Abstract
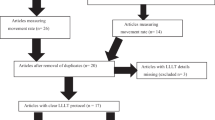
To determine whether the application of photobiomodulation (PBM), as an adjunctive treatment for patients with orthodontic fixed appliances, decreased the total treatment time compared to conventional orthodontics. Studies were collected from four electronic databases following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for systematic reviews. Eligibility criteria were full-text articles in English or Spanish with the design of randomized (RCT), non-randomized clinical trials (non-RCT), and retrospective cohort, without any restriction regarding the publication time, in which the effect of PBM using low-level laser irradiation (LLLI) and light-emitting diode (LED) for the acceleration of the orthodontic movement had been evaluated. Data collection and analysis: Two authors independently extracted data for the characteristics and outcomes of the studies selected for inclusion. The risk of bias (RoB 2 and Robins-I) and the quality assessments (GRADE) were performed. For the quantitative synthesis, the standardized mean difference was calculated for each individual study selected and then the data were combined using a random-effects meta-analysis. The total number of included studies was n = 22 (only RCT and non-RCT were found) with a total of 515 participants. The included studies exhibited high risk of bias and some concerns, though none of them presented a low risk of bias. The quality of the studies was very low. The meta-analysis showed that the means (mm) and 95% confidence intervals (95% CI) of acceleration of tooth movement at 1, 2, and 3 months were 0.50 (− 0.28, 1.28), 1.40 (0.27, 2.53), and 0.46 (− 0.33, 1.24), respectively. The analysis showed that there is no evidence to support the use of LLLI to accelerate the orthodontic movement. LED for the acceleration of orthodontic movement does not have sufficient evidence to generate conclusions about it.



Similar content being viewed by others
References
Cruz DR, Kohara EK, Ribeiro MS, Wetter NU (2004) Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: a preliminary study. Lasers Surg Med 35:117–120. https://doi.org/10.1002/lsm.20076
Mota-Rodriguez AN, Olmedo-Hernandez O, Argueta-Figueroa L (2019) A systematic analysis of evidence for surgically accelerated orthodontics. J Clin Exp Dent 11:e829–e838. https://doi.org/10.4317/jced.56048
AlSayed Hasan MMA, Sultan K, Hamadah O (2017) Low-level laser therapy effectiveness in accelerating orthodontic tooth movement: a randomized controlled clinical trial. Angle Orthod 87:499–504. https://doi.org/10.2319/062716-503.1
Fernandes MRU, Suzuki SS, Suzuki H, Martinez EF, Garcez AS (2019) Photobiomodulation increases intrusion tooth movement and modulates IL-6, IL-8 and IL-1β expression during orthodontically bone remodeling. J Biophotonics 12:e201800311. https://doi.org/10.1002/jbio.201800311
Borzabadi-Farahani A (2016) Effect of low-level laser irradiation on proliferation of human dental mesenchymal stem cells; a systemic review. J Photochem Photobiol B 162:577–582. https://doi.org/10.1016/j.jphotobiol.2016.07.022
Mohamad SA, Milward MR, Hadis MA, Kuehne SA, Cooper PR (2021) Photobiomodulation of mineralisation in mesenchymal stem cells. Photochem Photobiol Sci 20:699–714. https://doi.org/10.1007/s43630-021-00047-5
Sleep SL, Skelly D, Love RM, George R (2021) Bioenergetics of photobiomodulated osteoblast mitochondrial cells derived from human pulp stem cells: systematic review. Lasers Med Sci. https://doi.org/10.1007/s10103-021-03439-2
Shaughnessy T, Kantarci A, Kau CH, Skrenes D, Skrenes S, Ma D (2016) Intraoral photobiomodulation-induced orthodontic tooth alignment: a preliminary study. BMC Oral Health 16:3. https://doi.org/10.1186/s12903-015-0159-7
Batinjan G, Filipović Zore I, Rupić I, Bago Jurič I, Zore Z, Gabrić Pandurić D (2013) Assessing health-related quality of life with antimicrobial photodynamic therapy (APDT) and low level laser therapy (LLLT) after third molar removal. J Lasers Med Sci 4:120–126
Alfawal AMH, Hajeer MY, Ajaj MA, Hamadah O, Brad B, Latifeh Y (2020) Evaluation of patient-centered outcomes associated with the acceleration of canine retraction by using minimally invasive surgical procedures: a randomized clinical controlled trial. Dent Med Probl 57:285–293. https://doi.org/10.17219/dmp/120181
Khullar SM, Brodin P, Barkvoll P, Haanaes HR (1996) Preliminary study of low-level laser for treatment of long-standing sensory aberrations in the inferior alveolar nerve. J Oral Maxillofac Surg 54:2–7. https://doi.org/10.1016/s0278-2391(96)90290-6 (discussion 7-8)
De La Torre F, Alfaro C (2016) Parestesia postquirúrgica: terapia con láser de baja potencia. Reporte de 2 casos. Revista Estomatológica Herediana 26:92–101
Eslamian L, Borzabadi-Farahani A, Hassanzadeh-Azhiri A, Badiee MR, Fekrazad R (2014) The effect of 810-nm low-level laser therapy on pain caused by orthodontic elastomeric separators. Lasers Med Sci 29:559–564. https://doi.org/10.1007/s10103-012-1258-1
Borzabadi-Farahani A, Cronshaw M (2017) Lasers in Orthodontics. In: Coluzzi D, Parker S (eds) Lasers in Dentistry—Current Concepts. Textbooks in Contemporary Dentistry. Springer, Cham, p 247–271
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 372:n160. https://doi.org/10.1136/bmj.n160
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (2019) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, p 1–694
Üretürk SE, Saraç M, Fıratlı S, Can ŞB, Güven Y, Fıratlı E (2017) The effect of low-level laser therapy on tooth movement during canine distalization. Lasers Med Sci 32:757–764. https://doi.org/10.1007/s10103-017-2159-0
Samara SA, Nahas AZ, Rastegar-Lari TA (2018) Velocity of orthodontic active space closure with and without photobiomodulation therapy: a single-center, cluster randomized clinical trial. Lasers Dent Sci 2:109–118. https://doi.org/10.1007/s41547-018-0026-3
Kau CH, Kantarci A, Shaughnessy T, Vachiramon A, Santiwong P, de la Fuente A et al (2013) Photobiomodulation accelerates orthodontic alignment in the early phase of treatment. Prog Orthod 14:30. https://doi.org/10.1186/2196-1042-14-30
Caccianiga G, Crestale C, Cozzani M, Piras A, Mutinelli S, Lo Giudice A et al (2016) Low-level laser therapy and invisible removal aligners. J Biol Regul Homeost Agents 30:107–113
Sousa MV, Scanavini MA, Sannomiya EK, Velasco LG, Angelieri F (2011) Influence of low-level laser on the speed of orthodontic movement. Photomed Laser Surg 29:191–196. https://doi.org/10.1089/pho.2009.2652
Limpanichkul W, Godfrey K, Srisuk N, Rattanayatikul C (2006) Effects of low-level laser therapy on the rate of orthodontic tooth movement. Orthod Craniofac Res 9:38–43. https://doi.org/10.1111/j.1601-6343.2006.00338.x
Yassaei S, Aghili H, Afshari JT, Bagherpour A, Eslami F (2016) Effects of diode laser (980 nm) on orthodontic tooth movement and interleukin 6 levels in gingival crevicular fluid in female subjects. Lasers Med Sci 31:1751–1759. https://doi.org/10.1007/s10103-016-2045-1
Ekizer A, Türker G, Uysal T, Güray E, Taşdemir Z (2016) Light emitting diode mediated photobiomodulation therapy improves orthodontic tooth movement and miniscrew stability: a randomized controlled clinical trial. Lasers Surg Med 48:936–943. https://doi.org/10.1002/lsm.22516
Doshi-Mehta G, Bhad-Patil WA (2012) Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop 141:289–297. https://doi.org/10.1016/j.ajodo.2011.09.009
Qamruddin I, Alam MK, Mahroof V, Fida M, Khamis MF, Husein A (2017) Effects of low-level laser irradiation on the rate of orthodontic tooth movement and associated pain with self-ligating brackets. Am J Orthod Dentofacial Orthop 152:622–630. https://doi.org/10.1016/j.ajodo.2017.03.023
Varella AM, Revankar AV, Patil AK (2018) Low-level laser therapy increases interleukin-1β in gingival crevicular fluid and enhances the rate of orthodontic tooth movement. Am J Orthod Dentofacial Orthop 154:535-544.e535. https://doi.org/10.1016/j.ajodo.2018.01.012
Kansal A, Kittur N, Kumbhojkar V, Keluskar KM, Dahiya P (2014) Effects of low-intensity laser therapy on the rate of orthodontic tooth movement: a clinical trial. Dent Res J (Isfahan) 11:481–488
Abdelhameed AN, Refai WMM (2018) Evaluation of the effect of combined low energy laser application and micro-osteoperforations versus the effect of application of each technique separately on the rate of orthodontic tooth movement. Open Access Maced J Med Sci 6:2180–2185. https://doi.org/10.3889/oamjms.2018.386
Isola G, Matarese M, Briguglio F, Grassia V, Picciolo G, Fiorillo L, et al (2019) Effectiveness of low-level laser therapy during tooth movement: a randomized clinical trial. Materials (Basel Switzerland) 12:2187 https://doi.org/10.3390/ma12132187
Dalaie K, Hamedi R, Kharazifard MJ, Mahdian M, Bayat M (2015) Effect of low-level laser therapy on orthodontic tooth movement: a clinical investigation. J Dent (Tehran) 12:249–256
Genc G, Kocadereli I, Tasar F, Kilinc K, El S, Sarkarati B (2013) Effect of low-level laser therapy (LLLT) on orthodontic tooth movement. Lasers Med Sci 28:41–47. https://doi.org/10.1007/s10103-012-1059-6
Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M (2008) The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci 23:27–33. https://doi.org/10.1007/s10103-007-0449-7
Domínguez A, Gómez C, Palma JC (2015) Effects of low-level laser therapy on orthodontics: rate of tooth movement, pain, and release of RANKL and OPG in GCF. Lasers Med Sci 30:915–923. https://doi.org/10.1007/s10103-013-1508-x
Nimeri G, Kau CH, Abou-Kheir NS, Corona R (2013) Acceleration of tooth movement during orthodontic treatment–a frontier in orthodontics. Prog Orthod 14:42. https://doi.org/10.1186/2196-1042-14-42
Wakabayashi H, Hamba M, Matsumoto K, Tachibana H (1993) Effect of irradiation by semiconductor laser on responses evoked in trigeminal caudal neurons by tooth pulp stimulation. Lasers Surg Med 13:605–610. https://doi.org/10.1002/lsm.1900130603
Bjordal JM, Lopes-Martins RA, Iversen VV (2006) A randomised, placebo controlled trial of low level laser therapy for activated Achilles tendinitis with microdialysis measurement of peritendinous prostaglandin E2 concentrations. Br J Sports Med 40:76–80. https://doi.org/10.1136/bjsm.2005.020842 (discussion 76-80)
Deana NF, Zaror C, Sandoval P, Alves N (2017) Effectiveness of low-level laser therapy in reducing orthodontic pain: a systematic review and meta-analysis. Pain Res Manag 2017:8560652. https://doi.org/10.1155/2017/8560652
Smith KC (1991) The photobiological basis of low level laser radiation therapy. Laser Therapy 3:19–24
España-Tost AJ, Arnabat-Domínguez J, Berini-Aytés L, Gay-Escoda C (2004) Aplicaciones del láser en Odontología. RCOE 9:497–511
Bjordal JM, Couppé C, Chow RT, Tunér J, Ljunggren EA (2003) A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother 49:107–116. https://doi.org/10.1016/s0004-9514(14)60127-6
Szewczyk J, Koszowski R, Juźwiak R, Smieszek-Wilczewska J (2013) A radiographic assessment of the regeneration process in post-operative alveolar bone defects in patients with different IL-1B-511 genotypes. Adv Clin Exp Med 22:847–854
Flores-Mejia LA, Cabrera-Rivera GL, Ferat-Osorio E, Mancilla-Herrera I, Torres-Rosas R, Bosco-Garate IB et al (2019) Function is dissociated from activation-related immunophenotype on phagocytes from patients with SIRS/sepsis syndrome. Shock 52:e68–e75. https://doi.org/10.1097/SHK.0000000000001314
Tanaka T, Narazaki M, Kishimoto T (2014) IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol 6:a016295. https://doi.org/10.1101/cshperspect.a016295
Michelogiannakis D, Al-Shammery D, Akram Z, Rossouw PE, Javed F, Romanos GE (2019) Influence of low-level laser therapy on orthodontically-induced inflammatory root resorption. A systematic review. Arch Oral Biol 100:1–13. https://doi.org/10.1016/j.archoralbio.2019.01.017
Ge MK, He WL, Chen J, Wen C, Yin X, Hu ZA et al (2015) Efficacy of low-level laser therapy for accelerating tooth movement during orthodontic treatment: a systematic review and meta-analysis. Lasers Med Sci 30:1609–1618. https://doi.org/10.1007/s10103-014-1538-z
Sonesson M, De Geer E, Subraian J, Petrén S (2016) Efficacy of low-level laser therapy in accelerating tooth movement, preventing relapse and managing acute pain during orthodontic treatment in humans: a systematic review. BMC Oral Health 17:11. https://doi.org/10.1186/s12903-016-0242-8
Cronshaw M, Parker S, Anagnostaki E, Lynch E (2019) Systematic review of orthodontic treatment management with photobiomodulation therapy. Photobiomodul Photomed Laser Surg 37:862–868. https://doi.org/10.1089/photob.2019.4702
AlShahrani I, Togoo RA, Hosmani J, Alhaizaey A (2019) Photobiomodulation in acceleration of orthodontic tooth movement: a systematic review and meta analysis. Complement Ther Med 47:102220. https://doi.org/10.1016/j.ctim.2019.102220
Bakdach WMM, Hadad R (2020) Effectiveness of low-level laser therapy in accelerating the orthodontic tooth movement: a systematic review and meta-analysis. Dent Med Probl 57:73–94. https://doi.org/10.17219/dmp/112446
Pandis N (2012) Sample calculation for split-mouth designs. Am J Orthod Dentofac Orthop 141:818–819
O’Brien SF, Yi QL (2016) How do I interpret a confidence interval? Transfusion 56:1680–1683. https://doi.org/10.1111/trf.13635
Sánchez-Meca J, Marín-Martínez F (2008) Confidence intervals for the overall effect size in random-effects meta-analysis. Psychol Methods 13:31
Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P. Chapter 15: Interpreting results and drawing conclusions. 2020. Cochrane Handbook for Systematic Reviews of Interventions Version 61
Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557. https://doi.org/10.1136/bmj.327.7414.557
Acknowledgements
LAF thank “Investigadoras e investigadores por México” CONACYT program and the Posgrado de la Facultad de Odontología, Universidad Autónoma Benito Juárez de Oaxaca, for their support. LAF and RTR thank “Cuerpo Académico Investigación en Salud UABJO-CA63.”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Olmedo-Hernández, O.L., Mota-Rodríguez, A.N., Torres-Rosas, R. et al. Effect of the photobiomodulation for acceleration of the orthodontic tooth movement: a systematic review and meta-analysis. Lasers Med Sci 37, 2323–2341 (2022). https://doi.org/10.1007/s10103-022-03538-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-022-03538-8