Abstract
Aim
This study aims to explore the independent age, period, and cohort effects on the burden of gout globally and across different Socio-demographic Index (SDI) regions.
Subject and methods
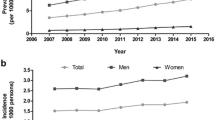
We extracted data of age-standardized incidence, prevalence, and disability-adjusted life years (DALYs) rate from the Global Burden of Disease (GBD) database as gout burden measures. In the study, Joinpoint regression analysis was conducted to explore the temporal trends from 1990 to 2019. Trend analyses were explored according to 21 world regions (including high-income North America, Australasia, Southern Latin America, East Asia, etc.) and sociodemographic indices (SDI). The age-period-cohort (APC) model was performed to estimate the age, period, and cohort effects on gout.
Results
Globally, the age-standardized incidence rate (ASIR), age-standardized prevalence rate (ASPR), and DALYs increased from 1990 to 2019. The ASIR, ASPR, and DALYs for the age effect of gout in different SDI regions increased at first, and then decreased, peaking at 70–74 years. The period effect showed an upward trend, while the cohort effect continued to decrease. Surprisingly, the age, period, and cohort effect for global gout DALYs differed significantly from that in five SDI regions.
Conclusions
Therefore, more specific interventions are urgently warranted to reduce the incidence and prevalence of gout, especially among older adults in high SDI regions.



Similar content being viewed by others
Availability of data and material
The dataset in the study was publicly available from https://vizhub.healthdata.org/gbd-results/.
Code availability
Not applicable.
References
Ayoub-Charette S, Liu Q, Khan TA, Au-Yeung F, Blanco Mejia S, de Souza RJ, Wolever TM, Leiter LA, Kendall C, Sievenpiper JL (2019) Important food sources of fructose-containing sugars and incident gout: a systematic review and meta-analysis of prospective cohort studies. BMJ Open 9:e024171
Campion EW, Glynn RJ, DeLabry LO (1987) Asymptomatic hyperuricemia. Risks and consequences in the Normative Aging Study. Am J Med 82:421–426
Chen Y, Tang Z, Huang Z, Zhou W, Li Z, Li X, Sun F (2017) The prevalence of gout in mainland China from 2000 to 2016: a systematic review and meta-analysis. J Public Health 25:521–529
Chen-Xu M, Yokose C, Rai SK, Pillinger MH, Choi HK (2019) Contemporary prevalence of gout and hyperuricemia in the United States and decadal trends: the National Health and Nutrition Examination Survey, 2007-2016. Arthritis Rheumatol 71:991–999
Choi HK, Curhan G (2008) Soft drinks, fructose consumption, and the risk of gout in men: prospective cohort study. BMJ 336:309–312
Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G (2004a) Alcohol intake and risk of incident gout in men: a prospective study. Lancet 363:1277–1281
Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G (2004b) Purine-rich foods, dairy and protein intake, and the risk of gout in men. N Engl J Med 350:1093–1103
Collaborators GBDD (2019) Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 393:1958–1972
Collaborators GDaH (2019) Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 393:e44
Dalbeth N, Merriman TR, Stamp LK (2016) Gout Lancet 388:2039–2052
Dalbeth N, Gosling AL, Gaffo A, Abhishek A (2021) Gout Lancet 397:1843–1855
Dehlin M, Drivelegka P, Sigurdardottir V, Svard A, Jacobsson LT (2016) Incidence and prevalence of gout in Western Sweden. Arthritis Res Ther 18:164
Dehlin M, Jacobsson L, Roddy E (2020) Global epidemiology of gout: prevalence, incidence, treatment patterns and risk factors. Nat Rev Rheumatol 16:380–390
Diseases GBD, Injuries C (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1204–1222
Evans PL, Prior JA, Belcher J, Mallen CD, Hay CA, Roddy E (2018) Obesity, hypertension and diuretic use as risk factors for incident gout: a systematic review and meta-analysis of cohort studies. Arthritis Res Ther 20:136
Fu W (2018) A practical guide to age-period-cohort analysis: The identification problem and beyond (Chapman and Hall/CRC)
Guillen AG, Te Karu L, Singh JA, Dalbeth N (2020) Gender and Ethnic Inequities in Gout Burden and Management. Rheum Dis Clin North Am 46:693–703
Hainer BL, Matheson E, Wilkes RT (2014) Diagnosis, treatment, and prevention of gout. Am Fam Physician 90:831–836
Hak AE, Curhan GC, Grodstein F, Choi HK (2010) Menopause, postmenopausal hormone use and risk of incident gout. Ann Rheum Dis 69:1305–1309
Kim JW, Kwak SG, Lee H, Kim SK, Choe JY, Park SH (2017) Prevalence and incidence of gout in Korea: data from the national health claims database 2007-2015. Rheumatol Int 37:1499–1506
Kuo CF, Grainge MJ, Mallen C, Zhang W, Doherty M (2015) Rising burden of gout in the UK but continuing suboptimal management: a nationwide population study. Ann Rheum Dis 74:661–667
McCormick N, Lu N, Yokose C, Joshi AD, Sheehy S, Rosenberg L, Warner ET, Dalbeth N, Merriman TR, Saag KG, Zhang Y, Choi HK (2022a) Racial and Sex Disparities in Gout Prevalence Among US Adults. JAMA Netw Open 5:e2226804
McCormick N, Yokose C, Lu N, Joshi AD, Curhan GC, Choi HK (2022b) Impact of adiposity on risk of female gout among those genetically predisposed: sex-specific prospective cohort study findings over >32 years. Ann Rheum Dis 81:556–563
National Cancer Institute (2022) Joinpoint Regression Program version 4.9.1.0
Pisaniello HL, Lester S, Gonzalez-Chica D, Stocks N, Longo M, Sharplin GR, Dal Grande E, Gill TK, Whittle SL, Hill CL (2018) Gout prevalence and predictors of urate-lowering therapy use: results from a population-based study. Arthritis Res Ther 20:143
Rai SK, Burns LC, De Vera MA, Haji A, Giustini D, Choi HK (2015) The economic burden of gout: A systematic review. Semin Arthritis Rheum 45:75–80
Rai SK, Fung TT, Lu N, Keller SF, Curhan GC, Choi HK (2017) The Dietary Approaches to Stop Hypertension (DASH) diet, Western diet, and risk of gout in men: prospective cohort study. BMJ 357:j1794
Safiri S, Kolahi AA, Cross M, Carson-Chahhoud K, Hoy D, Almasi-Hashiani A, Sepidarkish M, Ashrafi-Asgarabad A, Moradi-Lakeh M, Mansournia MA, Kaufman JS, Collins G, Woolf AD, March L, Smith E (2020) Prevalence, incidence, and years lived with disability due to gout and its attributable risk factors for 195 countries and territories 1990-2017: a systematic analysis of the Global Burden of Disease Study 2017. Arthritis Rheumatol 72:1916–1927
Sigurdardottir V, Drivelegka P, Svard A, Jacobsson LTH, Dehlin M (2018) Work disability in gout: a population-based case-control study. Ann Rheum Dis 77:399–404
Stamp LK, Jordan S (2011) The challenges of gout management in the elderly. Drugs Aging 28:591–603
Taylor WJ, Fransen J, Jansen TL, Dalbeth N, Schumacher HR, Brown M, Louthrenoo W, Vazquez-Mellado J, Eliseev M, McCarthy G, Stamp LK, Perez-Ruiz F, Sivera F, Ea HK, Gerritsen M, Scire C, Cavagna L, Lin C, Chou YY et al (2015) Study for updated gout classification criteria: identification of features to classify gout. Arthritis Care Res (Hoboken) 67:1304–1315
Teng GG, Pan A, Yuan JM, Koh WP (2015) Food Sources of Protein and Risk of Incident Gout in the Singapore Chinese Health Study. Arthritis Rheumatol 67:1933–1942
Wang Y, Weng P, Wan H, Zhang W, Chen C, Chen Y, Cai Y, Guo M, Xia F, Wang N, Lu Y (2020) Economic status moderates the association between early-life famine exposure and hyperuricemia in adulthood. J Clin Endocrinol Metab 105:e3862
Xia Y, Wu Q, Wang H, Zhang S, Jiang Y, Gong T, Xu X, Chang Q, Niu K, Zhao Y (2020) Global, regional and national burden of gout, 1990-2017: a systematic analysis of the Global Burden of Disease Study. Rheumatology (Oxford) 59:1529–1538
Yang Y, Fu WJ, Land KC (2004) A methodological comparison of age-period-cohort models: the intrinsic estimator and conventional generalized linear models. Sociol Methodol 34:75–110
Yokose C, McCormick N, Lu N, Tanikella S, Lin K, Joshi AD, Raffield LM, Warner E, Merriman T, Hsu J, Saag K, Zhang Y, Choi HK (2023) Trends in prevalence of gout among US Asian adults, 2011-2018. JAMA Netw Open 6:e239501
Zhang M, Zhu X, Wu J, Huang Z, Zhao Z, Zhang X, Xue Y, Wan W, Li C, Zhang W, Wang L, Zhou M, Zou H, Wang L (2021) Prevalence of hyperuricemia among Chinese adults: findings from two nationally representative cross-sectional surveys in 2015-16 and 2018-19. Front Immunol 12:791983
Zhu B, Wang Y, Zhou W, Jin S, Shen Z, Zhang H, Zhang X, Ding X, Li Y (2022) Trend dynamics of gout prevalence among the Chinese population, 1990-2019: a joinpoint and age-period-cohort analysis. Front Public Health 10:1008598
Zobbe K, Prieto-Alhambra D, Cordtz R, Hojgaard P, Hindrup JS, Kristensen LE, Dreyer L (2019) Secular trends in the incidence and prevalence of gout in Denmark from 1995 to 2015: a nationwide register-based study. Rheumatology (Oxford) 58:836–839
Acknowledgments
We appreciate the Institute for Health Metrics and Evaluation and the Global Burden of Disease study collaborators for the data. We also would like to thank Xiao Ming (Xiaoming_room@hotmail.com) for his guidance in GBD database analysis.
Funding
The study was supported by the National Natural Science Foundations (NSFC) of China [grant number 81973153].
Author information
Authors and Affiliations
Contributions
Wenyan Yang conceived and designed the study, collected and analyzed the data, and drafted the article. Yiran Cui helped analyze the data and revised the article. Gang Tian, Feixiang Zhou, Jingliang Shuai, and Yulan Ma revised the article. Yan Yan applied for the funding and supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
The authors agree to publish in the journal.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 317 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, W., Cui, Y., Tian, G. et al. Secular trends in the global burden of gout: an age-period-cohort and joinpoint analysis. J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-02071-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-02071-4