Abstract
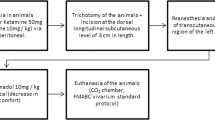
Low-power laser has been studied and applied as an auxiliary tool in wound healing. However, as it is a therapy with several variables to be controlled, there is great difficulty in establishing protocols and comparing its efficacy. Therefore, the objective of this study was to evaluate the effects of the use of low-power laser in fixed and crescent doses in the healing of skin wounds in rats. Seventy-five male Wistar rats were divided into three groups: G1 with animals that did not receive laser radiation; G2 with animals treated with fixed dose of 3 J/cm2 laser; G3 with animals treated with laser in increasing doses of 1 J/cm2, 3 J/cm2, 5 J/cm2. Macroscopic and histological analysis were performed. The lowest intensity of PMN was observed in the irradiated groups and G3 had lower intensity of this infiltrate compared to G1 and G2 (p <0.05). On the seventh day of injury, PMN infiltrate decreased in all groups, especially in G3 (p<0.05). It was observed that G2 had more blood vessels than G1 and G3 after 7 days of wound creation (p ˂ 0.05). Collagen quantification showed that laser-treated groups have increased collagen deposition. Different responses in the wound healing process were observed comparing G2 and G3 groups. The fluence of 1J/cm2 presented better results in the anti-inflammatory action than 3 J/cm2, although G3 presented the greatest amount of total collagen after ten days of treatment.





Similar content being viewed by others
References
Wilkinson HN, Hardman MJ Wound healing: cellular mechanisms and pathological outcomes. Open Biology 10:200223. https://doi.org/10.1098/rsob.200223
Gonzalez ACDO, Costa TF, Andrade ZDA, Medrado ARAP (2016) Wound healing - a literature review. An Bras Dermatol 91:614–620. https://doi.org/10.1590/abd1806-4841.20164741
Yang F, Bai X, Dai X, Li Y (2021) The biological processes during wound healing. Regen Med 16:373–390. https://doi.org/10.2217/rme-2020-0066
Karppinen S-M, Heljasvaara R, Gullberg D et al (2019) Toward understanding scarless skin wound healing and pathological scarring. F1000Res 8:F1000 Faculty Rev-787. https://doi.org/10.12688/f1000research.18293.1
Piva JADAC, Abreu EMDC, Silva VDS, Nicolau RA (2011) Ação da terapia com laser de baixa potência nas fases iniciais do reparo tecidual: princípios básicos. An Bras Dermatol 86:947–954. https://doi.org/10.1590/S0365-05962011000500013
Enwemeka CS, Parker JC, Dowdy DS et al (2004) The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg 22:323–329. https://doi.org/10.1089/pho.2004.22.323
de Lima FJC, de Oliveira Neto OB, Barbosa FT et al (2016) Is there a protocol in experimental skin wounds in rats using low-level diode laser therapy (LLDLT) combining or not red and infrared wavelengths? Systematic review. Lasers Med Sci 31:779–787. https://doi.org/10.1007/s10103-016-1893-z
Ribeiro MC, Correa VLR, Silva FKL da, et al (2020) Wound healing treatment using insulin within polymeric nanoparticles in the diabetes animal model. Eur J Pharm Sci 150:105330. https://doi.org/10.1016/j.ejps.2020.105330
Uzêda-E-Silva VD, Rodriguez TT, Rocha IAR et al (2016) Laser phototherapy improves early stage of cutaneous wound healing of rats under hyperlipidic diet. Lasers Med Sci 31:1363–1370. https://doi.org/10.1007/s10103-016-1985-9
Brassolatti P, Bossini PS, Oliveira MCD et al (2016) Comparative effects of two different doses of low-level laser therapy on wound healing third-degree burns in rats. Microsc Res Tech 79:313–320. https://doi.org/10.1002/jemt.22632
Andrade FDSDSD, Clark RMDO, Ferreira ML (2014) Effects of low-level laser therapy on wound healing. Rev Col Bras Cir 41:129–133. https://doi.org/10.1590/S0100-69912014000200010
Rochkind S, Rousso M, Nissan M et al (1989) Systemic effects of low-power laser irradiation on the peripheral and central nervous system, cutaneous wounds, and burns. Lasers Surg Med 9:174–182. https://doi.org/10.1002/lsm.1900090214
Rabelo SB, Villaverde AB, Nicolau RA et al (2006) Comparison between wound healing in induced diabetic and nondiabetic rats after low-level laser therapy. Photomed Laser Surg 24:474–479. https://doi.org/10.1089/pho.2006.24.474
Fiório FB, Albertini R, Leal-Junior ECP, de Carvalho PDTC (2014) Effect of low-level laser therapy on types I and III collagen and inflammatory cells in rats with induced third-degree burns. Lasers Med Sci 29:313–319. https://doi.org/10.1007/s10103-013-1341-2
Alhajj M, Goyal A (2022) Physiology, granulation tissue. In: In: StatPearls. StatPearls Publishing, Treasure Island (FL)
Kim SY, Nair MG (2019) Macrophages in wound healing: activation and plasticity. Immunology & Cell Biology 97:258–267. https://doi.org/10.1111/imcb.12236
Solmaz H, Dervisoglu S, Gulsoy M, Ulgen Y (2016) Laser biostimulation of wound healing: bioimpedance measurements support histology. Lasers Med Sci 31:1547–1554. https://doi.org/10.1007/s10103-016-2013-9
Colombo F, Neto ADAPV, Sousa APCD, Marchionni AMT, Pinheiro ALB, Reis SRDA (2013) Effect of low-level laser therapy (λ660 nm) on angiogenesis in wound healing: a immunohistochemical study in a rodent model. Braz Dent J 24:308–312. https://doi.org/10.1590/0103-6440201301867
Chittoria RK, Kumar SH (2021) Low-level laser therapy (LLLT) in wound healing. In: Shiffman MA, Low M (eds) Chronic wounds, wound dressings and wound healing. Springer International Publishing, Cham, pp 21–26
Silveira P, Silva L, Freitas T, Latini A (2011) Effects of low-power laser irradiation (LPLI) at different wavelengths and doses on oxidative stress and fibrogenesis parameters in an animal model of wound healing. Lasers in medical science 26:125–131. https://doi.org/10.1007/s10103-010-0839-0
Novaes RD, Gonçalves RV, Cupertino MC et al (2014) The energy density of laser light differentially modulates the skin morphological reorganization in a murine model of healing by secondary intention. Int J Exp Pathol 95:138–146. https://doi.org/10.1111/iep.12063
de Moraes JM, de Oliveira E, Mendonça D, Moura VBL et al (2013) Anti-inflammatory effect of low-intensity laser on the healing of third-degree burn wounds in rats. Lasers Med Sci 28:1169–1176. https://doi.org/10.1007/s10103-012-1213-1
Aparecida Da Silva A, Leal-Junior ECP, Alves ACA et al (2013) Wound-healing effects of low-level laser therapy in diabetic rats involve the modulation of MMP-2 and MMP-9 and the redistribution of collagen types I and III. J Cosmet Laser Ther. 15:210–216. https://doi.org/10.3109/14764172.2012.761345
Busnardo VL, Biondo-Simões MLP (2010) Os efeitos do laser hélio-neônio de baixa intensidade na cicatrização de lesões cutâneas induzidas em ratos. Rev bras fisioter 14:45–51. https://doi.org/10.1590/S1413-35552010000100008
Kilík R, Lakyová L, Sabo J et al (2014) Effect of equal daily doses achieved by different power densities of low-level laser therapy at 635 nm on open skin wound healing in normal and diabetic rats. BioMed Res. Int. 2014:e269253. https://doi.org/10.1155/2014/269253
Reis SRA, Medrado AP, Marchionni AMT et al (2008) Effect of 670-nm laser therapy and dexamethasone on tissue repair: a histological and ultrastructural study. Photomed Laser Surg 26:307–313. https://doi.org/10.1089/pho.2007.2151
Gál P, Vidinský B, Toporcer T et al (2006) Histological assessment of the effect of laser irradiation on skin wound healing in rats. Photomed Laser Surg 24:480–488. https://doi.org/10.1089/pho.2006.24.480
de Carvalho Abreu JA, da Luz Sousa A, Alves CLGF, Nunes JT (2011) Análise histológica da cicatrização de feridas cutâneas experimentais sob ação do laser de baixa potência. Sci med:96–100
Souza NHC, Ferrari RAM, Silva DFT et al (2014) Effect of low-level laser therapy on the modulation of the mitochondrial activity of macrophages. Braz J Phys Ther 18:308–314. https://doi.org/10.1590/bjpt-rbf.2014.0046
Fernandes KPS, Souza NHC, Mesquita-Ferrari RA et al (2015) Photobiomodulation with 660-nm and 780-nm laser on activated J774 macrophage-like cells: effect on M1 inflammatory markers. J. Photochem. Photobiol. B, Biol. 153:344–351. https://doi.org/10.1016/j.jphotobiol.2015.10.015
Acknowledgements
We would to thank Centro Multiusuário de Produção e Experimentaçao Animal (CMPEA) of the Instituto de Patologia Tropical e Saúde Pública (IPTSP) of the Universidade Federal de Goias (UFG) and Histotechnics and Innovation Laboratory (LHIn)/IPTSP/UFG by their for providing equipment and input materials.
Funding
The author Leiny Paula de Oliveira received personal financial support from her master’s degree scholarship sponsored by Higher Education Personnel Improvement Coordination (CAPES), a foundation linked to the Ministry of Education of Brazil.
Author information
Authors and Affiliations
Contributions
Leiny Paula de Oliveira: bibliographic review, animals’ management, performing the procedure of animals, treatment of animals, production of photographic material (macroscopic and microscopic), assistance in histological procedures (cleavage and microtomy), writing of the work, textual formatting. Angelica de Lima Chagas: animals’ management, treatment of animals, assistance in the production of photographic material (macroscopic) and assistance in writing. Tainara Ribeiro de Souza: animals’ management; assistance in writing, text formatting, translation and final review. Isabela Rodrigues Araújo: animals’ management, treatment of animals, assistance in the production of photographic material (macroscopic) and assistance in writing. Liliana Borges de Menezes: orientation, writing of the work, scientific supervision, spelling, textual and grammatical correction, translation and final review. Marina Pacheco Miguel: orientation, writing of the work, scientific supervision, spelling, textual and grammatical correction, translation and final review. Valcinir Aloisio Scalla Vulcani: orientation, writing of the work, scientific supervision, spelling, textual and grammatical correction, translation and final review.
Corresponding author
Ethics declarations
Conflict of interest
The authors no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Oliveira, L.P., de Lima Chagas, A., de Souza, T.R. et al. Low-power laser in increasing doses improve wound healing process in rats. Lasers Med Sci 38, 60 (2023). https://doi.org/10.1007/s10103-023-03716-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03716-2