Abstract
This scoping review aimed to synthesize and explore the current boundaries and limitations of laboratory research on the effectiveness of continuous chelation irrigation protocol in endodontics. This scoping review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews. Literature search was conducted on Pubmed and Scopus to identify all laboratory studies evaluating smear layer and hard-tissue debris removal or, antimicrobial efficacy, or dentine erosion induced by continuous chelation. Two independent reviewers performed the all review steps and the relevant items were recorded. Seventy-seven potentially relevant studies were identified. Finally, 23 laboratory studies met the eligibility criteria for qualitative synthesis. Seven studies focused on the smear layer/debris removal outcome, 10 on antimicrobial activity, and 10 on dentine erosion. In general, the continuous chelation protocol was equally or more effective in the cleanliness of root canals and antimicrobial activity compared with traditional sequential protocol. In addition, etidronate solutions seemed to be milder chelating agents compared to those with EDTA, thus resulting in reduced or no dentine erosion and roughness modification. Yet, the methodological differences among the included studies limit the results’ generalizability. The continuous chelation seems to be equally or more effective in all investigated outcomes when compared with the traditional sequential protocol. The methodological variability among the studies and shortcomings in the methods employed limit the generalizability and clinical relevance of the results. Standardized laboratory conditions combined with reliable three-dimensional investigation approaches are necessary to obtain clinically informative findings.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
The root canal treatment aims to eliminate the intracanal infection and avoid reinfection by obturation of the root canal space [1, 2]. Mechanical preparation is able to remove microorganisms from an infected root canal [3]. However, after instrumentation up to 35% of the canal surface area may remain unchanged [4], which may not guarantee a clean and bacteria-free root canal space. As a consequence, an active irrigation sequence is generally combined with the mechanical treatment [5]. Although the irrigants are crucial for the success of root canal treatment, it is important they do not damage the tissues surrounding the root, they are safe for both patient and clinician, and ensure full functional recovery of the tooth [6]. Sodium hypochlorite (NaOCl), a non-specific proteolytic agent available in different concentrations (0.5–6%), is used for its notable tissue solvent action, antimicrobial and anti-biofilm effects [7, 8]. However, NaOCl is unable to eliminate the smear layer and prevent the accumulation of hard-tissue debris [9]. Dentinal debris can act as a physical barrier that prevents NaOCl from reaching all anatomical anfractuosities [10, 11]. In addition, the presence of dentinal debris reduces the antimicrobial efficacy of NaOCl on dentinal structure [11]. Consequently, considering its inability to remove the inorganic tissue remnants, NaOCl is usually followed by a chelating agent such as ethylenediaminetetraacetic acid (EDTA), at a concentration of 15–17% for 1 − 2 min [12, 13].
Of note, chelating agents negatively impact the free available chlorine content of NaOCl and thus reduce its tissue dissolution ability, while the antimicrobial action decreases only when the initial NaOCl concentrations are low [14]. In order to prevent these phenomena, the sequential use of NaOCl/EDTA, known as the “sequential protocol”, is routinely used in day-to-day clinical practice. NaOCl is used as an antimicrobial agent during instrumentation, and EDTA is applied at the end of instrumentation to promote the smear layer removal [15]. A final flush of NaOCl has also been proposed to improve NaOCl penetration into the areas that were earlier covered with the smear layer [16].
The sequential protocol results in a wider opening of the dentinal tubules [17] and intertubular tunnelling due to dentine erosion [18]. NaOCl/EDTA determines the complete decalcification of the superficial 1 − 5 µm of intertubular dentine, and up to 20 µm of the dentinal tubular walls [17]. These structural changes significantly diminish the flexural strength of dentine [19,20,21] and may increase the risk of vertical root fractures [22].
To overcome the above issues caused by the sequential use of NaOCl/EDTA, the concept of “continuous chelation” was proposed in 2005. It refers to the combination of a soft chelator with NaOCl for simultaneous antimicrobial and proteolytic action with the smear layer removal [23,24,25]. According to this protocol, NaOCl is added with the salt of a weak chelator, 1 hydroxyethylidene-1, 1-bisphosphonate or etidronate (HEBP or HEDP or etidronate), because the tetra-sodium HEDP salt is extremely compatible with NaOCl [25]. Continuous chelation is an attractive concept because of its multiple benefits: simplification of the clinical procedure, improved debris removal [13], acceptable tolerability with some dental materials [26], and no reduction in NaOCl antimicrobial activity [25] and dissolving properties [23]. Moreover, chelators promote the detachment of biofilms from the root canal walls [27, 28] and eliminate the metal ions employed by bacteria as nutrients [29]. One of the major concerns associated with their application is the potential chemical reactions between NaOCl and the chelator. Indeed, NaOCl is able to chemically interact with other irrigants and the consequent mixing of two irrigants (i.e., chelators and antimicrobials) has different effects. It determines the pH reduction of the hypochlorite component and its decomposition to chlorine gas. In addition, the mixing generates intermediate toxic products able to reduce the clinical performance of NaOCl [30].
To date, the majority of available studies are performed in laboratory setting under different methodological conditions. To explore and define the current knowledge on the effectiveness of continuous chelation in endodontic research, a scoping review of current laboratory studies is appropriate. A scoping review is a flexible approach for exploring a broad question with the aim of synthesizing the existing knowledge boundaries, identifying the current gaps and addressing the future research [31]. The aim of this scoping review was to explore the current literature in relation to the effectiveness of continuous chelation compared to the sequential protocol in order to provide an overall and updated view for researchers to detect gaps and carry out further laboratory studies.
Materials and methods
This scoping review was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews [32].
Research question
This scoping review aimed to synthesize and explore the current boundaries and limitations of laboratory research on the effectiveness of continuous chelation irrigation protocol in smear layer and hard-tissue debris removal, antimicrobial efficacy and dentine erosion.
Search strategy
A literature search was conducted in the PubMed and Scopus databases on 25 September, 2022 to identify all pertinent studies. The following search string was adopted for each database: (“continuous chelation” OR “soft chelation” OR “etidronate” OR “HEDP” OR “HEBP” OR “etidronic acid”) AND (“root canal irrigants” OR “irrigation” OR “antimicrobial efficacy” OR “smear layer” OR “debris” OR “dentine erosion”) AND (“endodontics”). No language restrictions were applied. Reference lists of included studies were further screened for other potential studies. Principal peer-reviewed scientific journals in endodontics (Journal of Endodontics, International Endodontic Journal, Clinical Oral Investigations, Odontology and Australian Endodontic Journal) were also hand searched. Two review authors independently reviewed and selected studies from searches. Disagreements were resolved through discussion or by the intervention of a third reviewer.
Eligibility criteria
Laboratory studies evaluating smear layer and hard-tissue debris removal or antimicrobial efficacy or dentine erosion induced by continuous chelation compared to sequential chelation were included. The exclusion criteria included the study design (animal and human studies), outcome, comparator (i.e. no comparison with NaOCl and EDTA solutions), article type (editorials, commentaries, letters and reviews), peer-revision (abstracts and preprint articles) and language (studies without an English abstract).
Data extraction
For each study, the following items:
-
Name of first author
-
Year of the study published
-
Study design
-
Sample size (n)
-
Irrigants used
-
Outcome(s)
-
Measurement outcome(s)
-
Main findings
were extracted and synthesized in study tables for each outcome investigated. Data were extracted independently by two reviewers. Any discrepancies were solved by discussion or help of a third reviewer.
Results
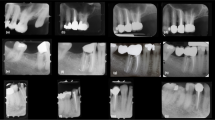
Study selection is schematized in Fig. 1, according to PRISMA 2020 for scoping reviews. The search retrieved 77 potentially relevant studies. Duplicates (n = 9) and articles not satisfying the inclusion criteria (n = 45) were removed. Finally, 23 studies met the eligibility criteria for qualitative synthesis. The main features of the included studies are reported in Tables 1, 2, 3.
Smear layer/debris removal
The studies retrieved for smear layer/debris removal outcomes are shown in Table 1. Five blinded, randomized studies on extracted human teeth [3, 13, 33,34,35] were identified. Two studies were randomized but no blinding was reported [17, 36]. Four studies tested HEBP (9–18%) combined with different NaOCl concentrations (2–3%) [13, 17, 34, 36], one study in an aqueous gel consisting in 2% alginate, 3% aerosil, 10% Tween 80 [3] and one with EDTA to obtain Na2 and Na4 salts of HEDP [33]. One study tested the efficacy of two techniques for activation of irrigants (i.e., XP-Endo Finisher and passive ultrasonics irrigation) [36]. Different testing methods were employed to determine the smear layer/debris removal including a precision balance [36], scanning electron microscopy (SEM) [3, 17, 34, 35], laser microscopy [33] and micro-CT [13].
Overall, the continuous chelation protocol was equally or more effective in the cleanliness of root canals (smear layer/debris removal) when compared with the traditional sequential protocol [3, 13, 17, 34, 36]. Patil et al. [35] reported that sequential use of 5.25% NaOCl + 17% EDTA (both combined with surfactants) was more efficient than 18% etidronic acid + 5% NaOCl in the removal of smear layer in the apical third. According to Deari et al. [33], EDTA was a stronger chelator than HEDP. Nevertheless, none of the chelating solutions was able to completely remove smear layer and debris from the root canal walls.
Antimicrobial activity
Table 2 reports the details of the ten studies identified for the antimicrobial activity outcome. Two blinded, randomized studies on extracted human teeth [25, 37], seven randomized with no reporting on blinding procedures [27, 38,39,40,41,42,43] and one with no information on randomization and blinding [44] were retrieved. All studies tested HEBP (5–18%) combined with different NaOCl concentrations (1–6%). Three studies tested the efficacy of techniques for activation of irrigants (i.e., XP-Endo Finisher, diode laser, Er: YAG laser activation, passive ultrasonics irrigation) [40, 42, 43]. Antimicrobial activity was principally assessed by confocal laser scanning microscopy [27, 37,38,39, 41,42,43]. Other testing methods include optical coherence tomography [44], quantitative real-time polymerase chain reaction [40], SEM and atomic absorption spectrometry [25].
In general, the continuous chelation protocol was equally or more effective in antimicrobial activity when compared with the traditional sequential protocol [25, 27, 37,38,39,40,41,42]. Pedrinha et al. [43] reported that NaOCl + EDTA-T (i.e., EDTA plus sodium lauryl ether sulfate) showed the best intratubular antibacterial activity. Furthermore, the addition of HEBP delayed the anti-biofilm action of NaOCl but did not compromise its antimicrobial efficacy [44]. However, none of the solutions were able to completely eliminate bacteria from the root canals.
Dentine erosion
Table 3 lists the studies retrieved for dentine erosion outcome. Three of ten selected laboratory studies were blinded and randomized on extracted human teeth [3, 33, 34], four did not report blinding procedures for examiners [17, 45,46,47] and three did not specify blinding or randomization techniques [48,49,50]. Two studies tested HEBP (9–18%) alone [48, 50], eight combined with different NaOCl concentrations (1.3–5%) [17, 34, 45,46,47,48,49,50], one with NaOCl-Chlorhexidine [49], one in an aqueous gel consisting of 2% alginate, 3% aerosil, 10% Tween 80 [3] and one with EDTA to obtain Na2 and Na4 salts of HEDP [33].
Testing methods to assess the dentine erosion and roughness modification were varied and included nanoindenter [50], Vickers microhardness test [45], SEM [17, 34, 50], atomic absorption spectroscopy [17, 33], attenuated total reflectance in Fourier-transform infrared spectroscopy [48], scanning light and transmission microscopies [47], Fourier-transform infrared spectroscopy [47], energy-dispersive-X-ray spectroscopy [47], profilometer [46] and roughness measuring station [46].
Overall, HEDP liquid irrigant solutions seemed to be milder chelating agents compared to those with EDTA, thus resulting in reduced or no dentine erosion and roughness modification when the continuous chelation protocol was used [17, 33, 34, 45, 47,48,49]. Conversely, Ulusoy et al. [50] reported that final irrigation with etidronic acid alone or in association with NaOCl altered structurally the root canal dentine. According to Girard et al. [3], the tested HEBP gel demonstrated major calcium chelating capacity compared with the marketed paste-type chelator products containing EDTA and hydrogen peroxide. Finally, Tartari et al. [46] showed that NaOCl did not influence the surface roughness; only the irrigation protocols including chelating agents modified the roughness of root dentine.
Discussion
Smear layer and debris removal
Mechanical instrumentation of the root canal is likely to produce hard debris [13] and inorganic shavings, generating a smear layer [51, 52] that covers the walls of the prepared root canal [53, 54]. More specifically, smear layer was defined as “a layer of material composed of dentine, remnants of pulp tissue and odontoblastic processes, and sometimes bacteria” [55] and debris may contain “pulp tissue fragments, necrotic tissue, microorganisms, dentine chips and canal irrigants” [56]. Accumulated hard-tissue debris is clinically unfavourable, because it is conceivable that microorganisms remaining in anatomical ramifications after instrumentation may be protected by debris from disinfectants that are used in the main root canal system [13]. Moreover, accumulated debris might negatively affect the canal sealability [57] and interfere with NaOCl antimicrobial activity, reducing its effectiveness due the inability of the NaOCl solution to dissolve the smear layer [41]. This mechanism could be explained by the function barrier exerted by smear layer and the accelerated consumption of free available chlorine mediated by the organic components [27, 58, 59]. NaOCl cannot dissolve inorganic smear layer components [9]. Hence, the use of calcium-complexing (chelating) agents is suggested. They can be applied in a liquid or past-type formulation [9]. Several studies evaluated the efficacy of HEBP as an alternative to traditional chelating agents such as EDTA. Evidence from the included studies is limited by the extreme variability in terms of concentration of the NaOCl irrigant solutions, the irrigant formulation (i.e., liquid and paste-type), the type and concentration of HEBP, the time of irrigant application and the measurement of outcome. All included studies were randomized and conducted on extracted teeth or samples of teeth. Only one study [17] did not specify whether it was blinded; the others were blinded.
According to Kfir et al. [34] and Lottanti [17], cleanliness of HEDP-based irrigating solutions was not significantly different from NaOCl, followed by EDTA [17, 34]. Interestingly, the apical part did not present debris [34], in contrast with some previous studies which showed the apical part was associated with a notable quantity of debris when a syringe and needle were used for an irrigation procedure [60, 61]. Kfir et al. [34] suggest that this difference could be due to the small dimensions of the irrigation needle used (i.e., 30 G) which ensured to achieve the last 1–2 mm from the root canal apex, resulting in an effective cleanliness of the apical part. Furthermore, these contrasting findings could also due to a methodological systematic error occurred in previous studies, as suggested by Lottanti et al. [17]. Indeed, conventional investigations assessed the amount of smear layer on root canal walls evaluating exclusively the number of open tubules in a limited canal wall area. However, tubular sclerosis is most accentuated in the apical zona [62] and consequently, this physiological condition could have affected the smear layer evaluation in this anatomical area.
As reported by Deari et al. [33], smear layer removal by chelating agents such as EDTA and HEDP could be affected by pH values. More specifically, the sodium ions present in tetra-sodium salts induced an alkaline pH in solution. This caused a reduction of the decalcifying action of both molecules under investigation (i.e., EDTA and HEDP) in comparison with their disodium preparations. Moreover, they stated that EDTA was a stronger chelator than HEDP.
Patil et al. [35] reported that sequential use of 5.25% NaOCl with surfactant + 17% EDTA with surfactant was more efficient than a mixture of Doxycycline/citric acid/detergent and of Chloroquick (etidronic acid based-solution) in the smear layer elimination from the apical third. A direct comparison with other included studies is challenging because of the differences in methodological procedures, including the agent formulation, the use of surfactant, the sample, and the procedure overall. According to Girard et al. [3], the HEBP gel exhibited higher hypochlorite compatibility, calcium chelating ability, and smear layer preventing action when compared with paste-type chelator products with EDTA and hydrogen peroxide available into the market. Nevertheless, one possible limit of paste-type chelators use is the difficulty in achieving a smear-free apical root canal portion [9]. Rotating instruments can move the chelator away from the apical area, reducing the action of the calcium chelating agent in that area. Therefore, an additional chelating solution delivered by a fine needle should be used to reach the apical zone at the end of shaping [3].
When comparing different studies on smear layer removal by endodontic irrigants, methodological pitfalls frequently affect the results obtained [63]. Studies on dentine surface topography frequently use SEM [34]. Scanning electron microscope analysis of root canal walls has been a matter of extensive discussion in the late 2000s. Obvious biases were identified and discussed previously [63, 64]. The smear layer is a phenomenon that depends on dentine instrumentation. Thus, it is difficult to know if the observed areas after treatment were smear layer free before the SEM analysis [63]. It assesses a small area of the root canal that may be not representative of the entire surface. Additionally, it is commonly unknown how such areas are chosen during evaluation or whether the operator is blinded to them (i.e., operator bias) [65]. Moreover, quantifying smear layer presence can be complicated by the extent of sclerotic dentin in samples [62]. Finally, issues arise when drying and coating specimens since these processes can introduce various artefacts [63].
Overall, the results by score-based conventional SEM studies are not trustworthy and reproducible [63]. A valid alternative could be the 3D laser scanning microscope. It allows a simplified sample management at environmental conditions, ensuring high-quality images [33]. Micro-CT could be considered a valid alternative for assessing hard debris reduction[13]. Finally, it is important to emphasize that any type of irrigant cannot guarantee total cleaning of the root space and additional methods of cleaning should be considered [34]. Activation methods of the irrigant, such as mechanical scrubbing [66] or XP-Finisher (FKG Dentaire, La Chaux de-Fonds, Switzerland) [67] may influence the removal of debris and smear layer mainly from the apical root canal [34]. These laboratory-based results do not allow definitive conclusions to be reached about the substances tested. Indeed, clinical performance can be affected by multiple factors, such as the presence of blood and tissue remnants [3].
Within the methodological and procedural differences between the included studies, etidronate-based solutions and the continuous chelation protocol seem to be equally or more effective in the cleanliness of root canals when compared with traditional chelating agents and the sequential protocol. Yet, the 2D methodologies employed limit the clinical reliability of these results.
Antimicrobial efficacy
Dentine infection is linked with pulp necrosis and the presence of biofilms in the root canal space. The complexity of the anatomical space prevents mechanical instrumentation alone from removing adherent biofilm [68]. Sodium hypochlorite is widely used for the removal of biofilm in the root canal space. The antimicrobial efficacy of NaOCl is dependent on its free chlorine form, which is influenced by several factors such as concentration, exposure time, pH, temperature, interaction with other organic or inorganic substances, or interaction with chelating agents [25, 59]. Combining an oxidizing agent (e.g., NaOCl) with a chelating agent (e.g., EDTA or citric acid) causes a chemical interaction and exothermic reaction [69]. The reaction reduces the amount of chlorine in NaOCl solutions, which makes the solutions less antimicrobial and less able to dissolve pulp [37].
Although differences in the methodology, substrate and volumes of NaOCl make comparison difficult, all included studies demonstrated that HEBP did not interfere with the antimicrobial ability of NaOCl [25, 38, 39, 42, 44] and under certain circumstances, may significantly increase the bacterial reduction [27, 37, 40, 41]. Indeed, the continuous chelation protocol penetrated deeper into the bacterial biofilm matrix, disrupting it and exposing the bacteria to NaOCl action [42]. Interestingly, according to Neelakantan et al. [42], NaOCl plus etidronic acid or NaOCl-EDTA-NaOCl guaranteed better dentinal tubule disinfection than NaOCl-EDTA. Consequently, the application of a disinfecting solution (e.g., NaOCl) after EDTA and continuous chelation caused significantly higher bacterial reduction.
Furthermore, some studies investigated the influence of smear layer or dentine powder on the antimicrobial activity of NaOCl alone or combined with HEBP [27, 37, 41]. Interestingly, in the study of Arias-Moliz et al. [27], a significantly higher antimicrobial activity emerged in the 1% HEBP solution compared with the solution without the chelator. This phenomenon could be due to the interaction of HEBP with biofilm structure and the inorganic components of infected dentine [17] which causes the bacteria detachment from the dentine surface also with sub-lethal chlorine concentration [27]. In addition, the mixing of HEBP and 2.5% NaOCl prevented NaOCl inactivation by dentine when dentine powder was present. These results are in agreement with those obtained by Morago et al. [41] who reported that the antimicrobial activity of 9% HEBP–2.5% NaOCl was not impacted by the smear layer. The higher activity of the combination of NaOCl with HEBP rather than NaOCl alone may be associated with the HEBP ability to remove the smear layer [17], probably allowing NaOCl to penetrate better into the dentine structure to exert its bactericidal action [41]. When the smear layer is present, the limited bactericidal action of NaOCl in all concentrations may be related to its inability to dissolve the smear layer [11]. This phenomenon has multiple explanations. First, the interaction between NaOCl and organic components of the smear layer could accelerate the consumption of the available free chlorine, thus deactivating the solution [27, 59]. Second, the smear layer may act as a barrier, preventing the irrigant from reaching infected dentinal tubules [41].
Nevertheless, according to Giardino et al. [37], adding a compatible chelator (i.e., corresponding to Dual Rinse HEDP in that study) to a NaOCl solution may increase its surface tension. The high surface tension could represent an obstacle for irrigating solution in achieving the root canal space for an extensive cleaning [37]. Conversely, the NaOCl/Dual Rinse HEDP mixture exhibited a better antibacterial action than NaOCl + EDTA. This result could be explained by the fact that this weak chelator, once dissolved in NaOCl, did not alter the antimicrobial action of NaOCl with no significant reduction of chlorine available within the first 60 min [25]. Moreover, the combination of etidronate powder with NaOCl makes the solution hypertonic and could intensify the antimicrobial efficacy by means of an osmotic effect. Indeed, hypertonic salt solutions are able to promote bacterial cell death and diminish the cohesion of biofilm matrices [70, 71].
According to Pedrinha et al. [43], NaOCl + EDTA-T showed the best intratubular antibacterial activity, particularly associated with XP-Endo Finisher activation, when compared with 5% NaOCl + 18% HEBP. The main methodological difference with the previous study is the application of activation techniques for irrigants. Mechanical devices and sonic, ultrasonic, and lasers techniques have been proposed as additional methods to increase the antibacterial and anti-biofilm activity of root canal irrigants, including etidronate [42, 72,73,74,75]. Nevertheless, the efficacy evaluation of the above tools was beyond the scope of the present review.
Generally, studies on the antimicrobial efficacy of irrigant solutions employ a single-species culture of E. faecalis [37, 41]. Although endodontic infections are polymicrobial [41, 76], this bacterial strain is widely selected in laboratory studies, because most endodontic retreatments were found to be caused by Enterococcus faecalis [77, 78]. The culture-based method has been considered the gold standard to evaluate the residual infection in the root canal space [79]. Anyway, assessing the antimicrobial activity of an irrigant on dentine substrate presents some limitations due to the culture methods employed [38]. Most of the included studies on the antimicrobial activity of irrigating solutions used Confocal Laser Scanning Microscope (CLSM) analysis. In contrast to traditional culture methods, CLSM analysis makes it possible to assess the proportion of dead/living bacteria without interfering with the cells attached to the substrate [39, 80, 81].
It is pivotal to underline that root canal anatomy is complex and direct applications of laboratory results in clinical practice require prudence [25, 42]. Despite these limitations, based on the results of the included studies, the continuous chelation protocol seems to be equally or more effective in antimicrobial activity when compared with the traditional sequential protocol.
Dentine erosion
Chelator-induced erosion of the root canal walls negatively affects the mechanical properties of dentine [20, 82, 83]. Most of the included studies confirmed that HEDP was milder than EDTA in inducing dentine demineralization [17, 33, 45, 47, 48]. Conversely, Ulusoy et al. [50] reported that final irrigation with etidronic acid alone or in association with NaOCl altered structurally the root canal dentine compared with a single chelator and a chelator combined with NaOCl. These findings are probably related to the methodological procedure, including exposure time, irrigating protocol, and outcome measure. Studying the root canal appearance by images, indeed, could be misleading because of the notable heterogeneity of root dentine [17]. More sensitive alternatives to investigate directly and indirectly how irrigants modify the composition of dentine are digital techniques such as energy-dispersive X-ray spectroscopy (EDS) [84, 85], atomic force microscopic imaging (AFM) [84], microhardness and roughness tests [86] and Attenuated Total Reflectance in Fourier Transform Infrared Spectroscopy (ATR-FTIR) [87]. The considerations previously mentioned on limits of SEM are equally valid for dentin erosion investigations [63].
A study comparing the chelating ability of gel solutions containing HEDP or EDTA reported that the HEBP had superior calcium chelating capacity as opposed to the available paste-type chelator products constituted by EDTA and hydrogen peroxide [3]. Also, in this situation, it is complex to compare these results with those of previous studies due to the methodological differences such as composition and type of irrigant tested (i.e., gel vs liquid). As observed for smear layer removal, calcium chelation seems to be affected by pH solution [33]. More specifically, considering the di-and tetra-sodium salts, the high quantity of metal ions in the tetra-sodium formulation may impact the chelation activity of the sequestrant, with less chelation for Na4. Of note, the disodium salt solutions exhibited a lower pH compared to the tetra-sodium ones, which could have influenced the calcium dissolution from dentine discs. These results are in agreement with previously published data [48, 49]. In addition, EDTA and HEDP chelators induced different patterns of dentine decalcification. As reported by Rath et al. [47], dentine surface exposed to the NaOCl/EDTA protocol exhibited “naked” collagen fibers that were free of mineral encapsulation. On the other hand, the NaOCl/HEDP protocol presented a surface erosion and disorientation of the organic matrix at the interface. However, the collagen fibrils were embedded by minerals and a uniform structure of organic and inorganic elements was still appreciable [47]. Such limited alterations of dentine composition with no modifications in the amide and phosphate ratio have been previously reported [49, 88].
The collagen microstructure has a pivotal role in determining the biomechanical properties of dentine. More in detail, the fracture toughness of dentine depends on collagen and water content [89, 90]. Consequently, any procedure that alters the fibrillary arrangement of dentine matrix negatively impacted the flexural strength, potentially favouring the dentine fracture [91, 92]. Moreover, it is expected that the exposed collagen fibers have to be encapsulated by root canal sealers such as epoxy resins [93]. Anyway, exposed collagen fibers free of mineral protection or not embedded by root canal fillings are susceptible to bacteria-derived proteolytic enzymes [94], contributing to clinical failure [34]. Changes occurring in dentine structure may also influence the surface roughness of dentine tissue [46]. A limited enhancement in surface roughness could be clinically auspicious, because it may increase the micromechanical bonding of root canal sealers [86, 95]. Nevertheless, accentuated roughness can promote bacterial colonization [96]. According to Tartari et al. [49], HEDP did not alter the dentine roughness, whereas EDTA did. Kfir et al. [34] reported the HEDP-based irrigation solution was not significantly different from 3% NaOCl + EDTA in causing erosion of the canal wall. Conversely, as reported by Tartari et al. [46], the regimens that employed citric acid and HEBP combined with NaOCl showed a greater increase in roughness than other groups, including those containing EDTA. The different findings are probably related to the methodological conditions, including the irrigation protocol, application time, irrigant concentration, and the technique of analysis used for measuring dentine hardness.
Within the methodological differences between the included studies, on the basis of the current knowledge, HEDP irrigant seems to be a milder chelating agent compared with EDTA, thus resulting in reduced or no dentine erosion and roughness modification when the continuous chelation protocol was used. However, methodological limitations hinder the reliability of results similarly to debris removal outcome.
Scoping review guarantees a more flexible methodological approach in which the quality assessment of included studies is not mandatory, because the primary aim is to explore a broad topic for identifying the state of current knowledge, hypothetical gaps, and directing the future research [31]. For all these reasons, a scoping approach instead of a systematic was chosen. Moreover, considering the notable variety in laboratory conditions among the included studies, a meta-analysis was not conducted. Furthermore, the effect of continuous chelation on the bond strength of endodontic sealers, root transportation, and fracture resistance has not been assessed in the current review and requires further investigation.
In addition, the included studies presented notable differences regarding the type of samples, the irrigation protocol, the application time and concentration of irrigant solution, the outcome and measurement. Hence, a comparison is challenging, and the findings should be interpreted with caution. Moreover, the above-mentioned limitations of two-dimensional investigation methods prevent from obtaining reliable and trustworthy results especially for smear layer/debris removal and dentin erosion outcomes. Future studies should be based on three-dimensional techniques which allow a straightforward, standardized and not operator-dependent sample analysis.
Despite the standardized conditions, laboratory studies cannot fully reproduce the complexity of oral conditions, including pH, dentine structure and ageing and root canal microbiota. When the outcome allows it, high-quality randomized clinical trials should be preferred.
Conclusions
Overall, most of the included studies showed that continuous chelation seems to be equally or more effective in smear layer/debris removal, antimicrobial activity, and dentine erosion when compared with the traditional sequential protocol. Yet, included studies differ among each other in terms of samples, irrigation protocol, application time and concentration of irrigant solution and outcome measure making comparison difficult. Moreover, investigation methods applied in the current research are often inadequate (i.e., SEM). For future laboratory-based studies to be more informative, they should use a standardized and comparable experimental protocol with reliable and unbiased investigation methods.
Data availability
Data sharing not applicable—no new data generated, or the article describes entirely theoretical research.
References
Gagliani MM, Gorni FG, Strohmenger L. Periapical resurgery versus periapical surgery: a 5-year longitudinal comparison. Int Endod J. 2005;38(5):320–7.
Orstavik D, Pitt Ford TR. Apical periodontitis: microbial infection and host responses. Essential endodontology: prevention and treatment of apical periodontitis. 2nd ed. Oxford: Wiley-Blackwell; 2007.
Girard S, Paqué F, Badertscher M, Sener B, Zehnder M. Assessment of a gel-type chelating preparation containing 1-hydroxyethylidene-1, 1-bisphosphonate. Int Endod J. 2005;38(11):810–6.
Peters OA, Schönenberger K, Laib A. Effects of four Ni-Ti preparation techniques on root canal geometry assessed by micro computed tomography. Int Endod J. 2001;34(3):221–30.
Byström A, Sundqvist G. Bacteriologic evaluation of the effect of 0.5 percent sodium hypochlorite in endodontic therapy. Oral Surg Oral Med Oral Pathol. 1983;55(3):307–12.
Hülsmann M, Rödig T. Problems in disinfection of the root canal system. In: Hülsmann M, Shäfer E, editors. Problems in endodontics: etiology, diagnosis and treatment. London: Quintessence; 2009. p. 253–92.
Ordinola-Zapata R, Bramante CM, Cavenago B, Graeff MS, Gomes de Moraes I, Marciano M, Duarte MA. Antimicrobial effect of endodontic solutions used as final irrigants on a dentine biofilm model. Int Endod J. 2012;45(2):162–8.
Tagelsir A, Yassen GH, Gomez GF, Gregory RL. Effect of antimicrobials used in regenerative endodontic procedures on 3-week-old enterococcus faecalis biofilm. J Endod. 2016;42(2):258–62.
Hülsmann M, Heckendorff M, Lennon A. Chelating agents in root canal treatment: mode of action and indications for their use. Int Endod J. 2003;36(12):810–30.
Haapasalo M, Qian W, Portenier I, Waltimo T. Effects of dentin on the antimicrobial properties of endodontic medicaments. J Endod. 2007;33(8):917–25.
Wang Z, Shen Y, Haapasalo M. Effect of smear layer against disinfection protocols on Enterococcus faecalis-infected dentin. J Endod. 2013;39(11):1395–400.
Adigüzel O, Yiğit-Özer S, Kaya S, Uysal İ, Ganidağli-Ayaz S, Akkuş Z. Effectiveness of ethylenediaminetetraacetic acid (EDTA) and MTAD on debris and smear layer removal using a self-adjusting file. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(6):803–8.
Paqué F, Rechenberg DK, Zehnder M. Reduction of hard-tissue debris accumulation during rotary root canal instrumentation by etidronic acid in a sodium hypochlorite irrigant. J Endod. 2012;38(5):692–5.
Rossi-Fedele G, Doğramaci EJ, Guastalli AR, Steier L, de Figueiredo JA. Antagonistic interactions between sodium hypochlorite, chlorhexidine, EDTA, and citric acid. J Endod. 2012;38(4):426–31.
Zehnder M, Kosicki D, Luder H, Sener B, Waltimo T. Tissue-dissolving capacity and antibacterial effect of buffered and unbuffered hypochlorite solutions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(6):756–62.
Goldman M, Goldman LB, Cavaleri R, Bogis J, Lin PS. The efficacy of several endodontic irrigating solutions: a scanning electron microscopic study: Part 2. J Endod. 1982;8(11):487–92.
Lottanti S, Gautschi H, Sener B, Zehnder M. Effects of ethylenediaminetetraacetic, etidronic and peracetic acid irrigation on human root dentine and the smear layer. Int Endod J. 2009;42(4):335–43.
Lima Nogueira BM, da Costa Pereira TI, Pedrinha VF, de Almeida RP. Effects of different irrigation solutions and protocols on mineral content and ultrastructure of root canal dentine. Iran Endod J. 2018;13(2):209–15.
Cecchin D, Soares Giaretta V, Granella Cadorin B, Albino Souza M, Vidal CMP, Paula FA. Effect of synthetic and natural-derived novel endodontic irrigant solutions on mechanical properties of human dentin. J Mater Sci Mater Med. 2017;28(9):141.
Mai S, Kim YK, Arola DD, Gu LS, Kim JR, Pashley DH, Tay FR. Differential aggressiveness of ethylenediamine tetraacetic acid in causing canal wall erosion in the presence of sodium hypochlorite. J Dent. 2010;38(3):201–6.
Wagner MH, da Rosa RA, de Figueiredo J, Duarte M, Pereira JR, Só M. Final irrigation protocols may affect intraradicular dentin ultrastructure. Clin Oral Investig. 2017;21:2173–82.
Cochrane S, Burrow MF, Parashos P. Effect on the mechanical properties of human and bovine dentine of intracanal medicaments and irrigants. Aust Dent J. 2019;64(1):35–42.
Tartari T, Guimarães BM, Amoras LS, Duarte MA, Silva e Souza PA, Bramante CM. Etidronate causes minimal changes in the ability of sodium hypochlorite to dissolve organic matter. Int Endod J. 2015;48(4):399–404.
Wright PP, Kahler B, Walsh LJ. The effect of heating to intracanal temperature on the stability of sodium hypochlorite admixed with etidronate or EDTA for continuous chelation. J Endod. 2019;45(1):57–61.
Zehnder M, Schmidlin P, Sener B, Waltimo T. Chelation in root canal therapy reconsidered. J Endod. 2005;31(11):817–20.
Paulson L, Ballal NV, Bhagat A. Effect of root dentin conditioning on the pushout bond strength of biodentine. J Endod. 2018;44(7):1186–90.
Arias-Moliz MT, Morago A, Ordinola-Zapata R, Ferrer-Luque CM, Ruiz-Linares M, Baca P. Effects of dentin debris on the antimicrobial properties of sodium hypochlorite and etidronic acid. J Endod. 2016;42(5):771–5.
Zehnder M. Root canal irrigants. J Endod. 2006;32(5):389–98.
Estrela C, Costa E Silva R, Urban RC, Gonçalves PJ, Silva JA, Estrela CRA, Pecora JD, Peters OA. Demetallization of Enterococcus faecalis biofilm: a preliminary study. J Appl Oral Sci. 2018;26:e20170374.
Wright PP, Kahler B, Walsh LJ. Alkaline sodium hypochlorite irrigant and its chemical interactions. Materials (Basel). 2017;10(10):1147.
Daudt HM, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13:48.
Tricco AC, Lillie E, Zarin W, O’Brien KK, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Deari S, Mohn D, Zehnder M. Dentine decalcification and smear layer removal by different ethylenediaminetetraacetic acid and 1-hydroxyethane-1,1-diphosphonic acid species. Int Endod J. 2019;52(2):237–43.
Kfir A, Goldenberg C, Metzger Z, Hülsmann M, Baxter S. Cleanliness and erosion of root canal walls after irrigation with a new HEDP-based solution vs. traditional sodium hypochlorite followed by EDTA. A scanning electron microscope study. Clin Oral Investig. 2020;24(10):3699–706.
Patil PH, Gulve MN, Kolhe SJ, Samuel RM, Aher GB. Efficacy of new irrigating solution on smear layer removal in apical third of root canal: a scanning electron microscope study. J Conserv Dent. 2018;21(2):190–3.
Ulusoy ÖI, Savur IG, Alaçam T, Çelik B. The effectiveness of various irrigation protocols on organic tissue removal from simulated internal resorption defects. Int Endod J. 2018;51(9):1030–6.
Giardino L, Del Fabbro M, Morra M, Pereira T, de Bombarda AF, Savadori P. Generali L. Dual Rinse® HEDP increases the surface tension of NaOCl but may increase its dentin disinfection efficacy. Odontology. 2019;107(4):521–9.
Arias-Moliz MT, Ordinola-Zapata R, Baca P, Ruiz-Linares M, Ferrer-Luque CM. Antimicrobial activity of a sodium hypochlorite/etidronic acid irrigant solution. J Endod. 2014;40(12):1999–2002.
Arias-Moliz MT, Ordinola-Zapata R, Baca P, Ruiz-Linares M, García García E, Hungaro Duarte MA, Monteiro Bramante C, Ferrer-Luque CM. Antimicrobial activity of chlorhexidine, peracetic acid and sodium hypochlorite/etidronate irrigant solutions against Enterococcus faecalis biofilms. Int Endod J. 2015;48(12):1188–93.
Campello AF, Rodrigues RCV, Alves FRF, Miranda KR, Brum SC, Mdala I, Siqueira JF Jr, Rôças IN. Enhancing the intracanal antibacterial effects of sodium hypochlorite with etidronic acid or citric acid. J Endod. 2022;48(9):1161–8.
Morago A, Ordinola-Zapata R, Ferrer-Luque CM, Baca P, Ruiz-Linares M, Arias-Moliz MT. Influence of smear layer on the antimicrobial activity of a sodium hypochlorite/etidronic acid irrigating solution in infected dentin. J Endod. 2016;42(11):1647–50.
Neelakantan P, Cheng CQ, Mohanraj R, Sriraman P, Subbarao C, Sharma S. Antibiofilm activity of three irrigation protocols activated by ultrasonic, diode laser or Er:YAG laser in vitro. Int Endod J. 2015;48(6):602–10.
Pedrinha VF, Cardenas Cuellar MR, Velásquez-Espedilla EG, Duarte MAH, Andrade FB, Rodrigues PA. Impact of irrigation protocols with some chelators and mechanical agitation on intratubular decontamination. Braz Oral Res. 2021;35: e127.
Borges MMB, Dijkstra RJB, de Andrade FB, Duarte MAH, Versluis M, van der Sluis LWM, Petridis X. The response of dual-species bacterial biofilm to 2% and 5% NaOCl mixed with etidronic acid: a laboratory real-time evaluation using optical coherence tomography. Int Endod J. 2022;55(7):758–71.
Dineshkumar MK, Vinothkumar TS, Arathi G, Shanthisree P, Kandaswamy D. Effect of ethylene diamine tetra-acetic acid, MTAD™, and HEBP as a final rinse on the microhardness of root dentin. J Conserv Dent. 2012;15(2):170–3.
Tartari T, Duarte Junior AP, Silva Júnior JO, Klautau EB, Silva E Souza Junior MH, Silva E Souza Junior PA. Etidronate from medicine to endodontics: effects of different irrigation regimes on root dentin roughness. J Appl Oral Sci. 2013;21(5):409–15.
Rath PP, Yiu CKY, Matinlinna JP, Kishen A, Neelakantan P. The effects of sequential and continuous chelation on dentin. Dent Mater. 2020;36(12):1655–65.
Tartari T, Oda DF, Zancan RF, da Silva TL, de Moraes IG, Duarte MA, Bramante CM. Mixture of alkaline tetrasodium EDTA with sodium hypochlorite promotes in vitro smear layer removal and organic matter dissolution during biomechanical preparation. Int Endod J. 2017;50(1):106–14.
Tartari T, Wichnieski C, Bachmann L, Jafelicci M Jr, Silva RM, Letra A, van der Hoeven R, Duarte MAH, Bramante CM. Effect of the combination of several irrigants on dentine surface properties, adsorption of chlorhexidine and adhesion of microorganisms to dentine. Int Endod J. 2018;51(12):1420–33.
Ulusoy Öİ, Mantı AŞ, Çelik B. Nanohardness reduction and root dentine erosion after final irrigation with ethylenediaminetetraacetic, etidronic and peracetic acids. Int Endod J. 2020;53(11):1549–58.
Koskinen KP, Meurman JH, Stenvall H. Appearance of chemically treated root canal walls in the scanning electron microscope. Scand J Dent Res. 1980;88(5):397–405.
Lester KS, Boyde A. Scanning electron microscopy of instrumented, irrigated and filled root canals. Br Dent J. 1977;143(11):359–67.
Eick JD, Wilko RA, Anderson CH, Sorensen SE. Scanning electron microscopy of cut tooth surfaces and identification of debris by use of the electron microprobe. J Dent Res. 1970;49(6):1359–68.
McComb D, Smith DC. A preliminary scanning electron microscopic study of root canals after endodontic procedures. J Endod. 1975;1(7):238–42.
Sen BH, Wesselink PR, Türkün M. The smear layer: a phenomenon in root canal therapy. Int Endod J. 1995;28(3):141–8.
Elmsallati EA, Wadachi R, Suda H. Extrusion of debris after use of rotary nickel-titanium files with different pitch: a pilot study. Aust Endod J. 2009;35(2):65–9.
Violich DR, Chandler NP. The smear layer in endodontics—a review. Int Endod J. 2010;43(1):2–15.
Clark-Holke D, Drake D, Walton R, Rivera E, Guthmiller JM. Bacterial penetration through canals of endodontically treated teeth in the presence or absence of the smear layer. J Dent. 2003;31(4):275–81.
Macedo RG, Wesselink PR, Zaccheo F, Fanali D, Van Der Sluis LW. Reaction rate of NaOCl in contact with bovine dentine: effect of activation, exposure time, concentration and pH. Int Endod J. 2010;43(12):1108–15.
Paqué F, Musch U, Hülsmann M. Comparison of root canal preparation using RaCe and ProTaper rotary Ni-Ti instruments. Int Endod J. 2005;38(1):8–16.
Versümer J, Hülsmann M, Schäfers F. A comparative study of root canal preparation using Profile .04 and Lightspeed rotary Ni-Ti instruments. Int Endod J. 2002;35(1):37–46.
Vasiliadis L, Darling AI, Levers BG. The amount and distribution of sclerotic human root dentine. Arch Oral Biol. 1983;28(7):645–9.
De-Deus G, Reis C, Paciornik S. Critical appraisal of published smear layer-removal studies: methodological issues. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(4):531–43.
Zehnder M. Research that matters – irrigants and disinfectants. Int Endod J. 2012;45:961–2.
Hülsmann M, Peters OA, Dummer PMH. Mechanical preparation of root canals: shaping goals, techniques and means. Endod Topics. 2005;10:30–76.
Metzger Z, Solomonov M, Kfir A. The role of mechanical instrumentation in the cleaning of root canals. Endod Topics. 2013;29:87109.
Elnaghy AM, Mandorah A, Elsaka SE. Effectiveness of XP-endo finisher, endoactivator, and file agitation on debris and smear layer removal in curved root canals: a comparative study. Odontology. 2017;105(2):178–83.
Nair PN, Henry S, Cano V, Vera J. Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after “one-visit” endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(2):231–52.
Clarkson RM, Podlich HM, Moule AJ. Influence of ethylenediaminetetraacetic acid on the active chlorine content of sodium hypochlorite solutions when mixed in various proportions. J Endod. 2011;37(4):538–43.
de Almeida J, Hoogenkamp M, Felippe WT, Crielaard W, van der Waal SV. Effectiveness of EDTA and modified salt solution to detach and kill cells from enterococcus faecalis biofilm. J Endod. 2016;42(2):320–3.
van der Waal SV, van der Sluis LW, Özok AR, Exterkate RA, van Marle J, Wesselink PR, de Soet JJ. The effects of hyperosmosis or high pH on a dual-species biofilm of enterococcus faecalis and pseudomonas aeruginosa: an in vitro study. Int Endod J. 2011;44(12):1110–7.
Cachovan G, Schiffner U, Altenhof S, Guentsch A, Pfister W, Eick S. Comparative antibacterial efficacies of hydrodynamic and ultrasonic irrigation systems in vitro. J Endod. 2013;39(9):1171–5.
de Gregorio C, Estevez R, Cisneros R, Heilborn C, Cohenca N. Effect of EDTA, sonic, and ultrasonic activation on the penetration of sodium hypochlorite into simulated lateral canals: an in vitro study. J Endod. 2009;35(6):891–5.
De Moor RJ, Blanken J, Meire M, Verdaasdonk R. Laser induced explosive vapor and cavitation resulting in effective irrigation of the root canal. Part 2: evaluation of the efficacy. Lasers Surg Med. 2009;41(7):520–3.
Halford A, Ohl CD, Azarpazhooh A, Basrani B, Friedman S, Kishen A. Synergistic effect of microbubble emulsion and sonic or ultrasonic agitation on endodontic biofilm in vitro. J Endod. 2012;38(11):1530–4.
Farrugia C, Baca P, Camilleri J, Arias Moliz MT. Antimicrobial activity of ProRoot MTA in contact with blood. Sci Rep. 2017;7:41359.
Rôças IN, Siqueira JF Jr, Santos KR. Association of Enterococcus faecalis with different forms of periradicular diseases. J Endod. 2004;30(5):315–20.
Sundqvist G, Figdor D, Persson S, Sjögren U. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(1):86–93.
Shuping GB, Orstavik D, Sigurdsson A, Trope M. Reduction of intracanal bacteria using nickel-titanium rotary instrumentation and various medications. J Endod. 2000;26(12):751–5.
Guerreiro-Tanomaru JM, Nascimento CA, Faria-Júnior NB, Graeff MS, Watanabe E, Tanomaru-Filho M. Antibiofilm activity of irrigating solutions associated with cetrimide. Confocal laser scanning microscopy. Int Endod J. 2014;47(11):1058–63.
Shen Y, Stojicic S, Haapasalo M. Bacterial viability in starved and revitalized biofilms: comparison of viability staining and direct culture. J Endod. 2010;36(11):1820–3.
Marending M, Paqué F, Fischer J, Zehnder M. Impact of irrigant sequence on mechanical properties of human root dentin. J Endod. 2007;33(11):1325–8.
Saleh AA, Ettman WM. Effect of endodontic irrigation solutions on microhardness of root canal dentine. J Dent. 1999;27(1):43–6.
Zelic K, Milovanovic P, Rakocevic Z, Askrabic S, Potocnik J, Popovic M, Djuric M. Nano-structural and compositional basis of devitalized tooth fragility. Dent Mater. 2014;30(5):476–86.
Wang Z, Maezono H, Shen Y, Haapasalo M. Evaluation of root canal dentin erosion after different irrigation methods using energy-dispersive x-ray spectroscopy. J Endod. 2016;42(12):1834–9.
Ballal NV, Mala K, Bhat KS. Evaluation of the effect of maleic acid and ethylenediaminetetraacetic acid on the microhardness and surface roughness of human root canal dentin. J Endod. 2010;36(8):1385–8.
Tartari T, Bachmann L, Maliza AG, Andrade FB, Duarte MA, Bramante CM. Tissue dissolution and modifications in dentin composition by different sodium hypochlorite concentrations. J Appl Oral Sci. 2016;24(3):291–8.
Becker LC. Safety assessment of etidronic acid and its simple salts as used in cosmetics. Cosmetic Ingredient Review 2016:1–48.
Kishen A, Asundi A. Experimental investigation on the role of water in the mechanical behavior of structural dentine. J Biomed Mater Res Part A. 2005;73:192–200.
Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod Topics. 2006;13:57–83.
Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002;18(3):134–7.
Zhang K, Kim YK, Cadenaro M, Bryan TE, Sidow SJ, Loushine RJ, Ling JQ, Pashley DH, Tay FR. Effects of different exposure times and concentrations of sodium hypochlorite/ethylenediaminetetraacetic acid on the structural integrity of mineralized dentin. J Endod. 2010;36(1):105–9.
Fisher MA, Berzins DW, Bahcall JK. An in vitro comparison of bond strength of various obturation materials to root canal dentin using a push-out test design. J Endod. 2007;33(7):856–8.
Starcher B. A ninhydrin-based assay to quantitate the total protein content of tissue samples. Anal Biochem. 2001;292:125–9.
Hu X, Ling J, Gao Y. Effects of irrigation solutions on dentin wettability and roughness. J Endod. 2010;36:1064–7.
Tang L, Pillai S, Revsbech NP, Schramm A, Bischoff C, Meyer RL. Biofilm retention on surfaces with variable roughness and hydrophobicity. Biofouling. 2011;27(1):111–21.
Funding
Open access funding provided by Università degli Studi di Catania within the CRUI-CARE Agreement. No funding to declare.
Author information
Authors and Affiliations
Contributions
GRMLR, GP, VN and EP involved in conception and design and acquisition of data. GRMLR and GP involved in data analysis. VN, EP and GRMLR, GP involved in interpretation of data, reviewing, editing and final approval. GRMLR and GP involved in first draft preparation.
Corresponding author
Ethics declarations
Conflict of interest
All authors report no conflicts of interest related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
La Rosa, G.R.M., Plotino, G., Nagendrababu, V. et al. Effectiveness of continuous chelation irrigation protocol in endodontics: a scoping review of laboratory studies. Odontology 112, 1–18 (2024). https://doi.org/10.1007/s10266-023-00835-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-023-00835-8