Abstract
Intravascular laser irradiation of blood (ILIB) was developed to treat cardiovascular diseases due to its rheological effects. In its original form, ILIB was applied by an intravenous optical fiber, restricting its application. However, this technique was modified to non-invasive irradiation through the radial artery, now called vascular photobiomodulation (VPBM). Many studies have used both, ILIB and VPBM, to treat lung diseases. It is well established that lung diseases affect more than 300 million people worldwide with high morbidity and mortality rates. In this short critical review, we discuss the potential benefits of photobiomodulation to treat lung diseases using these two approaches. The search was performed in the electronic database of MEDLINE (Medical Literature Analysis and Retrieval System Online) via PubMed. The data search was carried out from 1991 to 2017. We selected a total of 10 clinical studies using either ILIB or VPBM, in addition to 2 experimental studies in animals. The respiratory diseases treated in these studies included bronchitis, asthma, pneumonia, and tuberculosis. The results showed overall beneficial effects on lung diseases, characterized by a reduction in the inflammatory cascade and antioxidant effects, improvement of hemodynamic parameters, the efficiency of gas exchange, and reduction of hospitalization periods. In conclusion, all studies showed promising effects of ILIB in both animal and human studies. The studies did not discuss any disadvantages or contraindications. However, further studies are needed in order to understand the dosimetry, and the literature is lacking in randomized, controlled clinical trials. Thus, this review highlights the need for additional studies using this approach.
Similar content being viewed by others
Introduction
Photobiomodulation (PBM) has been used in experimental and clinical studies as a therapy to promote healing and to reduce or prevent danage for over 40 years [1, 2]. This therapy can normalize biological functions either by stimulation of desirable processes or inhibition of damaging processes [3]. PBM can be applied by directly irradiating the target organ, as well as irradiating the vascular system, either transdermally or intravascularly [4]. Thus, it has become clear that PBM, depending on its application, can induce both local and systemic effects.
In its original form, when PBM was applied inside the blood vessels, it was called ILIB, an acronym for intravascular laser irradiation of the blood. This therapy was developed by Russian scientists in the 1970s to treat cardiovascular diseases due to the rheological effects of laser irradiation [5].
This technique was performed by introducing an intravenous catheter, usually in the radial artery, coupled to an optical fiber that irradiated the blood with a He–Ne laser, at a wavelength of 632 nm (red) [6]. However, the ILIB method was limited because it is an invasive therapy thus restricting its widespread application. Afterwards, ILIB was modified to become a non-invasive and relatively simple method involving transcutaneous irradiation of the radial artery. With this new approach, the term ILIB was changed as it is no longer an invasive technique, now called Vascular photobiomodulation (VPBM) [7]. Interestingly, studies have shown that transcutaneous irradiation of the radial artery with low-intensity He–Ne laser at 632 nm (red) produced similar effects to the original technique, by administering light through the skin into the blood vessels.
Both, ILIB as well as VPBM can modulate redox signaling in the mitochondria through the stimulation of components of the respiratory chain. This signaling cascade triggers beneficial effects on immunoglobulins, interferons, and interleukins [8]. Studies have shown that ILIB can have analgesic, spasmolytic, and sedative effects [9]. Besides that, it improves blood circulation, stimulates cellular metabolism in the tissue, and increases ATP synthesis [10].
Clinical and experimental studies have evaluated the therapeutic effects of light delivered by the traditional intravascular method or by the modified VPBM method to treat several diseases, including pulmonary, cardiovascular, infectious, autoimmune, connective tissue diseases, among others [11, 12]. Although the biological effects of these approaches have been established, there is still no consensus in the literature on the parameters to be used, and their effectiveness for different conditions.
Lung diseases affect more than 300 million people worldwide with high rates of morbidity and mortality. In the last 2 years due to COVID-19, there has been an increase in the number of studies investigating various therapies to treat lung infctions. Respiratory tract infections affect lung function, including impairment in gas exchange and an inability to remove foreign substances from the airways. Conventional therapies usually show some side effects, and sometimes, they only have a palliative effect. In this context, ILIB has been used as adjuvant therapy to treat lung diseases, but the studies are still at an early stage and its effectiveness is still controversial.
Here, we have undertaken a literature review on the effects of ILIB on lung diseases. It was not possible to carry out a systematic review according to PRISMA guidelines because there were not enough randomized controlled trials on this topic. Thus, this short critical review summarized the human and animal studies using either ILIB or VPBM as an adjuvant therapy to treat lung diseases. Our objective was to evaluate the effectiveness of this treatment, in order to not only show the safety of this technology, but also to highlight the lack of randomized, controlled trials. Therefore, this review emphasizes the necessity for additional studies on this topic.
Methods
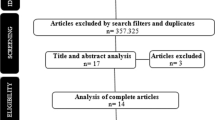
In this short critical review, we surveyed the effectiveness of PBM using both invasive and non-invasive approaches to treat lung diseases. This review included human clinical and experimental animal studies that evaluated the therapeutic effect of ILIB or VPBM in lung disease, without language restriction. Exclusion criteria were studies not related to the subject, review articles, case reports, book chapters, and congress abstracts.
The search was performed in the electronic database of MEDLINE (Medical Literature Analysis and Retrieval System Online) via PubMed. The data search was performed from 1991 to 2017. The respiratory diseases treated in these studies were bronchitis, asthma, pneumonia, and tuberculosis. Medical Subject Headings were used to select search keywords selecting Boolean operators “AND”/ “OR.” The keywords included in the search were “ILIB,” “Intravascular laser irradiation of blood,” “Photobiomodulation,” “Systemic photobiomodulation,” “Transcutaneous system photobiomodulation,” “Intravascular photobiomodulation lung disease.”
In this review, we used the term VPBM (vascular photobiomodulation) for the non-invasive technique since different anatomical sites can be irradiated, but all the sites involve vascular irradiation, whether through the radial or sublingual artery, or other blood vessels.
The search was carried out in November 2021. After an initial search, 263 articles were initially identified, but considering the inclusion and exclusion criteria, 12 articles were finally selected for discussion. Of these 12, two reported animal studies while ten described human studies (Tables 1 and 2 respectively). Also, it is important to mention that 7 out of the 10 human studies were published in the Russian language, and data from these studies were extracted only from their abstracts. Furthermore, unfortunately the dosimetry parameters were not mentioed in the abstract summary. However, given the important contribution of Russian scientists to this topic, we propose that it is reasonable and important to include such studies in the article despite not knowing the dosimetry used. Moreover, we emphasize the importance of a complete description of the methodology, especially with regard to the dosimetric parameters. Otherwise, any study cannot fulfil its real function, which is to support clinical treatments with evidence of efficacy and safety.
Results and discussion
In this short review, the manuscripts were selected according to the criteria described above, to investigate the effectiveness of ILIB or VPBM as an adjuvant therapy to treat lung diseases (Tables 1 and 2).
In Table 1, we summarize the two animal studies which used VPBM to treat two important lung diseases: acute lung injury and asthma. Both studies focused on evaluating the main biomarkers of the respective diseases, evaluating the effect of VPBM per se. In these studies, pharmacological therapy was not used.
Acute lung injury (ALI) is a severe multifactorial lung pathology characterized by diffuse alveolar injury, inflammatory cell infiltration, disruption of the alveolar epithelial barrier, alveolar edema, and impaired pulmonary gas exchange, with a high mortality rate [13]. Asthma is a chronic inflammatory disease caused by allergies or other triggers, characterized by recurrent and reversible episodes of wheezing, dyspnea, chest stiffness, and cough [14]. In the first experimental study, the authors [15] investigated the effects of VPBM on ALI. They used light light-emitting diodes (LED), although the ILIB technique originally used a laser. However, we do not believe that this difference could be a study bias since it is well established that the biological effects of laser and LED are similar, despite their physical differences [16]. The results showed the beneficial effects of VPBM in reducing important biomarkers of ALI, which are often used to determine the prognosis of the disease. VPBM reduced neutrophil migration, myeloperoxidase enzyme activity, and interleukins (IL) 1β, IL-6, and IL-17 in the lung tissue [15]. The parameters used were red LED, wavelength 660 nm; power 100 mW; energy density 5 J/cm2; total energy 15 J; and time 150 s, and the site of application was the skin overlying the caudal artery.
Other animal study using the same parameters mentioned above evaluated the effects of VPBM treatment in an animal model of asthma [17]. The authors again showed the beneficial effects of VPBM, with reduced cell migration into the lungs, and less mast cell degranulation. Considering that asthma symptoms are dependent on mast cell degranulation, which causes lung inflammation, we suggest that VPBM could be useful in asthma treatment. Moreover, VPBM increased the levels of interleukin 10 (IL-10) [17] suggesting that inflammation was reduced since this cytokine has an anti-inflammatory function. However, it is important to mention that the tracheal hyperresponsiveness was not reversed by the VPBM treatment, and this symptom is very troublesome in asthmatic patients, frequently necessitating emergency room visits.
In Table 2, we summarize the human studies, which have evaluated the effects of ILIB or VPBM in lung diseases. In all of studies listed here, PBM was used as adjuvant therapy to other treatments. We found reports of human studies using ILIB to treat pneumonia, bronchitis, asthma, and tuberculosis. However, the majority of these articles was in Russian, restricting our analysis to their abstracts [11, 12, 21,22,23,24, 27]. Unfortunatelly, the details of the PBM parameters (mainly involving lasers) were not mentioned in the abstract, which hindered the discussion, as well as limiting the future application of this technology. However, considering the important role of Russian scientists in this topic, we propose it is reasonable to include these studies in this review.
Burduli and Gabueva [12] evaluated the effect of ILIB in patients with community-acquired pneumonia. A total of 70 patients were treated with ILIB for a period of 7 days. The functional activity of neutrophils was estimated from their ability to reduce nitroblue tetrazolium (NBT) in both spontaneous and stimulated conditions. Neutrophils are the first line of defense against microorganisms, and their main function is phagocytosis and the generation of reactive oxygen and nitrogen species. The antimicrobial mechanisms of neutrophils are oxygen dependent. The NBT test is a method used for evaluating the oxidative metabolism of neutrophils. This study suggested that the inclusion of ILIB in the combined treatment regimen of patients with pneumonia promoted normalization of the bactericidal activity of neutrophils.
Prokopova et al. [18] studied the effect of ILIB at a dose of 10–30 J/cm2 in 20 children with bilateral destructive pneumonia, but they measured blood viscosity as a parameter of success. The results showed a decrease in blood viscosity and a hypocoagulative effect (reduced blood clotting) after ILIB treatment. However, this study did not assess any improvements in the actual symptoms of pneumonia. It is important to mention here that the viscosity of blood is linked with the number of circulating blood cells, and leucocytosis is a common observation in this disease. Thus, it is reasonable to propose that the reduction in blood viscosity may be related to a reduction in white blood cells caused by the anti-inflammatory effects of ILIB.
Similarly, Burduli and Aksenova [19] demonstrated the effectiveness of ILIB treatment by changing the hemodynamics from hyperkinetic into normokinetic in patients with bronchitis. Ninety-seven patients with bronchitis were divided into two groups: 47 patients received conventional treatment, while 50 patients received the same therapy plus ILIB. ILIB treatment was performed during 10 consecutive days for 20 min per session. The authors claimed that ILIB could be useful in the treatment of bronchitis, despite the fact that they did not evaluate important biomarkers of the disease, such as interleukins, airway reactivity, mucus production, among others.
Sarycheva et al. [20] also analyzed parameters related to blood cells, more specifically the morphometry and electrophoretic mobility of red blood cells in patients with infection-dependent asthma. Patients treated with conventional therapy plus ILIB showed better morphofunctional parameters of red blood cells, restoring their normal shape and their electrophoretic mobility. Patients who received only conventional therapy did not show these morphofunctional changes in the erythrocytes. The authors claimed that changes in the morphology and function of red blood cells in asthmatic patients could be corrected by ILIB. Again, these authors did not measure any symptoms or biomarkers of the disease.
Ivaniuta et al. [21] reported that ILIB had a beneficial effect on the clinical course of chronic bronchitis, including normalization of lipid peroxidation levels, a marked immune stimulant effect, anti-inflammatory activity, and also improved the rheological properties of the blood. Moreover, Mikhailov et al. [22] observed that ILIB increased the lung compliance and gas exchange efficiency in asthmatic patients. Although drug therapy is still widely used and necessary for lung diseases, ILIB therapy has been shown to be useful in conditions of hypercapnia, hypoxia, and impaired gas exchange. In addition, Ananchenko et al. [23] showed that ILIB promoted the normalization of mucociliary transport, activated phagocytosis and immune defense, cleaned the bronchial tree, and reduced airway obstruction (measured by forced expiratory volume for 1 s) in the management of exacerbations in patients with chronic bronchitis.
Kashankaia and Fedorov [11] also investigated the use of ILIB in patients with chronic obstructive bronchitis. The reported that the application of ILIB in combination with drug therapy accelerated the resolution of clinical symptoms, increased breathing efficiency, promoted the drainage of the bronchi, and facilitated the normalization of the patient’s immune status. It is important to mention that bronchitis is characterized by serious alterations in the cardiorespiratory system, including moderate pulmonary emphysema and pulmonary hypertension associated with an impairment of general health status.
Another study reported the effect of ILIB in asthma [24]. The authors showed that edema was reduced, lung elasticity was gradually restored, mast cells were stabilized with inhibition of histamine release, and bronchoconstriction was reversed. Finally, the authors reported that ILIB stabilized the asthma symptoms for up to nine months with a significant improvement in the quality of life, and the need for conventional medication was reduced. Asthma and bronchitis are two inflammatory conditions of the airways with similar symptoms, such as difficulty breathing, coughing, tightness in the chest, and tiredness. However, they have different etiologies. While in bronchitis the inflammation is caused by viruses or bacteria, in asthma there are many ambient or intrinsic factors that tigger its onset, including genetic susceptibility [25]. These factors could affect the response of these patients to various therapies. Comparing these last two studies with the others above, we can see that ILIB has important effects on pulmonary function and not only on hemodynamics.
We also found one manuscript that evaluated the efficacy of ILIB to treat progressive tuberculosis [26]. The results of treatment were evaluated by clinical and laboratory criteria obtained after 1 or 2 months. ILIB treatment increased the therapeutic effect and stimulated the resolution of the disease, and made it possible to stabilize the course of tuberculosis with less pronounced changes in the lungs. Similarly, Polyakov et al. [27] showed that ILIB applied to patients with tuberculosis in the early stages of chemotherapy led to an increased effectiveness of treatment, contributing to the cessation of bacterial excretion in the sputum and reduction of the hospitalization period. Stimulation of the immune system could be attributed to the effects of ILIB in the blood microcirculation, inducing vasodilation, analgesic effects, improving the oxygen transport in the blood, and normalizing some metabolic processes related to proteins, lipids, carbohydrates, and intracellular energy balance.
The studies mentioned above have shown the effectiveness of ILIB, in both animal models and human studies. In addition, it also showed similar effects independent of the route used, invasive ILIB, or non-invasive VPBM. In the majority of studies, ILIB improved the hemodynamic parameters measured. Despite the promising and beneficial effects of ILIB in the various lung diseases summarized here, we must highlight the limitations in our review, including the problem of the language of the majority of articles, and the lack of detailed information regarding the dosimetry parameters. The information about the exact parameters employed is essential to validate this approach and to enable a safe and effective therapy to be developed.
Photobiomodulation parameters have involved wavelengths mainly in the red or near infrared regions, and the therapeutic effect is largely determined by the energy density. A biphasic dose response has been demonstrated, meaning that there are optimal irradiation and dose parameters, although these are likely to vary according to the pathology, whether light is delivered on the mucosal surface or the skin, and individual patient-associated factors [28]. Thus, for PBM treatment to be effective, the irradiation parameters need to be within the optimal dose window and this is a prerequisite for successful treatment.
Besides the effects of ILIB shown in this review, a variety of other metabolic, analgesic, anti-inflammatory, and immunomodulatory effects could be involved, thereby providing many opportunities for further study. Many lung diseases arise from disturbances in immune responses in individual patients, with intense release of pro-inflammatory cytokines (cytokine storm) that can damage the structure of organs such as the lungs. In this context, COVID-19 is an important viral disease, and researchers from all over the world have been looking for ways to fight this pandemic. Light-based therapies could be an interesting approach in combination with more traditional treatments.
The relevance of this review lies in compiling studies on an important topic, because the current literature is lacking and somewhat inaccessibile. In addition, it shows that more studies are needed, including randomized controlled trials, in order to support the use of this therapy in the clinic with safety using well-documented parameters.
Conclusion
In conclusion, this short review has shown the potential benefits, limitations, and relevance of ILIB in the treatment of lung diseases. All studies included have shown satisfactory effects of ILIB in both animal or human studies, with respect to the reduction in the inflammatory cascade, improved antioxidant effects, improvement of hemodynamic parameters, higher efficiency of gas exchange, and reduction of hospitalization periods. The studies included did not show any disadvantages or contraindications. Further studies are needed in order to better understand the dosimetry, and whether non-invasive VPBM can perform as well as invasive ILIB. The literature is currently lacking in randomized, controlled trials; therefore, this review highlights the importance of additional studies on this topic.
References
Boas DA, Pitris C, Ramanujam N (Eds.) (2011) Handbook of biomedical optics (1st ed.). CRC Press
Gasparyan L (2003) Laser irradiation of the blood. Laser Partner – Clinixperience 1–4
Hamblin MR (2018) Mechanisms and mitochondrial redox signaling in photobiomodulation. Photochem Photobiol 94(2):199–212
Dompe C, Moncrieff L, Matys J, Grzech-Leśniak K, Kocherova I, Bryja A, Bruska M, Dominiak M, Mozdziak P, Skiba THI, Shibli JA, AngelovaVolponi A, Kempisty B, Dyszkiewicz-Konwińska M (2020) Photobiomodulation-underlying mechanism and clinical applications. J Clin Med 9(6):1724
Tomé RFF, Silva DFB, dos Santos CAO et al (2020) ILIB (intravascular laser irradiation of blood) as an adjuvant therapy in the treatment of patients with chronic systemic diseases—an integrative literature review. Lasers Med Sci 35:1899–1907
Huang Ying-Ying, Aaron C-H Chen, Hamblin MR (2016) Low level laser and light therapy. Handb Biomed Optics 771–814
Fernandes KPS, Ferrari RM, Bussadori SK, Franca CM (2021) Vascular Photobiomodulation. Photobiomodul Photomed Laser Surg 39(3):143–144
Weber MH, Fußgänger-May TH, Wolf T (2007) The intravenous laser blood irradiation. Introduction of a new therapy. Ger J Acupunct Relat Tech 50:12–23
Tomé RFF, Silva DFB, Dos Santos CAO, de Vasconcelos NG, Rolim AKA, de Castro Gomes DQ (2020) ILIB (intravascular laser irradiation of blood) as an adjuvant therapy in the treatment of patients with chronic systemic diseases-an integrative literature review. Lasers Med Sci 35(9):1899–1907
Kirsanova AK, Novoderzhkina IS, Kozhura VL, Berezina TL, Dvoretskiĭ SV, Talantsev KV, Iakovleva NE (1994) Changes in the oxygen balance of the body in the acute period of hemorrhagic shock and after resuscitation under the effect of intravascular helium-neon laser irradiation of the blood. Anesteziol Reanimatol 5:33–35
Kashanskaia EP, Fedorov AA (2009) Low-intensity laser radiation in the combined treatment of patients with chronic obstructive bronchitis. Vopr Kurortol Fizioter Lech Fiz Kult 2:19–22
Burduli NM, Gabueva AA (2016) The influence of low-intensity laser radiation on the functional activity of neutrophils in the patients presenting with community-acquired pneumonia. Vopr Kurortol Fizioter Lech Fiz Kult 93(2):9–12
Atabai K, Matthay MA (2002) The pulmonary physician in critical care. 5: Acute lung injury and the acute respiratory distress syndrome: definitions and epidemiology. Thorax 57(5):452–8
Aït-Khaled N, Enarson DA (2006) Management of asthma: the essentials of good clinical practice [Educational Series: Asthma. Serialised guide. Management of asthma: the essentials of good clinical practice. Number 1 in the series]. Int J Tuberc Lung Dis 10(2):133–7
da Silva JGF, Dos Santos SS, de Almeida P, Marcos RL (2020) Lino-Dos-Santos-Franco A Effect of systemic photobiomodulation on the course of acute lung injury in rats. Lasers Med Sci 36(5):965–973
Chaves MEA, de Araújo AR, Piancastelli ACC, Pinotti M (2014) Effects of low-power light therapy on wound healing: LASER x LED. An Bras Dermatol 89(4):616–623
Alonso PT, Schapochnik A, Klein S, Brochetti R, Damazo AS (2022) de Souza Setubal Destro MF, Lino-Dos-Santos-Franco A Transcutaneous systemic photobiomodulation reduced lung inflammation in experimental model of asthma by altering the mast cell degranulation and interleukin 10 level. Lasers Med Sci 37(2):1101–1109
Prokopova LV, Losev AA (1992) Ursol IuI Effect of intravascular laser therapy on the rheological properties of blood in children with bilateral destructive pneumonia, Klin. Khir 6:7–9
Burduli NM (2006) Aksenova IZ The effects of intravenous laser irradiation of blood on the system hemodynamics of patients with chronic obstructive bronchitis exacerbation. Klin Med (MosK) 84(3):37–9
Sarycheva TG, Tsybzhitova EB, Popova OV, Aleksandrov OV (2009) Morphometry and electrophoretic mobility of red blood cells from patients with asthma in the intravenous blood laser irradiation. [Article in Russian] Klin Lab Diagn (3):13–4
Ivaniuta OM, Dziublik AIa, Skopichenko VN (1992) Optimal effectiveness of complex treatment of patients with chronic obstructive bronchitis by intravascular laser irradiation of blood. Clin Trial Probl Tuber (5–6):21–4. Article in Russian
Mikhaĭlov VA, Aleksandrova OIu, Gol’dina EM (1998) The immunomo-dulating action of low-energy laser radiation in the treatment of bronchial asthma (4):23–5.
Ananchenko VG, Khanin AG, Gostishcheva OV (1999) Cytological parameters of bronchoalveolar lavage in patients with chronic obstructive bronchitis exposed to laser radiation of blood. Ter Arkh 71(11):65–7
Farkhutdinov UR (2007) Intravascular laser blood irradiation in the treatment of patients with bronchial asthma. Ter Arkh 79(3):44–8
Hargreave FE, Nair P (2009) The definition and diagnosis of asthma. Clin Exp Allergy 39(11):1652–1658
Rusakova LI, Dobkin VG, Ovsyankina ES, Firsova VA, Bondarev GB, Sidorov VA (2001) Intravenous laser irradiation of blood in the complex treatment for acute and progressive tuberculosis in adolescentes. Proc SPIE 4422:102–105
Polyakov AA, Kornilova ZH, Demikhova OV (2017) The use of plasmapheresis and intravenous laser blood irradiation in treatment of patients with newly diagnosed tuberculosis at the late stages of hiv infection (references review). IP Pavlov Russ Med Biol Her 25(4):655–668
Huang YY, Sharma SK, Carroll J, Hamblin MR (2011) Biphasic dose response in low level light therapy an update. Dose Response 9:602–618
Funding
ALSF was supported by CNPq (302746/2020–0). MRH was supported by US NIH Grants R01AI050875 and R21AI121700.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. R. H. declares the following potential conflicts of interest. Scientific Advisory Boards: Transdermal Cap Inc, Cleveland, OH; Hologenix Inc. Santa Monica, CA; Vielight, Toronto, Canada; JOOVV Inc, Minneapolis-St. Paul MN; Sunlighten, Kansas City, MO; Consulting; USHIO Corp, Japan; Sanofi-Aventis Deutschland GmbH, Frankfurt am Main, Germany; Klox Asia, Guangzhou, China. Stockholding: Niraxx Light Therapeutics, Inc., Irvine CA; JelikaLite Corp, New York, NY. Other authors declare no cmpeting interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schapochnik, A., Alonso, P.T., de Souza, V. et al. Intravascular laser irradiation of blood (ILIB) used to treat lung diseases: a short critical review. Lasers Med Sci 38, 93 (2023). https://doi.org/10.1007/s10103-023-03750-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03750-0