. (2013). Chemokines in tumor progression and metastasis. Oncotarget, 4(12), 2171–2185. https://doi.org/10.18632/oncotarget.1426
Zou, Y., Watters, A., Cheng, N., Perry, C. E., Xu, K., Alicea, G. M., Parris, J. L. D., Baraban, E., Ray, P., Nayak, A., Xu, X., Herlyn, M., Murphy, M. E., Weeraratna, A. T., Schug, Z. T., & Chen, Q. (2019). Polyunsaturated fatty acids from astrocytes activate PPARγ signaling in cancer cells to promote brain metastasis. Cancer Discovery, 9(12), 1720–1735. https://doi.org/10.1158/2159-8290.CD-19-0270
Kaverina, N., Borovjagin, A. V., Kadagidze, Z., Baryshnikov, A., Baryshnikova, M., Malin, D., Ghosh, D., Shah, N., Welch, D. R., Gabikian, P., Karseladze, A., Cobbs, C., & Ulasov, I. V. (2017). Astrocytes promote progression of breast cancer metastases to the brain via a KISS1-mediated autophagy. Autophagy, 13(11), 1905–1923. https://doi.org/10.1080/15548627.2017.1360466
Farber, S. H., Tsvankin, V., Narloch, J. L., Kim, G. J., Salama, A. K., Vlahovic, G., Blackwell, K. L., Kirkpatrick, J. P., & Fecci, P. E. (2016). Embracing rejection: Immunologic trends in brain metastasis. Oncoimmunology, 5(7), e1172153. https://doi.org/10.1080/2162402X.2016.1172153
Quail, D. F., & Joyce, J. A. (2013). Microenvironmental regulation of tumor progression and metastasis. Nature Medicine, 19(11), 1423–1437. https://doi.org/10.1038/nm.3394
Du Four, S., Maenhout, S. K., De Pierre, K., Renmans, D., Niclou, S. P., Thielemans, K., Neyns, B., & Aerts, J. L. (2015). Axitinib increases the infiltration of immune cells and reduces the suppressive capacity of monocytic MDSCs in an intracranial mouse melanoma model. Oncoimmunology, 4(4), e998107. https://doi.org/10.1080/2162402X.2014.998107
Hambardzumyan, D., Gutmann, D. H., & Kettenmann, H. (2016). The role of microglia and macrophages in glioma maintenance and progression. Nature Neuroscience, 19(1), 20–27. https://doi.org/10.1038/nn.4185
Jacobs, J. F., Idema, A. J., Bol, K. F., Nierkens, S., Grauer, O. M., Wesseling, P., Grotenhuis, J. A., Hoogerbrugge, P. M., de Vries, I. J., & Adema, G. J. (2009). Regulatory T cells and the PD-L1/PD-1 pathway mediate immune suppression in malignant human brain tumors. Neuro-Oncology, 11(4), 394–402. https://doi.org/10.1215/15228517-2008-104
Di Giacomo, A. M., Valente, M., Cerase, A., Lofiego, M. F., Piazzini, F., Calabro, L., Gambale, E., Covre, A., & Maio, M. (2019). Immunotherapy of brain metastases: Breaking a “dogma.” Journal of Experimental & Clinical Cancer Research, 38(1), 419. https://doi.org/10.1186/s13046-019-1426-2
Stacker, S. A., Baldwin, M. E., & Achen, M. G. (2002). The role of tumor lymphangiogenesis in metastatic spread. The FASEB Journal, 16(9), 922–934. https://doi.org/10.1096/fj.01-0945rev
Entschladen, F., Palm, D., Lang, K., Drell, T. I. V., & Zaenker, K. S. (2006). Neoneurogenesis: Tumors may initiate their own innervation by the release of neurotrophic factors in analogy to lymphangiogenesis and neoangiogenesis. Medical Hypotheses, 67(1), 33–35. https://doi.org/10.1016/j.mehy.2006.01.015
Madden, K. S., Szpunar, M. J., & Brown, E. B. (2011). β-Adrenergic receptors (β-AR) regulate VEGF and IL-6 production by divergent pathways in high β-AR-expressing breast cancer cell lines. Breast Cancer Res Tr, 130(3), 747–758. https://doi.org/10.1007/s10549-011-1348-y
Chen, H., Liu, D., Yang, Z., Sun, L., Deng, Q., Yang, S., Qian, L., Guo, L., Yu, M., Hu, M., Shi, M., & Guo, N. (2014). Adrenergic signaling promotes angiogenesis through endothelial cell-tumor cell crosstalk. Endocrine-Related Cancer, 21(5), 783–795. https://doi.org/10.1530/ERC-14-0236
Dantzer, R. (2018). Neuroimmune interactions: From the brain to the immune system and vice versa. Physiological Reviews, 98(1), 477–504. https://doi.org/10.1152/physrev.00039.2016
Sloan, E. K., Priceman, S. J., Cox, B. F., Yu, S., Pimentel, M. A., Tangkanangnukul, V., Arevalo, J. M., Morizono, K., Karanikolas, B. D., Wu, L., Sood, A. K., & Cole, S. W. (2010). The sympathetic nervous system induces a metastatic switch in primary breast cancer. Cancer Research, 70(18), 7042–7052. https://doi.org/10.1158/0008-5472.CAN-10-0522
Bonaz, B., Sinniger, V., & Pellissier, S. (2016). Anti-inflammatory properties of the vagus nerve: Potential therapeutic implications of vagus nerve stimulation. J Physiol-London, 594(20), 5781–5790. https://doi.org/10.1113/Jp271539
Kawashima, K., Yoshikawa, K., Fujii, Y. X., Moriwaki, Y., & Misawa, H. (2007). Expression and function of genes encoding cholinergic components in murine immune cells. Life Sciences, 80(24–25), 2314–2319. https://doi.org/10.1016/j.lfs.2007.02.036
Coleridge, J. C., & Coleridge, H. M. (1984). Afferent vagal C fibre innervation of the lungs and airways and its functional significance. Reviews of Physiology Biochemistry and Pharmacology, 99, 1–110. https://doi.org/10.1007/BFb0027715
Erin, N., Duymus, O., Ozturk, S., & Demir, N. (2012). Activation of vagus nerve by semapimod alters substance P levels and decreases breast cancer metastasis. Regulatory Peptides, 179(1–3), 101–108. https://doi.org/10.1016/j.regpep.2012.08.001
Erin, N., Boyer, P. J., Bonneau, R. H., Clawson, G. A., & Welch, D. R. (2004). Capsaicin-mediated denervation of sensory neurons promotes mammary tumor metastasis to lung and heart. Anticancer Research, 24(2B), 1003–1009.
Chavan, S. S., Pavlov, V. A., & Tracey, K. J. (2017). Mechanisms and therapeutic relevance of neuro-immune communication. Immunity, 46(6), 927–942. https://doi.org/10.1016/j.immuni.2017.06.008
Mueller, S. N. (2022). Neural control of immune cell trafficking. J Exp Med, 219(3). https://doi.org/10.1084/jem.20211604
Gautam J, Banskota S, Regmi SC, Ahn S, Jeon YH, Jeong H, Kim SJ, Nam TG, Jeong BS, & Kim JA (2016). Tryptophan hydroxylase 1 and 5-HT7 receptor preferentially expressed in triple-negative breast cancer promote cancer progression through autocrine serotonin signaling. Mol Cancer, 15. https://doi.org/10.1186/s12943-016-0559-6
Fernandez-Nogueira, P., Noguera-Castells, A., Fuster, G., Recalde-Percaz, L., Moragas, N., Lopez-Plana, A., Enreig, E., Jauregui, P., Carbo, N., Almendro, V., Gascon, P., Bragado, P., & Mancino, M. (2018). Histamine receptor 1 inhibition enhances antitumor therapeutic responses through extracellular signal-regulated kinase (ERK) activation in breast cancer. Cancer Letters, 424, 70–83. https://doi.org/10.1016/j.canlet.2018.03.014
Rzeski W, Ikonomidou C, & Turski L (2002). Glutamate antagonists limit tumor growth. Biochem Pharmacol, 64(8):1195–1200. Pii S0006–2952(02)01218–2 Doi https://doi.org/10.1016/S0006-2952(02)01218-2
Deshmukh A, Deshpande K, Arfuso F, Newsholme P, & Dharmarajan A (2016). Cancer stem cell metabolism: A potential target for cancer therapy. Mol Cancer, 15. ARTN 69 https://doi.org/10.1186/s12943-016-0555-x
Li, X. Y., Wang, H. R., Yang, X., Wang, X. Q., Zhao, L. A., Zou, L., Yang, Q., Hou, Z. L., Tan, J., Zhang, H. L., Nie, J. Y., & Jiao, B. W. (2021). GABRP sustains the stemness of triple-negative breast cancer cells through EGFR signaling. Cancer Letters, 514, 90–102. https://doi.org/10.1016/j.canlet.2021.04.028
Feng, X. L., Wu, Z. J., Wu, Y. S., Hankey, W., Prior, T. W., Li, L., Ganju, R. K., Shen, R. L., & Zou, X. H. (2011). Cdc25A regulates matrix metalloprotease 1 through Foxo1 and mediates metastasis of breast cancer cells. Molecular and Cellular Biology, 31(16), 3457–3471. https://doi.org/10.1128/Mcb.05523-11
Ciccarone, F., Di Leo, L., Lazzarino, G., Maulucci, G., Di Giacinto, F., Tavazzi, B., & Ciriolo, M. R. (2020). Aconitase 2 inhibits the proliferation of MCF-7 cells promoting mitochondrial oxidative metabolism and ROS/FoxO1-mediated autophagic response. Brit J Cancer, 122(2), 182–193. https://doi.org/10.1038/s41416-019-0641-0
Shurin, M. R., Shurin, G. V., Zlotnikov, S. B., & Bunimovich, Y. L. (2020). The neuroimmune axis in the tumor microenvironment. The Journal of Immunology, 204(2), 280–285. https://doi.org/10.4049/jimmunol.1900828
Magaway, C., Kim, E., & Jacinto, E. (2019). Targeting mTOR and metabolism in cancer: Lessons and innovations. Cells, 8(12). https://doi.org/10.3390/cells8121584
Switzer, C. H., Glynn, S. A., Ridnour, L. A., Cheng, R. Y., Vitek, M. P., Ambs, S., & Wink, D. A. (2011). Nitric oxide and protein phosphatase 2A provide novel therapeutic opportunities in ER-negative breast cancer. Trends in Pharmacological Sciences, 32(11), 644–651. https://doi.org/10.1016/j.tips.2011.07.001
Silverman, D. A., Martinez, V. K., Dougherty, P. M., Myers, J. N., Calin, G. A., & Amit, M. (2021). Cancer-associated neurogenesis and nerve-cancer cross-talk. Cancer Research, 81(6), 1431–1440. https://doi.org/10.1158/0008-5472.CAN-20-2793
Krizanova, O., Babula, P., & Pacak, K. (2016). Stress, catecholaminergic system and cancer. Stress, 19(4), 419–428. https://doi.org/10.1080/10253890.2016.1203415
De Blasi, A. (1990). Beta-adrenergic receptors: Structure, function and regulation. Drugs Under Experimental and Clinical Research, 16(3), 107–112.
Payton, S. (2011). Targeted therapies: Can sunitinib use be expanded to other cancers? Nature Reviews. Urology, 9(1), 3. https://doi.org/10.1038/nrurol.2011.207
Park, S. Y., Kang, J. H., Jeong, K. J., Lee, J., Han, J. W., Choi, W. S., Kim, Y. K., Kang, J., Park, C. G., & Lee, H. Y. (2011). Norepinephrine induces VEGF expression and angiogenesis by a hypoxia-inducible factor-1α protein-dependent mechanism. International Journal of Cancer, 128(10), 2306–2316. https://doi.org/10.1002/ijc.25589
Powe, D. G., Voss, M. J., Zanker, K. S., Habashy, H. O., Green, A. R., Ellis, I. O., & Entschladen, F. (2010). Beta-blocker drug therapy reduces secondary cancer formation in breast cancer and improves cancer specific survival. Oncotarget, 1(7), 628–638. https://doi.org/10.18632/oncotarget.101009
Lee, J. W., Shahzad, M. M., Lin, Y. G., Armaiz-Pena, G., Mangala, L. S., Han, H. D., Kim, H. S., Nam, E. J., Jennings, N. B., Halder, J., Nick, A. M., Stone, R. L., Lu, C., Lutgendorf, S. K., Cole, S. W., Lokshin, A. E., & Sood, A. K. (2009). Surgical stress promotes tumor growth in ovarian carcinoma. Clinical Cancer Research, 15(8), 2695–2702. https://doi.org/10.1158/1078-0432.CCR-08-2966
Akbar, S., & Alsharidah, M. S. (2014). Are beta blockers new potential anticancer agents? Asian Pacific Journal of Cancer Prevention, 15(22), 9567–9574. https://doi.org/10.7314/apjcp.2014.15.22.9567
Nuevo-Tapioles, C., Santacatterina, F., Stamatakis, K., Nunez de Arenas, C., Gomez de Cedron, M., Formentini, L., & Cuezva, J. M. (2020). Coordinate β-adrenergic inhibition of mitochondrial activity and angiogenesis arrest tumor growth. Nature Communications, 11(1), 3606. https://doi.org/10.1038/s41467-020-17384-1
De Bock, K., Georgiadou, M., Schoors, S., Kuchnio, A., Wong, B. W., Cantelmo, A. R., Quaegebeur, A., Ghesquiere, B., Cauwenberghs, S., Eelen, G., Phng, L. K., Betz, I., Tembuyser, B., Brepoels, K., Welti, J., Geudens, I., Segura, I., Cruys, B., Bifari, F., … Carmeliet, P. (2013). Role of PFKFB3-driven glycolysis in vessel sprouting. Cell, 154(3), 651–663. https://doi.org/10.1016/j.cell.2013.06.037
Szpunar, M. J., Burke, K. A., Dawes, R. P., Brown, E. B., & Madden, K. S. (2013). The antidepressant desipramine and α2-adrenergic receptor activation promote breast tumor progression in association with altered collagen structure. Cancer Prevention Research (Philadelphia, Pa.), 6(12), 1262–1272. https://doi.org/10.1158/1940-6207.CAPR-13-0079
Lamkin, D. M., Sung, H. Y., Yang, G. S., David, J. M., Ma, J. C., Cole, S. W., & Sloan, E. K. (2015). α2-Adrenergic blockade mimics the enhancing effect of chronic stress on breast cancer progression. Psychoneuroendocrinology, 51, 262–270. https://doi.org/10.1016/j.psyneuen.2014.10.004
Wong, H. P. S., Li, Z. J., Shin, V. Y., Tai, E. K. K., Wu, W. K. K., Yu, L., & Cho, C. H. (2009). Effects of cigarette smoking and restraint stress on human colon tumor growth in mice. Digestion, 80(4), 209–214. https://doi.org/10.1159/000231898
Wei, P. L., Hung, C. S., & Chang, Y. J. (2012). The alpha9 nicotinic acetylcholine receptor is the key mediator in nicotine-enhanced cancer metastasis in breast cancer cells. Cancer Research, 72. https://doi.org/10.1158/1538-7445.Am2012-456
Jimenez, E., & Montiel, M. (2005). Activation of MAP kinase by muscarinic cholinergic receptors induces cell proliferation and protein synthesis in human breast cancer cells. Journal of Cellular Physiology, 204(2), 678–686. https://doi.org/10.1002/jcp.20326
Bucsek, M. J., Qiao, G., MacDonald, C. R., Giridharan, T., Evans, L., Niedzwecki, B., Liu, H., Kokolus, K. M., Eng, J. W., Messmer, M. N., Attwood, K., Abrams, S. I., Hylander, B. L., & Repasky, E. A. (2017). β-Adrenergic signaling in mice housed at standard temperatures suppresses an effector phenotype in CD8+ T cells and undermines checkpoint inhibitor therapy. Cancer Research, 77(20), 5639–5651. https://doi.org/10.1158/0008-5472.CAN-17-0546
Bakhtou, H., Olfatbakhsh, A., Deezagi, A., & Ahangari, G. (2019). The expression of dopamine receptors gene and their potential role in targeting breast cancer cells with selective agonist and antagonist drugs. Could it be the novel insight to therapy? Current Drug Discovery Technologies, 16(2), 184–197. https://doi.org/10.2174/1570163815666180130101421
Borcherding, D. C., Tong, W., Hugo, E. R., Barnard, D. F., Fox, S., LaSance, K., Shaughnessy, E., & Ben-Jonathan, N. (2016). Expression and therapeutic targeting of dopamine receptor-1 (D1R) in breast cancer. Oncogene, 35(24), 3103–3113. https://doi.org/10.1038/onc.2015.369
Asada, M., Ebihara, S., Numachi, Y., Okazaki, T., Yamanda, S., Ikeda, K., Yasuda, H., Sora, I., & Arai, H. (2008). Reduced tumor growth in a mouse model of schizophrenia, lacking the dopamine transporter. International Journal of Cancer, 123(3), 511–518. https://doi.org/10.1002/ijc.23562
Chakroborty, D., Chowdhury, U. R., Sarkar, C., Baral, R., Dasgupta, P. S., & Basu, S. (2008). Dopamine regulates endothelial progenitor cell mobilization from mouse bone marrow in tumor vascularization. Journal of Clinical Investigation, 118(4), 1380–1389. https://doi.org/10.1172/Jci33125
Wang, P. S., Walker, A. M., Tsuang, M. T., Orav, E. J., Glynn, R. J., Levin, R., & Avorn, J. (2002). Dopamine antagonists and the development of breast cancer. Archives of General Psychiatry, 59(12), 1147–1154. https://doi.org/10.1001/archpsyc.59.12.1147
Sarkar, C., Chakroborty, D., Chowdhury, U. R., Dasgupta, P. S., & Basu, S. (2008). Dopamine increases the efficacy of anticancer drugs in breast and colon cancer preclinical models. Clinical Cancer Research, 14(8), 2502–2510. https://doi.org/10.1158/1078-0432.Ccr-07-1778
Arese, M., Bussolino, F., Pergolizzi, M., Bizzozero, L., & Pascal, D. (2018). Tumor progression: The neuronal input. Ann Transl Med, 6(5):89. https://doi.org/10.21037/atm.2018.01.01
Li, J., Yao, Q. Y., Xue, J. S., Wang, L. J., Yuan, Y., Tian, X. Y., Su, H., Wang, S. Y., Chen, W. J., Lu, W., & Zhou, T. Y. (2017). Dopamine D2 receptor antagonist sulpiride enhances dexamethasone responses in the treatment of drug-resistant and metastatic breast cancer. Acta Pharmacologica Sinica, 38(9), 1282–1296. https://doi.org/10.1038/aps.2017.24
Wang, S., Mou, Z., Ma, Y., Li, J., Li, J., Ji, X., Wu, K., Li, L., Lu, W., & Zhou, T. (2015). Dopamine enhances the response of sunitinib in the treatment of drug-resistant breast cancer: Involvement of eradicating cancer stem-like cells. Biochemical Pharmacology, 95(2), 98–109. https://doi.org/10.1016/j.bcp.2015.03.013
Rosas-Cruz, A., Salinas-Jazmin, N., & Velasco-Velazquez, M. A. (2021). Dopamine receptors in cancer: Are they valid therapeutic targets? Technology in Cancer Research and Treatment, 20, 15330338211027912. https://doi.org/10.1177/15330338211027913
Roy, S., Lu, K., Nayak, M. K., Bhuniya, A., Ghosh, T., Kundu, S., Ghosh, S., Baral, R., Dasgupta, P. S., & Basu, S. (2017). Activation of D2 dopamine receptors in CD133+ve cancer stem cells in non-small cell lung carcinoma inhibits proliferation, clonogenic ability, and invasiveness of these cells. Journal of Biological Chemistry, 292(2), 435–445. https://doi.org/10.1074/jbc.M116.748970
Leng, Z. G., Lin, S. J., Wu, Z. R., Guo, Y. H., Cai, L., Shang, H. B., Tang, H., Xue, Y. J., Lou, M. Q., Zhao, W., Le, W. D., Zhao, W. G., Zhang, X., & Wu, Z. B. (2017). Activation of DRD5 (dopamine receptor D5) inhibits tumor growth by autophagic cell death. Autophagy, 13(8), 1404–1419. https://doi.org/10.1080/15548627.2017.1328347
Jamu, I. M., & Okamoto, H. (2022). Recent advances in understanding adverse effects associated with drugs targeting the serotonin receptor, 5-HT GPCR. Frontiers in Global Women’s Health, 3, 1012463. https://doi.org/10.3389/fgwh.2022.1012463
Zhang, Y., Dijkman, P. M., Zou, R., Zandl-Lang, M., Sanchez, R. M., Eckhardt-Strelau, L., Kofeler, H., Vogel, H., Yuan, S., & Kudryashev, M. (2021). Asymmetric opening of the homopentameric 5-HT(3A) serotonin receptor in lipid bilayers. Nature Communications, 12(1), 1074. https://doi.org/10.1038/s41467-021-21016-7
Pai, V. P., Marshall, A. M., Hernandez, L. L., Buckley, A. R., & Horseman, N. D. (2009). Altered serotonin physiology in human breast cancers favors paradoxical growth and cell survival. Breast Cancer Research, 11(6), R81. https://doi.org/10.1186/bcr2448
Flamand, V., Zhao, H., & Peehl, D. M. (2010). Targeting monoamine oxidase A in advanced prostate cancer. Journal of Cancer Research and Clinical Oncology, 136(11), 1761–1771. https://doi.org/10.1007/s00432-010-0835-6
Satram-Maharaj, T., Nyarko, J. N. K., Kuski, K., Fehr, K., Pennington, P. R., Truitt, L., Freywald, A., Lukong, K. E., Anderson, D. H., & Mousseau, D. D. (2014). The monoamine oxidase-A inhibitor clorgyline promotes a mesenchymal-to-epithelial transition in the MDA-MB-231 breast cancer cell line. Cellular Signalling, 26(12), 2621–2632. https://doi.org/10.1016/j.cellsig.2014.08.005
Kuol, N., Stojanovska, L., Apostolopoulos, V., & Nurgali, K. (2018). Role of the nervous system in tumor angiogenesis. Cancer Microenvironment, 11(1), 1–11. https://doi.org/10.1007/s12307-018-0207-3
Gwynne, W., Shakeel, M. S., Wu, J. H., Hallett, R., Girgis-Gabardo, A., Dvorkin-Gheva, A., & Hassell, J. A. (2019). Monoamine oxidase-A activity is required for clonal tumorsphere formation by human breast tumor cells. Cell Mol Biol Lett, 24(1). https://doi.org/10.1186/s11658-019-0183-8
Hallett, R. M., Girgis-Gabardo, A., Gwynne, W. D., Giacomelli, A. O., Bisson, J. N., Jensen, J. E., Dvorkin-Gheva, A., & Hassell, J. A. (2016). Serotonin transporter antagonists target tumor-initiating cells in a transgenic mouse model of breast cancer. Oncotarget, 7(33), 53137–53152. https://doi.org/10.18632/oncotarget.10614
Fischer, A., Rennert, H. S., & Rennert, G. (2022). Selective serotonin reuptake inhibitors associated with increased mortality risk in breast cancer patients in northern Israel. International Journal of Epidemiology. https://doi.org/10.1093/ije/dyac004
Rogers, L. Q., Courneya, K. S., Anton, P. M., Verhulst, S., Vicari, S. K., Robbs, R. S., & McAuley, E. (2017). Effects of a multicomponent physical activity behavior change intervention on fatigue, anxiety, and depressive symptomatology in breast cancer survivors: Randomized trial. Psycho-Oncology, 26(11), 1901–1906. https://doi.org/10.1002/pon.4254
Liu, Q., Sun, H., Liu, Y., Li, X., Xu, B., Li, L., & Jin, W. (2022). HTR1A inhibits the progression of triple-negative breast cancer via TGF-β canonical and noncanonical pathways. Adv Sci (Weinh), 9(12), e2105672. https://doi.org/10.1002/advs.202105672
Gilardi, M., Ramos, M., & Hollern, D. (2022). B cells secrete GABA, which provokes a pro-tumor immune microenvironment. Cancer Cell, 40(1), 17–19. https://doi.org/10.1016/j.ccell.2021.12.007
Lu, R., Fan, C. W., Shangguan, W. Q., Liu, Y., Li, Y., Shang, Y. N., Yin, D. Q., Zhang, S. L., Huang, Q. R., Li, X., Meng, W. T., Xu, H., Zhou, Z. G., Hu, J. K., Li, W. M., Liu, L. X., & Mo, X. M. (2017). Neurons generated from carcinoma stem cells support cancer progression. Signal Transduct Tar, 2. https://doi.org/10.1038/sigtrans.2016.36
Zehentner, B. K., Dillon, D. C., Jiang, Y., Xu, J., Bennington, A., Molesh, D. A., Zhang, X., Reed, S. G., Persing, D., & Houghton, R. L. (2002). Application of a multigene reverse transcription-PCR assay for detection of mammaglobin and complementary transcribed genes in breast cancer lymph nodes. Clinical Chemistry, 48(8), 1225–1231.
McCallum, G. A., Shiralkar, J., Suciu, D., Covarrubias, G., Yu, J. S., Karathanasis, E., & Durand, D. M. (2020). Chronic neural activity recorded within breast tumors. Scientific Reports -Uk, 10(1). https://doi.org/10.1038/s41598-020-71670-y
Middelhoff, M., Westphalen, C. B., Hayakawa, Y., Yan, K. S., Gershon, M. D., Wang, T. C., & Quante, M. (2017). Dclk1-expressing tuft cells: Critical modulators of the intestinal niche? American Journal of Physiology-Gastrointestinal and Liver Physiology, 313(4), G285–G299. https://doi.org/10.1152/ajpgi.00073.2017
Lim, E., Vaillant, F., Wu, D., Forrest, N. C., Pal, B., Hart, A. H., Asselin-Labat, M. L., Gyorki, D. E., Ward, T., Partanen, A., Feleppa, F., Huschtscha, L. I., Thorne, H. J., Fox, S. B., Yan, M., French, J. D., Brown, M. A., Smyth, G. K., Visvader, J. E., & Lindeman, G. J. (2009). Aberrant luminal progenitors as the candidate target population for basal tumor development in BRCA1 mutation carriers. Nature Medicine, 15(8), 907–913. https://doi.org/10.1038/nm.2000
Christin, J. R., Wang, C. H., Chung, C. Y., Liu, Y., Dravis, C., Tang, W., Oktay, M. H., Wahl, G. M., & Guo, W. J. (2020). Stem cell determinant SOX9 promotes lineage plasticity and progression in basal-like breast cancer. Cell Reports, 31(10). https://doi.org/10.1016/j.celrep.2020.107742
Kwa, M. J., & Adams, S. (2018). Checkpoint inhibitors in triple-negative breast cancer (TNBC): Where to go from here. Cancer, 124(10), 2086–2103. https://doi.org/10.1002/cncr.31272
Wali, V. B., Patwardhan, G. A., Pelekanou, V., Karn, T., Cao, J., Ocana, A., Yan, Q., Nelson, B., Hatzis, C., & Pusztai, L. (2019). Identification and validation of a novel biologics target in triple negative breast cancer. Scientific Reports-Uk, 9. https://doi.org/10.1038/s41598-019-51453-w
Jin, L. T., Han, B. C., Siegel, E., Cui, Y. K., Giuliano, A., & Cui, X. J. (2018). Breast cancer lung metastasis: Molecular biology and therapeutic implications. Cancer Biology & Therapy, 19(10), 858–868. https://doi.org/10.1080/15384047.2018.1456599
Wang, Z., & Zhang, H. (2019). Phase separation, transition, and autophagic degradation of proteins in development and pathogenesis. Trends in Cell Biology, 29(5), 417–427. https://doi.org/10.1016/j.tcb.2019.01.008
Hutchings, C., Phillips, J. A., & Djamgoz, M. B. A. (2020). Nerve input to tumours: Pathophysiological consequences of a dynamic relationship. Biochimica et Biophysica Acta - Reviews on Cancer, 1874(2), 188411. https://doi.org/10.1016/j.bbcan.2020.188411
Thomas, M. L., de Antueno, R., Coyle, K. M., Sultan, M., Cruickshank, B. M., Giacomantonio, M. A., Giacomantonio, C. A., Duncan, R., & Marcato, P. (2016). Citral reduces breast tumor growth by inhibiting the cancer stem cell marker ALDH1A3. Molecular Oncology, 10(9), 1485–1496. https://doi.org/10.1016/j.molonc.2016.08.004
Vidovic, D., Huynh, T. T., Konda, P., Dean, C., Cruickshank, B. M., Sultan, M., Coyle, K. M., Gujar, S., & Marcato, P. (2020). ALDH1A3-regulated long non-coding RNA NRAD1 is a potential novel target for triple-negative breast tumors and cancer stem cells. Cell Death and Differentiation, 27(1), 363–378. https://doi.org/10.1038/s41418-019-0362-1
Huang, Y., Pledgie, A., Casero, R. A., Jr., & Davidson, N. E. (2005). Molecular mechanisms of polyamine analogs in cancer cells. Anti-Cancer Drugs, 16(3), 229–241. https://doi.org/10.1097/00001813-200503000-00002
Gerner, E. W. (2010). Cancer chemoprevention locks onto a new polyamine metabolic target. Cancer Prevention Research (Philadelphia, Pa.), 3(2), 125–127. https://doi.org/10.1158/1940-6207.CAPR-09-0252
Walls, A. B., Waagepetersen, H. S., Bak, L. K., Schousboe, A., & Sonnewald, U. (2015). The glutamine-glutamate/GABA cycle: Function, regional differences in glutamate and GABA production and effects of interference with GABA metabolism. Neurochemical Research, 40(2), 402–409. https://doi.org/10.1007/s11064-014-1473-1
Guyon, A. (2014). Baclofen and other GABAB receptor agents are allosteric modulators of the CXCL12 chemokine receptor CXCR4. Medical Science (Paris), 30(1), 9–12. https://doi.org/10.1051/medsci/20143001002
Stepulak, A., Luksch, H., Uckermann, O., Sifringer, M., Rzeski, W., Polberg, K., Kupisz, K., Klatka, J., Kielbus, M., Grabarska, A., Marzahn, J., Turski, L., & Ikonomidou, C. (2011). Glutamate receptors in laryngeal cancer cells. Anticancer Research, 31(2), 565–573.
Yi, H., Talmon, G., & Wang, J. (2019). Glutamate in cancers: From metabolism to signaling. Journal of Biomedical Research, 34(4), 260–270. https://doi.org/10.7555/JBR.34.20190037
Budczies, J., Pfitzner, B. M., Gyorffy, B., Winzer, K. J., Radke, C., Dietel, M., Fiehn, O., & Denkert, C. (2015). Glutamate enrichment as new diagnostic opportunity in breast cancer. International Journal of Cancer, 136(7), 1619–1628. https://doi.org/10.1002/ijc.29152
Fazzari, J., Lin, H., Murphy, C., Ungard, R., & Singh, G. (2015). Inhibitors of glutamate release from breast cancer cells; new targets for cancer-induced bone-pain. Science and Reports, 5, 8380. https://doi.org/10.1038/srep08380
Willard, S. S., & Koochekpour, S. (2013). Glutamate, glutamate receptors, and downstream signaling pathways. International Journal of Biological Sciences, 9(9), 948–959. https://doi.org/10.7150/ijbs.6426
Traynelis, S. F., Wollmuth, L. P., McBain, C. J., Menniti, F. S., Vance, K. M., Ogden, K. K., Hansen, K. B., Yuan, H., Myers, S. J., & Dingledine, R. (2010). Glutamate receptor ion channels: Structure, regulation, and function. Pharmacological Reviews, 62(3), 405–496. https://doi.org/10.1124/pr.109.002451
Reichardt, L. F. (2006). Neurotrophin-regulated signalling pathways. Philosophical Transactions of the Royal Society of London. Series B, Biological sciences, 361(1473), 1545–1564. https://doi.org/10.1098/rstb.2006.1894
Deutsch, S. I., Tang, A. H., Burket, J. A., & Benson, A. D. (2014). NMDA receptors on the surface of cancer cells: Target for chemotherapy? Biomedicine & Pharmacotherapy, 68(4), 493–496. https://doi.org/10.1016/j.biopha.2014.03.012
Cervantes-Villagrana, R. D., Albores-Garcia, D., Cervantes-Villagrana, A. R., & Garcia-Acevez, S. J. (2020). Tumor-induced neurogenesis and immune evasion as targets of innovative anti-cancer therapies. Signal Transduct Tar, 5(1). https://doi.org/10.1038/s41392-020-0205-z
Banda, M., Speyer, C. L., Semma, S. N., Osuala, K. O., Kounalakis, N., Torres Torres, K. E., Barnard, N. J., Kim, H. J., Sloane, B. F., Miller, F. R., Goydos, J. S., & Gorski, D. H. (2014). Metabotropic glutamate receptor-1 contributes to progression in triple negative breast cancer. PLoS ONE, 9(1), e81126. https://doi.org/10.1371/journal.pone.0081126
Sexton, R. E., Hachem, A. H., Assi, A. A., Bukhsh, M. A., Gorski, D. H., & Speyer, C. L. (2018). Metabotropic glutamate receptor-1 regulates inflammation in triple negative breast cancer. Science and Reports, 8(1), 16008. https://doi.org/10.1038/s41598-018-34502-8
Teh, J. L., Shah, R., La Cava, S., Dolfi, S. C., Mehta, M. S., Kongara, S., Price, S., Ganesan, S., Reuhl, K. R., Hirshfield, K. M., Karantza, V., & Chen, S. (2015). Metabotropic glutamate receptor 1 disrupts mammary acinar architecture and initiates malignant transformation of mammary epithelial cells. Breast Cancer Research and Treatment, 151(1), 57–73. https://doi.org/10.1007/s10549-015-3365-8
Sankhe, R., Pai, S. R. K., & Kishore, A. (2021). Tumour suppression through modulation of neprilysin signaling: A comprehensive review. European Journal of Pharmacology, 891, 173727. https://doi.org/10.1016/j.ejphar.2020.173727
Mutrie, N., Campbell, A., Barry, S., Hefferon, K., McConnachie, A., Ritchie, D., & Tovey, S. (2012). Five-year follow-up of participants in a randomised controlled trial showing benefits from exercise for breast cancer survivors during adjuvant treatment. Are there lasting effects? Journal of Cancer Survivorship, 6(4), 420–430. https://doi.org/10.1007/s11764-012-0233-y
Yang, C. Y., Tsai, J. C., Huang, Y. C., & Lin, C. C. (2011). Effects of a home-based walking program on perceived symptom and mood status in postoperative breast cancer women receiving adjuvant chemotherapy. Journal of Advanced Nursing, 67(1), 158–168. https://doi.org/10.1111/j.1365-2648.2010.05492.x
Diggins, A. D., Hearn, L. E., Lechner, S. C., Annane, D., Antoni, M. H., & Whitehead, N. E. (2017). Physical activity in Black breast cancer survivors: Implications for quality of life and mood at baseline and 6-month follow-up. Psycho-Oncology, 26(6), 822–828. https://doi.org/10.1002/pon.4095
Sadoughi, F., Maleki Dana, P., Homayoonfal, M., Sharifi, M., & Asemi, Z. (2022). Molecular basis of melatonin protective effects in metastasis: A novel target of melatonin. Biochimie. https://doi.org/10.1016/j.biochi.2022.05.012
Junior, R. P., Chuffa, L. G. A., Simao, V. A., Sonehara, N. M., Chammas, R., Reiter, R. J., & Zuccari, D. (2022). Melatonin regulates the daily levels of plasma amino acids, acylcarnitines, biogenic amines, sphingomyelins, and hexoses in a xenograft model of triple negative breast cancer. Int J Mol Sci, 23(16). https://doi.org/10.3390/ijms23169105
Onder, G. O., Sezer, G., Ozdamar, S., & Yay, A. (2022). Melatonin has an inhibitory effect on MCF-7 and MDA-MB-231 human breast cancer cell lines by inducing autophagy and apoptosis. Fundamental & Clinical Pharmacology. https://doi.org/10.1111/fcp.12813
Davoodvandi, A., Nikfar, B., Reiter, R. J., & Asemi, Z. (2022). Melatonin and cancer suppression: Insights into its effects on DNA methylation. Cellular & Molecular Biology Letters, 27(1), 73. https://doi.org/10.1186/s11658-022-00375-z
Alonso-Gonzalez, C., Gonzalez-Abalde, C., Menendez-Menendez, J., Gonzalez-Gonzalez, A., Alvarez-Garcia, V., Gonzalez-Cabeza, A., Martinez-Campa, C., & Cos, S. (2022). Melatonin modulation of radiation-induced molecular changes in MCF-7 human breast cancer cells. Biomedicines, 10(5). https://doi.org/10.3390/biomedicines10051088
Diamantopoulou, Z., Castro-Giner, F., Schwab, F. D., Foerster, C., Saini, M., Budinjas, S., Strittmatter, K., Krol, I., Seifert, B., Heinzelmann-Schwarz, V., Kurzeder, C., Rochlitz, C., Vetter, M., Weber, W. P., & Aceto, N. (2022). The metastatic spread of breast cancer accelerates during sleep. Nature, 607(7917), 156–162. https://doi.org/10.1038/s41586-022-04875-y
Lin, S. X., Chen, J., Mazumdar, M., Poirier, D., Wang, C., Azzi, A., & Zhou, M. (2010). Molecular therapy of breast cancer: Progress and future directions. Nature Reviews Endocrinology, 6(9), 485–493. https://doi.org/10.1038/nrendo.2010.92
Schecterson, L. C., & Bothwell, M. (2010). Neurotrophin receptors: Old friends with new partners. Developmental Neurobiology, 70(5), 332–338. https://doi.org/10.1002/dneu.20767
Bartkowska, K., Turlejski, K., & Djavadian, R. L. (2010). Neurotrophins and their receptors in early development of the mammalian nervous system. Acta Neurobiologiae Experimentalis, 70(4), 454–467.
Gibson, E. M., Purger, D., Mount, C. W., Goldstein, A. K., Lin, G. L., Wood, L. S., Inema, I., Miller, S. E., Bieri, G., Zuchero, J. B., Barres, B. A., Woo, P. J., Vogel, H., & Monje, M. (2014). Neuronal activity promotes oligodendrogenesis and adaptive myelination in the mammalian brain. Science, 344(6183), 487. https://doi.org/10.1126/science.1252304
Tilan, J., & Kitlinska, J. (2010). Sympathetic neurotransmitters and tumor angiogenesis-link between stress and cancer progression. J Oncol, 2010, 539706. https://doi.org/10.1155/2010/539706
Kim, J., Villadsen, R., Sorlie, T., Fogh, L., Gronlund, S. Z., Fridriksdottir, A. J., Kuhn, I., Rank, F., Wielenga, V. T., Solvang, H., Edwards, P. A., Borresen-Dale, A. L., Ronnov-Jessen, L., Bissell, M. J., & Petersen, O. W. (2012). Tumor initiating but differentiated luminal-like breast cancer cells are highly invasive in the absence of basal-like activity. Proc Natl Acad Sci U S A, 109(16), 6124–6129. https://doi.org/10.1073/pnas.1203203109
Edelmann, E., Lessmann, V., & Brigadski, T. (2014). Pre- and postsynaptic twists in BDNF secretion and action in synaptic plasticity. Neuropharmacology, 76 Pt C, 610–627. https://doi.org/10.1016/j.neuropharm.2013.05.043
Bartkowska, K., Paquin, A., Gauthier, A. S., Kaplan, D. R., & Miller, F. D. (2007). Trk signaling regulates neural precursor cell proliferation and differentiation during cortical development. Development, 134(24), 4369–4380. https://doi.org/10.1242/dev.008227
Lin, P. Y., Kavalali, E. T., & Monteggia, L. M. (2018). Genetic dissection of presynaptic and postsynaptic BDNF-TrkB signaling in synaptic efficacy of CA3-CA1 synapses. Cell Reports, 24(6), 1550–1561. https://doi.org/10.1016/j.celrep.2018.07.020
Colucci-D'Amato, L., Speranza, L., & Volpicelli, F. (2020). Neurotrophic factor BDNF, physiological functions and therapeutic potential in depression, neurodegeneration and brain cancer. International Journal of Molecular Sciences, 21(20). https://doi.org/10.3390/ijms21207777
Wang, H., Ward, N., Boswell, M., & Katz, D. M. (2006). Secretion of brain-derived neurotrophic factor from brain microvascular endothelial cells. European Journal of Neuroscience, 23(6), 1665–1670. https://doi.org/10.1111/j.1460-9568.2006.04682.x
Nakahashi, T., Fujimura, H., Altar, C. A., Li, J., Kambayashi, J., Tandon, N. N., & Sun, B. (2000). Vascular endothelial cells synthesize and secrete brain-derived neurotrophic factor. FEBS Letters, 470(2), 113–117. https://doi.org/10.1016/s0014-5793(00)01302-8
Yang, X., Martin, T. A., & Jiang, W. G. (2012). Biological influence of brain-derived neurotrophic factor on breast cancer cells. International Journal of Oncology, 41(4), 1541–1546. https://doi.org/10.3892/ijo.2012.1581
Tsai, Y. F., Tseng, L. M., Hsu, C. Y., Yang, M. H., Chiu, J. H., & Shyr, Y. M. (2017). Brain-derived neurotrophic factor (BDNF) -TrKB signaling modulates cancer-endothelial cells interaction and affects the outcomes of triple negative breast cancer. PLoS ONE, 12(6), e0178173. https://doi.org/10.1371/journal.pone.0178173
Tajbakhsh, A., Mokhtari-Zaer, A., Rezaee, M., Afzaljavan, F., Rivandi, M., Hassanian, S. M., Ferns, G. A., Pasdar, A., & Avan, A. (2017). Therapeutic potentials of BDNF/TrkB in breast cancer; current status and perspectives. Journal of Cellular Biochemistry, 118(9), 2502–2515. https://doi.org/10.1002/jcb.25943
Contreras-Zarate, M. J., Day, N. L., Ormond, D. R., Borges, V. F., Tobet, S., Gril, B., Steeg, P. S., & Cittelly, D. M. (2019). Estradiol induces BDNF/TrkB signaling in triple-negative breast cancer to promote brain metastases. Oncogene, 38(24), 4685–4699. https://doi.org/10.1038/s41388-019-0756-z
Liu, X., McMurphy, T., Xiao, R., Slater, A., Huang, W., & Cao, L. (2014). Hypothalamic gene transfer of BDNF inhibits breast cancer progression and metastasis in middle age obese mice. Molecular Therapy, 22(7), 1275–1284. https://doi.org/10.1038/mt.2014.45
Descamps, S., Toillon, R. A., Adriaenssens, E., Pawlowski, V., Cool, S. M., Nurcombe, V., Le Bourhis, X. F., Boilly, B., Peyrat, J. P., & Hondermarck, H. (2001). Nerve growth factor stimulates proliferation and survival of human breast cancer cells through two distinct signaling pathways. Journal of Biological Chemistry, 276(21), 17864–17870. https://doi.org/10.1074/jbc.M010499200
Louie, E., Chen, X. F., Coomes, A., Ji, K., Tsirka, S., & Chen, E. (2013). Neurotrophin-3 modulates breast cancer cells and the microenvironment to promote the growth of breast cancer brain metastasis. Oncogene, 32(35), 4064–4077. https://doi.org/10.1038/onc.2012.417
Rodriguez, P. L., Jiang, S. X., Fu, Y. G., Avraham, S., & Avraham, H. K. (2014). The proinflammatory peptide substance P promotes blood-brain barrier breaching by breast cancer cells through changes in microvascular endothelial cell tight junctions. International Journal of Cancer, 134(5), 1034–1044. https://doi.org/10.1002/ijc.28433
Skaper, S. D. (2012). The neurotrophin family of neurotrophic factors: An overview. Methods in Molecular Biology, 846, 1–12. https://doi.org/10.1007/978-1-61779-536-7_1
Meldolesi, J. (2018). Neurotrophin Trk receptors: New targets for cancer therapy. Reviews of Physiology Biochemistry and Pharmacology, 174, 67–79. https://doi.org/10.1007/112_2017_6
Rolfo, C., Ruiz, R., Giovannetti, E., Gil-Bazo, I., Russo, A., Passiglia, F., Giallombardo, M., Peeters, M., & Raez, L. (2015). Entrectinib: A potent new TRK, ROS1, and ALK inhibitor. Expert Opinion on Investigational Drugs, 24(11), 1493–1500. https://doi.org/10.1517/13543784.2015.1096344
Hong, S., Kim, J., Seo, J. H., Jung, K. H., Hong, S. S., & Hong, S. (2012). Design, synthesis, and evaluation of 3,5-disubstituted 7-azaindoles as Trk inhibitors with anticancer and antiangiogenic activities. Journal of Medicinal Chemistry, 55(11), 5337–5349. https://doi.org/10.1021/jm3002982
Doebele, R. C., Davis, L. E., Vaishnavi, A., Le, A. T., Estrada-Bernal, A., Keysar, S., Jimeno, A., Varella-Garcia, M., Aisner, D. L., Li, Y., Stephens, P. J., Morosini, D., Tuch, B. B., Fernandes, M., Nanda, N., & Low, J. A. (2015). An oncogenic NTRK fusion in a patient with soft-tissue sarcoma with response to the tropomyosin-related kinase inhibitor LOXO-101. Cancer Discovery, 5(10), 1049–1057. https://doi.org/10.1158/2159-8290.CD-15-0443
Russo, M., Misale, S., Wei, G., Siravegna, G., Crisafulli, G., Lazzari, L., Corti, G., Rospo, G., Novara, L., Mussolin, B., Bartolini, A., Cam, N., Patel, R., Yan, S., Shoemaker, R., Wild, R., Di Nicolantonio, F., Bianchi, A. S., Li, G., … Bardelli, A. (2016). Acquired resistance to the TRK inhibitor entrectinib in colorectal cancer. Cancer Discovery, 6(1), 36–44. https://doi.org/10.1158/2159-8290.CD-15-0940
Kefeli, U., Ucuncu Kefeli, A., Cabuk, D., Isik, U., Sonkaya, A., Acikgoz, O., Ozden, E., & Uygun, K. (2017). Netrin-1 in cancer: Potential biomarker and therapeutic target? Tumour Biology, 39(4), 1010428317698388. https://doi.org/10.1177/1010428317698388
Ramesh, G., Berg, A., & Jayakumar, C. (2011). Plasma netrin-1 is a diagnostic biomarker of human cancers. Biomarkers, 16(2), 172–180. https://doi.org/10.3109/1354750x.2010.541564
Wischhusen, J., Wilson, K. E., Delcros, J. G., Pena, R. M., Gibert, B., Jiang, S., Ngo, J., Goldschneider, D., Mehlen, P., Willmann, J. K., & Padilla, F. (2018). Ultrasound molecular imaging as a non-invasive companion diagnostic for netrin-1 interference therapy in breast cancer. Theranostics, 8(18), 5126–5142. https://doi.org/10.7150/thno.27221
Fitamant, J., Guenebeaud, C., Coissieux, M. M., Guix, C., Treilleux, I., Scoazec, J. Y., Bachelot, T., Bernet, A., & Mehlen, P. (2008). Netrin-1 expression confers a selective advantage for tumor cell survival in metastatic breast cancer. Proceedings of the National Academy of Sciences, 105(12), 4850–4855. https://doi.org/10.1073/pnas.0709810105
Grandin, M., Mathot, P., Devailly, G., Bidet, Y., Ghantous, A., Fayrot, C., Gibert, B., Gadot, N., Puisieux, I., Herceg, Z., Delcros, J. G., Bernet, A., Mehlen, P., & Dante, R. (2016). Inhibition of DNA methylation promotes breast tumor sensitivity to netrin-1 interference. EMBO Molecular Medicine, 8(8), 863–877. https://doi.org/10.15252/emmm.201505945
Ebner, K., & Singewald, N. (2006). The role of substance P in stress and anxiety responses. Amino Acids, 31(3), 251–272. https://doi.org/10.1007/s00726-006-0335-9
Palma, C. (2006). Tachykinins and their receptors in human malignancies. Current Drug Targets, 7(8), 1043–1052. https://doi.org/10.2174/138945006778019282
Koon, H. W., & Pothoulakis, C. (2006). Immunomodulatory properties of substance P: The gastrointestinal system as a model. Annals of the New York Academy of Sciences, 1088, 23–40. https://doi.org/10.1196/annals.1366.024
Rao, G., Patel, P. S., Idler, S. P., Maloof, P., Gascon, P., Potian, J. A., & Rameshwar, P. (2004). Facilitating role of preprotachykinin-I gene in the integration of breast cancer cells within the stromal compartment of the bone marrow: A model of early cancer progression. Cancer Research, 64(8), 2874–2881. https://doi.org/10.1158/0008-5472.Can-03-3121
Munoz, M., & Covenas, R. (2010). Neurokinin-1 receptor: A new promising target in the treatment of cancer. Discovery Medicine, 10(53), 305–313.
Garcia-Recio, S., Pastor-Arroyo, E. M., Marin-Aguilera, M., Almendro, V., & Gascon, P. (2015). The transmodulation of HER2 and EGFR by substance P in breast cancer cells requires c-Src and metalloproteinase activation. PLos One, 10(6). https://doi.org/10.1371/journal.pone.0129661
Suzuki, R., Furuno, T., McKay, D. M., Wolvers, D., Teshima, R., Nakanishi, M., & Bienenstock, J. (1999). Direct neurite-mast cell communication in vitro occurs via the neuropeptide substance P. The Journal of Immunology, 163(5), 2410–2415.
Medeiros, P. J., & Jackson, D. N. (2013). Neuropeptide Y Y5-receptor activation on breast cancer cells acts as a paracrine system that stimulates VEGF expression and secretion to promote angiogenesis. Peptides, 48, 106–113. https://doi.org/10.1016/j.peptides.2013.07.029
Dupouy, S., Viardot-Foucault, V., Alifano, M., Souaze, F., Plu-Bureau, G., Chaouat, M., Lavaur, A., Hugol, D., Gespach, C., Gompel, A., & Forgez, P. (2009). The neurotensin receptor-1 pathway contributes to human ductal breast cancer progression. PLoS One, 4(1). https://doi.org/10.1371/journal.pone.0004223
Fox, J. P., Philip, E. J., Gross, C. P., Desai, R. A., Killelea, B., & Desai, M. M. (2013). Associations between mental health and surgical outcomes among women undergoing mastectomy for cancer. The Breast Journal, 19(3), 276–284. https://doi.org/10.1111/tbj.12096
Jiang, L. W., Huang, S. B., Wang, J. Q., Zhang, Y. W., Xiong, Y. Q., Zeng, S. X., & Lu, H. (2020). Inactivating p53 is essential for nerve growth factor receptor to promote melanoma-initiating cell-stemmed tumorigenesis. Cell Death Dis, 11(7). https://doi.org/10.1038/s41419-020-02758-6
Chida, Y., Hamer, M., Wardle, J., & Steptoe, A. (2008). Do stress-related psychosocial factors contribute to cancer incidence and survival? Nature Clinical Practice Oncology, 5(8), 466–475. https://doi.org/10.1038/ncponc1134
Eng, J. W., Kokolus, K. M., Reed, C. B., Hylander, B. L., Ma, W. W., & Repasky, E. A. (2014). A nervous tumor microenvironment: The impact of adrenergic stress on cancer cells, immunosuppression, and immunotherapeutic response. Cancer Immunology, Immunotherapy, 63(11), 1115–1128. https://doi.org/10.1007/s00262-014-1617-9
Shi, M., Liu, D., Yang, Z., & Guo, N. (2013). Central and peripheral nervous systems: Master controllers in cancer metastasis. Cancer and Metastasis Reviews, 32(3–4), 603–621. https://doi.org/10.1007/s10555-013-9440-x
Szpunar, M. J., Belcher, E. K., Dawes, R. P., & Madden, K. S. (2016). Sympathetic innervation, norepinephrine content, and norepinephrine turnover in orthotopic and spontaneous models of breast cancer. Brain Behavior and Immunity, 53, 223–233. https://doi.org/10.1016/j.bbi.2015.12.014
Cole, S. W. (2013). Nervous system regulation of the cancer genome. Brain, Behavior, and Immunity, 30(Suppl), S10-18. https://doi.org/10.1016/j.bbi.2012.11.008
Cui, B., Luo, Y., Tian, P., Peng, F., Lu, J., Yang, Y., Su, Q., Liu, B., Yu, J., Luo, X., Yin, L., Cheng, W., An, F., He, B., Liang, D., Wu, S., Chu, P., Song, L., Liu, X., … Liu, Q. (2019). Stress-induced epinephrine enhances lactate dehydrogenase A and promotes breast cancer stem-like cells. The Journal of Clinical Investigation, 129(3), 1030–1046. https://doi.org/10.1172/JCI121685
Yang, H., Xia, L., Chen, J., Zhang, S., Martin, V., Li, Q., Lin, S., Chen, J., Calmette, J., Lu, M., Fu, L., Yang, J., Pan, Z., Yu, K., He, J., Morand, E., Schlecht-Louf, G., Krzysiek, R., Zitvogel, L., … Ma, Y. (2019). Stress-glucocorticoid-TSC22D3 axis compromises therapy-induced antitumor immunity. Nature Medicine, 25(9), 1428–1441. https://doi.org/10.1038/s41591-019-0566-4
Zhang, Y., Shi, G., Zhang, H., Xiong, Q., Cheng, F., Wang, H., Luo, J., Zhang, Y., Shi, P., Xu, J., Fu, J., Chen, N., Cheng, L., Li, Y., Dai, L., Yang, Y., Yu, D., Zhang, S., & Deng, H. (2021). Dexamethasone enhances the lung metastasis of breast cancer via a PI3K-SGK1-CTGF pathway. Oncogene, 40(35), 5367–5378. https://doi.org/10.1038/s41388-021-01944-w
Li, Z., Dong, J., Zou, T., Du, C., Li, S., Chen, C., Liu, R., & Wang, K. (2017). Dexamethasone induces docetaxel and cisplatin resistance partially through up-regulating Kruppel-like factor 5 in triple-negative breast cancer. Oncotarget, 8(7), 11555–11565. https://doi.org/10.18632/oncotarget.14135
He, L., Yuan, L., Sun, Y., Wang, P., Zhang, H., Feng, X., Wang, Z., Zhang, W., Yang, C., Zeng, Y. A., Zhao, Y., Chen, C., & Zhang, L. (2019). Glucocorticoid receptor signaling activates TEAD4 to promote breast cancer progression. Cancer Research, 79(17), 4399–4411. https://doi.org/10.1158/0008-5472.CAN-19-0012
Mohammadpour, H., MacDonald, C. R., Qiao, G., Chen, M., Dong, B., Hylander, B. L., McCarthy, P. L., Abrams, S. I., & Repasky, E. A. (2019). β2 Adrenergic receptor-mediated signaling regulates the immunosuppressive potential of myeloid-derived suppressor cells. The Journal of Clinical Investigation, 129(12), 5537–5552. https://doi.org/10.1172/JCI129502
Mravec, B., Tibensky, M., & Horvathova, L. (2020). Stress and cancer. Part II: Therapeutic implications for oncology. Journal of Neuroimmunology, 346, 577312. https://doi.org/10.1016/j.jneuroim.2020.577312
Armaiz-Pena, G. N., Lutgendorf, S. K., Cole, S. W., & Sood, A. K. (2009). Neuroendocrine modulation of cancer progression. Brain, Behavior, and Immunity, 23(1), 10–15. https://doi.org/10.1016/j.bbi.2008.06.007
Bower, J. E., Crosswell, A. D., Stanton, A. L., Crespi, C. M., Winston, D., Arevalo, J., Ma, J., Cole, S. W., & Ganz, P. A. (2015). Mindfulness meditation for younger breast cancer survivors: A randomized controlled trial. Cancer, 121(8), 1231–1240. https://doi.org/10.1002/cncr.29194
Cramer, H., Lauche, R., Klose, P., Lange, S., Langhorst, J., & Dobos, G. J. (2017). Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Systematic Review, 1, CD010802. https://doi.org/10.1002/14651858.CD010802.pub2
Zhang, Y., Sun, Y., Li, D., Liu, X., Fang, C., Yang, C., Luo, T., Lu, H., Li, H., Zhang, H., Liang, Q., Wu, J., Huang, L., Xu, R., Ren, L., & Chen, Q. (2021). Acupuncture for breast cancer: A systematic review and meta-analysis of patient-reported outcomes. Frontiers in Oncology, 11, 646315. https://doi.org/10.3389/fonc.2021.646315
Dieli-Conwright, C. M., Courneya, K. S., Demark-Wahnefried, W., Sami, N., Lee, K., Sweeney, F. C., Stewart, C., Buchanan, T. A., Spicer, D., Tripathy, D., Bernstein, L., & Mortimer, J. E. (2018). Aerobic and resistance exercise improves physical fitness, bone health, and quality of life in overweight and obese breast cancer survivors: A randomized controlled trial. Breast Cancer Research, 20(1), 124. https://doi.org/10.1186/s13058-018-1051-6
Bozorgi, A., Khazaei, S., Khademi, A., & Khazaei, M. (2020). Natural and herbal compounds targeting breast cancer, a review based on cancer stem cells. Iranian Journal of Basic Medical Sciences, 23(8), 970–983. https://doi.org/10.22038/ijbms.2020.43745.10270
Gosain, R., Gage-Bouchard, E., Ambrosone, C., Repasky, E., & Gandhi, S. (2020). Stress reduction strategies in breast cancer: Review of pharmacologic and non-pharmacologic based strategies. Semin Immunopathol, 42(6), 719–734. https://doi.org/10.1007/s00281-020-00815-y
Rosendahl, A. H., Perks, C. M., Zeng, L., Markkula, A., Simonsson, M., Rose, C., Ingvar, C., Holly, J. M., & Jernstrom, H. (2015). Caffeine and caffeic acid inhibit growth and modify estrogen receptor and insulin-like growth factor I receptor levels in human breast cancer. Clinical Cancer Research, 21(8), 1877–1887. https://doi.org/10.1158/1078-0432.CCR-14-1748
Zheng, K. H., Zhu, K., Wactawski-Wende, J., Freudenheim, J. L., LaMonte, M. J., Hovey, K. M., & Mu, L. (2021). Caffeine intake from coffee and tea and invasive breast cancer incidence among postmenopausal women in the Women’s Health Initiative. International Journal of Cancer, 149(12), 2032–2044. https://doi.org/10.1002/ijc.33771
Liu, L., Shi, Y., Li, T., Qin, Q., Yin, J., Pang, S., Nie, S., & Wei, S. (2016). Leisure time physical activity and cancer risk: Evaluation of the WHO’s recommendation based on 126 high-quality epidemiological studies. British Journal of Sports Medicine, 50(6), 372–378. https://doi.org/10.1136/bjsports-2015-094728
Lynch, B. M., Neilson, H. K., & Friedenreich, C. M. (2011). Physical activity and breast cancer prevention. Recent Results in Cancer Research, 186, 13–42. https://doi.org/10.1007/978-3-642-04231-7_2
Schmid, D., & Leitzmann, M. F. (2014). Association between physical activity and mortality among breast cancer and colorectal cancer survivors: A systematic review and meta-analysis. Annals of Oncology, 25(7), 1293–1311. https://doi.org/10.1093/annonc/mdu012
Agostini, D., Natalucci, V., Baldelli, G., De Santi, M., Donati Zeppa, S., Vallorani, L., Annibalini, G., Lucertini, F., Federici, A., Izzo, R., Stocchi, V., & Barbieri, E. (2018). New insights into the role of exercise in inhibiting mTOR signaling in triple-negative breast cancer. Oxidative Medicine and Cellular Longevity, 2018, 5896786. https://doi.org/10.1155/2018/5896786
Dieli-Conwright, C. M., Lee, K., & Kiwata, J. L. (2016). Reducing the risk of breast cancer recurrence: An evaluation of the effects and mechanisms of diet and exercise. Curr Breast Cancer Rep, 8(3), 139–150. https://doi.org/10.1007/s12609-016-0218-3
Xu, Y., & Rogers, C. J. (2020). Physical activity and breast cancer prevention: Possible role of immune mediators. Frontiers in Nutrition, 7, 557997. https://doi.org/10.3389/fnut.2020.557997
Kim, J. S., Wilson, R. L., Taaffe, D. R., Galvao, D. A., Gray, E., & Newton, R. U. (2022). Myokine expression and tumor-suppressive effect of serum after 12 wk of exercise in prostate cancer patients on ADT. Medicine and Science in Sports and Exercise, 54(2), 197–205. https://doi.org/10.1249/MSS.0000000000002783
Gannon, N. P., Vaughan, R. A., Garcia-Smith, R., Bisoffi, M., & Trujillo, K. A. (2015). Effects of the exercise-inducible myokine irisin on malignant and non-malignant breast epithelial cell behavior in vitro. International Journal of Cancer, 136(4), E197-202. https://doi.org/10.1002/ijc.29142
Raimondi, S., Botteri, E., Munzone, E., Cipolla, C., Rotmensz, N., DeCensi, A., & Gandini, S. (2016). Use of beta-blockers, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers and breast cancer survival: Systematic review and meta-analysis. International Journal of Cancer, 139(1), 212–219. https://doi.org/10.1002/ijc.30062
Childers, W. K., Hollenbeak, C. S., & Cheriyath, P. (2015). β-Blockers reduce breast cancer recurrence and breast cancer death: A meta-analysis. Clinical Breast Cancer, 15(6), 426–431. https://doi.org/10.1016/j.clbc.2015.07.001
Zhao, Y., Wang, Q. Y., Zhao, X., Meng, H. T., & Yu, J. (2018). Effect of antihypertensive drugs on breast cancer risk in female hypertensive patients: Evidence from observational studies. Clinical and Experimental Hypertension, 40(1), 22–27. https://doi.org/10.1080/10641963.2017.1288736
Barron, T. I., Connolly, R. M., Sharp, L., Bennett, K., & Visvanathan, K. (2011). Beta blockers and breast cancer mortality: A population-based study. Journal of Clinical Oncology, 29(19), 2635–2644. https://doi.org/10.1200/Jco.2010.33.5422
Mulcrone, P. L., Campbell, J. P., Clement-Demange, L., Anbinder, A. L., Merkel, A. R., Brekken, R. A., Sterling, J. A., & Elefteriou, F. (2017). Skeletal colonization by breast cancer cells is stimulated by an osteoblast and β2AR-dependent neo-angiogenic switch. Journal of Bone and Mineral Research, 32(7), 1442–1454. https://doi.org/10.1002/jbmr.3133
Melhem-Bertrandt, A., Chavez-MacGregor, M., Lei, X. D., Brown, E. N., Lee, R. T., Meric-Bernstam, F., Sood, A. K., Conzen, S. D., Hortobagyi, G. N., & Gonzalez-Angulo, A. M. (2011). Beta-blocker use is associated with improved relapse-free survival in patients with triple-negative breast cancer. Journal of Clinical Oncology, 29(19), 2645–2652. https://doi.org/10.1200/Jco.2010.33.4441
Hiller, J. G., Cole, S. W., Crone, E. M., Byrne, D. J., Shackleford, D. M., Pang, J. B., Henderson, M. A., Nightingale, S. S., Ho, K. M., Myles, P. S., Fox, S., Riedel, B., & Sloan, E. K. (2020). Preoperative β-blockade with propranolol reduces biomarkers of metastasis in breast cancer: A phase II randomized trial. Clinical Cancer Research, 26(8), 1803–1811. https://doi.org/10.1158/1078-0432.CCR-19-2641
Montoya, A., Amaya, C. N., Belmont, A., Diab, N., Trevino, R., Villanueva, G., Rains, S., Sanchez, L. A., Badri, N., Otoukesh, S., Khammanivong, A., Liss, D., Baca, S. T., Aguilera, R. J., Dickerson, E. B., Torabi, A., Dwivedi, A. K., Abbas, A., Chambers, K., … Nahleh, Z. (2017). Use of non-selective β-blockers is associated with decreased tumor proliferative indices in early stage breast cancer. Oncotarget, 8(4), 6446–6460. https://doi.org/10.18632/oncotarget.14119
Benish, M., Bartal, I., Goldfarb, Y., Levi, B., Avraham, R., Raz, A., & Ben-Eliyahu, S. (2008). Perioperative use of beta-blockers and COX-2 inhibitors may improve immune competence and reduce the risk of tumor metastasis. Annals of Surgical Oncology, 15(7), 2042–2052. https://doi.org/10.1245/s10434-008-9890-5
Li, R., Liu, H., Dilger, J. P., & Lin, J. (2018). Effect of propofol on breast cancer cell, the immune system, and patient outcome. BMC Anesthesiology, 18(1), 77. https://doi.org/10.1186/s12871-018-0543-3
Garib, V., Niggemann, B., Zanker, K. S., Brandt, L., & Kubens, B. S. (2002). Influence of non-volatile anesthetics on the migration behavior of the human breast cancer cell line MDA-MB-468. Acta Anaesthesiologica Scandinavica, 46(7), 836–844. https://doi.org/10.1034/j.1399-6576.2002.460714.x
Garib, V., Lang, K., Niggemann, B., Zanker, K. S., Brandt, L., & Dittmar, T. (2005). Propofol-induced calcium signalling and actin reorganization within breast carcinoma cells. European Journal of Anaesthesiology, 22(8), 609–615. https://doi.org/10.1017/s026502150500102x
Zhang, D., Li, X., Yao, Z., Wei, C., Ning, N., & Li, J. (2014). GABAergic signaling facilitates breast cancer metastasis by promoting ERK1/2-dependent phosphorylation. Cancer Letters, 348(1–2), 100–108. https://doi.org/10.1016/j.canlet.2014.03.006
Meng, C., Song, L., Wang, J., Li, D., Liu, Y., & Cui, X. (2017). Propofol induces proliferation partially via downregulation of p53 protein and promotes migration via activation of the Nrf2 pathway in human breast cancer cell line MDA-MB-231. Oncology Reports, 37(2), 841–848. https://doi.org/10.3892/or.2016.5332
Li, Q., Zhang, L., Han, Y., Jiang, Z., & Wang, Q. (2012). Propofol reduces MMPs expression by inhibiting NF-kappaB activity in human MDA-MB-231 cells. Biomedicine & Pharmacotherapy, 66(1), 52–56. https://doi.org/10.1016/j.biopha.2011.10.006
Ecimovic, P., Murray, D., Doran, P., & Buggy, D. J. (2014). Propofol and bupivacaine in breast cancer cell function in vitro - Role of the NET1 gene. Anticancer Research, 34(3), 1321–1331.
Yu, B., Gao, W., Zhou, H., Miao, X., Chang, Y., Wang, L., Xu, M., & Ni, G. (2018). Propofol induces apoptosis of breast cancer cells by downregulation of miR-24 signal pathway. Cancer Biomarkers, 21(3), 513–519. https://doi.org/10.3233/CBM-170234
Jaura, A. I., Flood, G., Gallagher, H. C., & Buggy, D. J. (2014). Differential effects of serum from patients administered distinct anaesthetic techniques on apoptosis in breast cancer cells in vitro: A pilot study. British Journal of Anaesthesia, 113(Suppl 1), i63-67. https://doi.org/10.1093/bja/aet581
Alter, G., Malenfant, J. M., & Altfeld, M. (2004). CD107a as a functional marker for the identification of natural killer cell activity. Journal of Immunological Methods, 294(1–2), 15–22. https://doi.org/10.1016/j.jim.2004.08.008
Kimmick, G. G., Lovato, J., McQuellon, R., Robinson, E., & Muss, H. B. (2006). Randomized, double-blind, placebo-controlled, crossover study of sertraline (Zoloft) for the treatment of hot flashes in women with early stage breast cancer taking tamoxifen. The Breast Journal, 12(2), 114–122. https://doi.org/10.1111/j.1075-122X.2006.00218.x
Wang, C., Li, K., Seo, D. C., & Gaylord, S. (2020). Use of complementary and alternative medicine in children with ADHD: Results from the 2012 and 2017 National Health Interview Survey. Complementary Therapies in Medicine, 49, 102352. https://doi.org/10.1016/j.ctim.2020.102352
Molassiotis, A., Scott, J. A., Kearney, N., Pud, D., Magri, M., Selvekerova, S., Bruyns, I., Fernadez-Ortega, P., Panteli, V., Margulies, A., Gudmundsdottir, G., Milovics, L., Ozden, G., Platin, N., & Patiraki, E. (2006). Complementary and alternative medicine use in breast cancer patients in Europe. Supportive Care in Cancer, 14(3), 260–267. https://doi.org/10.1007/s00520-005-0883-7
Greenlee, H., Kwan, M. L., Ergas, I. J., Sherman, K. J., Krathwohl, S. E., Bonnell, C., Lee, M. M., & Kushi, L. H. (2009). Complementary and alternative therapy use before and after breast cancer diagnosis: The pathways study. Breast Cancer Research and Treatment, 117(3), 653–665. https://doi.org/10.1007/s10549-009-0315-3
Wanchai, A., Arrner, J. M., & Stewart, B. R. (2010). Complementary and alternative medicine use among women with breast cancer: A systematic review. Clinical Journal of Oncology Nursing, 14(4), 431–431. https://doi.org/10.1188/10.Cjon.E45-E55
Pedersen, C. G., Christensen, S., Jensen, A. B., & Zachariae, R. (2013). In God and CAM we trust. Religious faith and use of complementary and alternative medicine (CAM) in a nationwide cohort of women treated for early breast cancer. Journal of Religion and Health, 52(3), 991–1013. https://doi.org/10.1007/s10943-012-9569-x
Sasaki, Y., Cheon, C., Motoo, Y., Jang, S., Park, S., Ko, S. G., Jang, B. H., & Hwang, D. S. (2019). Complementary and alternative medicine for breast cancer patients: An overview of systematic reviews. Yakugaku Zasshi, 139(7), 1027–1046. https://doi.org/10.1248/yakushi.18-00215
Funding
This work was supported by the National Key R&D Program of China (2020YFA0112300), the National Natural Science Foundation of China (81830087, U2102203, 82102987), the Yunnan Fundamental Research Projects (202101AS070050), the Guangdong Foundation Committee for Basic and Applied Basic Research projects (2022A1515012420), the Yunnan (Kunming) Academician Expert Workstation (YSZJGZZ-2020025), the Guangdong Medical University Affiliated Hospital Competitive Clinical Study (LCYJ2021B003), the Guangdong Province Characteristic Innovation Projects (2021KTSCX037), and the Guangdong Foundation Committe for Basic and Applied Basic Research Projects (2022A1515012420).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cui, Q., Jiang, D., Zhang, Y. et al. The tumor-nerve circuit in breast cancer. Cancer Metastasis Rev 42, 543–574 (2023). https://doi.org/10.1007/s10555-023-10095-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-023-10095-1