Abstract
Introduction
The present study aimed to explore the suitability of the vocabulary knowledge (VOC) test as an accurate and reliable proxy of cognitive reserve (CR) by evaluating its psychometric properties and discrimination accuracy compared with other CR measures in multiple sclerosis (MS).
Methods
Sixty-eight consecutive people with multiple sclerosis (pwMS), followed at our MS outpatient clinic, completed a clinical evaluation and neuropsychological assessment including: VOC, Brief Repeatable Battery of Neuropsychological Tests (BRB-N), Cognitive Reserve Index Questionnaire (CRIq), Beck Depression Inventory-II, and State-Trait Anxiety Inventory. Reliability, convergent and divergent validity, and discrimination accuracy of the VOC were assessed using educational level as reference standard. The possible effects of sociodemographic and clinical factors on VOC and their role in predicting global cognitive status were also explored.
Results
VOC demonstrated good internal consistency (Cronbach’s α = 0.894) and adequate construct validity. It showed an acceptable level of discrimination between pwMS with high and low CR, comparable to the CRIq score. Education strongly affected VOC scores, which in turn were independent of MS features. VOC emerged as an independent predictor of global cognitive status together with MS-related disability.
Conclusion
We demonstrated the validity of VOC as a reliable CR measure in pwMS. Thus, CR may also be estimated using fixed objective measures, independent of brain pathology and clinical features. Early CR estimation may help clinicians identify pwMS at a higher risk of cognitive decline and plan strict neuropsychological monitoring and cognitive interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cognitive changes in multiple sclerosis (MS) are estimated to affect 40-70% of patients because of chronic and multifocal MS-related central nervous system (CNS) damage [1]. Cognitive impairment is one of the most disabling manifestations in people with MS (pwMS), with detrimental consequences for individuals’ quality of life, performance, and achievements at study/work and in everyday activities [2]. However, extreme variability has been observed in MS-related cognitive deficits, with pwMS being able to withstand a considerable disease burden. This cognitive-neuropathologic dissociation is not exclusive to MS; indeed, it has also been described in Alzheimer’s disease (AD) [3] and other neurological conditions [3, 4]. This mismatch has prompted the elaboration of the concept of a structural and functional brain reserve that may explain individual differences in the delay in time between pathology and clinical expression of cognitive decline [5, 6].
The brain's capacity to cope with age-related brain changes and pathologic damage has been defined as cognitive reserve (CR), which recruits protective/compensatory mechanisms associated with cognitive abilities built up over the course of life [3, 4]. Numerous operationalizations of the latent concept of CR have attempted to quantify the level of reserve by proposing educational or occupational attainment, together with engagement in leisure and social activities, as the most influential proxy of CR [3, 7]. However, in clinical practice, CR evaluation is commonly limited to the highest attained educational level; this view presents some limitations because the educational level is strongly influenced by socioeconomic and cultural factors [5, 8] in terms of possibilities and resources needed to afford higher educational attainment and subsequent leading occupational position as well as an enriching environment [9], which results in being too simplistic to capture the dynamic and multidimensional nature of CR across life [10].
Multi-item surveys, including the assessment of socio-behavioral factors at different life stages, have been developed to overcome these limitations [11,12,13]; however, most of these do not consider crucial CR contributors, such as educational attainment and occupational history. Of these, the Cognitive Reserve Index Questionnaire (CRIq) has proven to be an efficient and reliable tool for measuring CR by integrating information related to educational level and occupational status with items assessing activities carried out throughout adulthood and current lifestyle (e.g., time spent performing cognitively, socially, and/or physically stimulating leisure activities or hobbies) [14].
Within this framework, lifetime intellectual enrichment represents a crucial source of CR and may be estimated by objective measures such as vocabulary knowledge (VOC), a test validated and standardized in several languages as a subtest of the Wechsler Adult Intelligence Scale (WAIS), which evaluates semantic knowledge acquired through enriching life activities, such as educational attainment, occupation, and frequent reading [15, 16]. Some studies revealed that higher CR assessed by the VOC was associated with better performance on cognitive tests in MS, independent of brain pathology and clinical features [17, 18], moderating the impact of lesion load on cognition in MS [19, 20]. However, to the best of our knowledge, no study has assessed the reliability and discrimination accuracy of this tool as a proxy for CR in pwMS. Therefore, the present study aimed to (i) examine the validity and reliability of the VOC as a suitable proxy of the CR and (ii) evaluate its discrimination accuracy compared to other CR measures, such as educational level and CRIq scale, in an Italian cohort of pwMS.
Materials and methods
Participants
Consecutive pwMS followed at the MS outpatient clinic of the Division of Neurology of the University of Campania “Luigi Vanvitelli,” in Naples (Italy) were screened and enrolled in the study. Participants were included in the study if they met the following inclusion criteria: (i) a diagnosis of MS according to the revised McDonald criteria [21], (ii) absence of psychiatric comorbidities and major neurocognitive disorders according to DSM-5, and (iii) absence of clinical relapse and use of corticosteroids or other drugs affecting cognitive functions within 3 months of the evaluation.
Demographic (i.e., age, sex, and years of schooling) and clinical aspects, such as disease duration and the Expanded Disability Status Scale (EDSS), were recorded by a neurologist with expertise in MS.
All participants signed an informed consent form to participate in the study, which was approved by the Local Ethics Committee and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Neuropsychological assessment
The participants completed the VOC of the WAIS. This test evaluates vocabulary knowledge by asking examinees to explain the meaning of 35 words. VOC is considered an estimate of lifetime intellectual enrichment because it is strongly influenced by enriching life activities (e.g., education, occupation, and reading) [3]. Raw VOC scores were used for the analyses.
All participants underwent the Italian version of Rao’s Brief Repeatable Battery of Neuropsychological Tests (BRB-N) [22]. The BRB-N comprises seven cognitive tests, administered in a fixed order, to assess verbal memory (Selective Reminding Test; SRT), visuospatial memory (10/36 Spatial Recall Test; SPART), attention, working memory, speed of information processing (Paced Auditory Serial Addition Test 3- and 2-s interval versions and Symbol Digit Modality Test; PASAT-3″, PASAT-2″, and SDMT), and semantic verbal fluency (Word List Generation; WLG). In addition, the interference subtask of the Stroop Color Word Interference Test was employed to evaluate inhibitory control [22]. Z-scores were calculated for each sub-score and the overall cognition score was computed by summing all z-scores.
To assess convergent validity, participants completed the CRIq, a multi-item interview widely used in pwMS [23, 24], designed to evaluate CR by combining three different sources: educational attainment, working activity, and engagement in leisure time activities [14]. It comprises three different subscores: The CRI-Education subscore counts the years of formal education plus training and professional courses with a duration of at least six months; the CRI-Working Activity reflects the number of working years based on the cognitive load of the occupation, defined considering intellectual involvement and responsibility; and finally, the CRI-Leisure Time considers all intellectual, social, and leisure activities (e.g., reading books, practicing sports, volunteering, travelling, caring for children/pets) practiced during adulthood. The CRIq total score is the average of the three subscores (standardized and transposed to a scale with mean = 100 and SD = 15), with higher CRIq scores reflecting higher estimated CR.
Finally, the Beck Depression Inventory-II (BDI-II) and State-Trait Anxiety Inventory (STAI-Y), validated in pwMS [25, 26], were employed to assess depressive and anxiety symptoms, respectively. Scores ≥ 19 on the BDI-II indicated the presence of clinically relevant depressive symptoms [25], whereas scores ≥ 64 on the STAI-Y indicated the presence of significant anxiety symptoms [26].
Statistical analysis
Data quality of data was defined as appropriate in the absence of missing values and by low percentages of floor and ceiling effects, following previous validation studies [27, 28]. Univariate normality was assessed by checking skewness and kurtosis values for the variables of interest; values not exceeding |2| are typically considered indicative of a normal distribution [29,30,31]. Descriptive variables are then reported accordingly with non-normal variables reported as median and interquartile range and normal variables as mean and standard deviation (SD).
Internal consistency was tested using Cronbach’s α coefficient with values ≥ 0.70 considered indicative of acceptable internal consistency [32]. We obtained additional evidence on the reliability and scaling assumptions for each item using Pearson’s item-total correlations and corrected item-total correlations to adjust for inflation errors [27]. Cohen’s conventions (weak, r < 0.30; moderate, r = 0.30–0.50; strong, r > 0.50) were used to interpret the effect sizes.
Convergent validity was assessed by correlations between the VOC and CRIq total scores, whereas divergent validity was evaluated by correlations with the total scores of the BDI-II and STAI-Y. The potential effects of demographic (i.e., age, sex, and educational level) and clinical factors (i.e., EDSS and disease duration) on the VOC score were evaluated using multiple regression analysis.
Receiver operating characteristics (ROC) analysis using education level as the gold standard (years of schooling ≥ 16) was performed to test the accuracy of VOC compared to CRIq in classifying individuals with low and high CR. Intrinsic properties, sensitivity (Se) and specificity (Sp), were determined at the optimal cutoff identified using Youden’s J statistic [33].
Multiple regression analysis was carried out to explore the possible effect of VOC on cognition by entering the overall BRB-N composite score as a dependent variable and age, years of schooling, sex, EDSS, disease duration, and vocabulary as predictors controlling for multicollinearity by checking tolerance and variance inflation factor (VIF).
Statistical analyses were performed using IBM SPSS Statistics version 29.
Results
Sixty-eight (62% males) pwMS were enrolled with a mean age of 41.66 (SD = 13.17) years and an average education of 14.07 (SD = 3.58). Fifty-two (76.5%) pwMS were relapsing–remitting MS (RRMS), three (4.4%) had primary progressive MS (PPMS), and 5 (7.3%) were secondary progressive (SPMS), with a mean EDSS score of 2.60 (SD = 1.77) and an average disease duration of 10.20 years (SD = 9.42) (Table 1). The mean VOC score was 45.32 (SD = 12.51).
Reliability
The VOC demonstrated acceptable internal consistency, as indicated by Cronbach’s α of 0.894. Most of the items showed an acceptable level of discrimination (items 2, 5, 7, 8, 10–13, 15, 18–20, 22–24, and 26–35; corrected item-total correlations range = 0.319–0.641). Although some items (1, 3, 4, 6, 9, 14, 16, 17, 21, and 25; corrected item-total correlations range = − 0.017 to 0.288) demonstrated an unsatisfactory level of discrimination (Table 2), these were retained for subsequent analyses to maintain the original structure of the scale.
Convergent and divergent validity
VOC correlated with CRIq-Education (r = 0.493, p < 0.001), CRIq-Working Activity (r = 0.365, p = 0.003), CRIq-Leisure time (rs = 0.421, p < 0.001), and CRIq-total (r = 0.516, p < 0.001) scores. Conversely, divergent validity was confirmed by the absence of correlations between the VOC and BDI-II (rs = − 0.034, p = 0.811) and STAI-Y (r = 0.110, p = 0.381).
Effect of demographic and clinical variables
Multiple regression analysis revealed that a higher level of education was related to better performance on the VOC (β = 0.585, t = 4.866, p < 0.001), whereas no associations emerged with age, sex, EDSS score, and disease duration (Table 3).
Level of discrimination
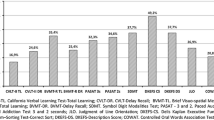
ROC analysis using educational level (years of schooling ≥ 16) as gold standard indicated that VOC demonstrated, at an optimal cutoff of 44.50 (J = 0.514), an acceptable level of discrimination of pwMS with high and low CR (AUC = 0.775; p < 0.001; SE = 0.059; 95% CI 0.659–0.891) with acceptable intrinsic properties (Se = 0.880; Sp = 0.634) and comparable to the CRIq score (AUC = 0.788; p < 0.001; SE = 0.057; 95% CI 0.677–0.899; Se = 0.560; Sp = 0.878) (Fig. 1). Based on the abovementioned cutoff of VOC (< 44, low CR; ≥ 45, high CR), 30 pwMS were classified as having low CR (44.1%) and 38 as having high CR (55.9%).
Predictors of overall cognition
Multiple regression analysis revealed that higher cognition scores were associated with lower EDSS (β = − 0.394, t = − 3.008, p = 0.004) and higher VOC scores (β = 0.339, t = 2.341, p = 0.023). The associations between the overall cognition score and age, sex, education, and disease duration were not significant (Table 4).
Discussion
The present study aimed to test the feasibility of VOC as a reliable measure of CR in MS. The VOC demonstrated acceptable internal consistency and adequate convergent and divergent validity, as indicated by a significant strong association with the CRIq scale but not with measures assessing depression and anxiety. In addition, this tool showed an acceptable level of discrimination of pwMS with high and low CR and comparable to the CRIq score using educational attainment as reference standard. VOC was associated with educational level but unrelated to age, sex, and clinical features, whereas it emerged as a crucial predictor of cognition, together with EDSS, when controlling for the effect of education and other clinical variables.
Although vocabulary knowledge is frequently used to estimate premorbid intelligence, considering its stability when facing neurologic insult and pathological cognitive decline [34, 35], it may also represent a proxy of CR [36]. Analyzing the capacity of VOC in discriminating between pwMS with high and low CR by ROC analysis, we found that VOC revealed an acceptable level of discrimination accuracy and good intrinsic properties, comparable to those of CRIq, a multi-item interview specifically designed to estimate CR. Indeed, CRIq was demonstrated to be a suitable tool for CR evaluation by combining the most frequently used proxies of CR, such as educational and occupational attainments and leisure activities carried out during an entire adult lifetime [14]. Therefore, the relationship with the CRIq global score, stronger than those with CRIq subscores, proves the convergent validity of the VOC and suggests that it adequately covers the entire spectrum of CR dimensions. Taken together, our findings indirectly confirm that CR relies on static measures, such as years of education and occupational attainment, as well as dynamic proxies, such as literacy and engaging in cognitively stimulating activities, likely to be modified over time [37]. Hence, our work provides further evidence that several factors contribute to the relationship between CR and cognition in clinical and non-clinical populations [38].
Moreover, VOC was not linked to scales assessing neuropsychiatric symptoms such as depression and anxiety. The protective effect of CR in MS is not confined to cognition but may also extend to neuropsychiatric symptoms [24, 39]; however, depression may also impact individuals’ participation in leisure and social activities and moderate the relationship between CR and cognition [40]. Similarly, we found that VOC scores were independent of demographic factors, except for educational level, and MS-related clinical features, such as the level of disability and disease duration. Taken together, these results support the idea that greater lifetime intellectual enrichment is independent of age-related processes and MS-related CNS pathology, thus suggesting that VOC might represent a reliable and standardized proxy of CR in pwMS, since it provides a reliable measure in the presence of neuropsychiatric disturbances.
Furthermore, VOC emerged as a predictor of cognitive status after controlling for educational level, with better performance on BRB-N related to higher VOC and lower EDSS scores. These results not only further confirm findings from previous studies revealing a link between disability and performance on neuropsychological tests in MS [41, 42] but also provide evidence of VOC as a more ecological measure of CR than education in MS. Considering that the MS course and prognosis remain unpredictable, here we propose a cutoff of VOC (44.50) that may help researchers and clinicians to identify pwMS with high and low CR. In fact, reliable CR estimation at the time of diagnosis seems to be a useful clinical predictor of future cognitive decline, driving the identification of patients who might benefit from stricter neuropsychological monitoring and early cognitive interventions [43].
Nevertheless, this study has some limitations. First, the small sample size may limit the generalizability of the results. Second, the cross-sectional nature of the study did not prove the stability of VOC over time; future longitudinal studies should provide evidence of sensitivity to change. Moreover, despite some items demonstrated an unsatisfactory level of discrimination, we decided to retain the original version of the scale. This can be explained by the fact that vocabulary is learned by repeated exposure to words in order to achieve long-term memory retention [44], and thus, the presence of obsolete words may affect individuals’ performance. To this end, a constant update of VOC tests is required to avoid including disused words, thus guaranteeing more reliable estimates of vocabulary knowledge.
In conclusion, we demonstrated the reliability and validity of the VOC as a brief instrument for measuring CR in pwMS. VOC showed good accuracy in discriminating pwMS with low and high CR comparable to specifically designed interviews and emerged as the most influential predictor of cognitive status, independent of demographic and MS clinical features. CR estimation may be crucial to identify pwMS most at risk for future cognitive decline in order to implement cognitive monitoring and timed interventions that can prevent detrimental consequences for patients’ quality of life and their social and professional achievements.
Data availability
Datasets associated with the present study are available upon reasonable request of interested researchers.
References
Chiaravalloti ND, DeLuca J (2008) Cognitive impairment in multiple sclerosis. Lancet Neurol 7(12), 1139–1151. https://doi.org/10.1016/S1474-4422(08)70259-X
Benedict RHB, Zivadinov R (2011) Risk factors for and management of cognitive dysfunction in multiple sclerosis. Nat Rev Neurol 7(6):332–342. https://doi.org/10.1038/nrneurol.2011.61
Stern Y (2009) Cognitive reserve. Neuropsychologia 47:2015–2028
Stern Y (2012) Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol 11(11):1006–1012. https://doi.org/10.1016/S1474-4422(12)70191-6
Zijlmans JL, Lamballais S, Vernooij MW et al (2022) Sociodemographic, lifestyle, physical, and psychosocial determinants of cognitive reserve. J Alzheimer’s Dis 85. https://doi.org/10.3233/JAD-215122
Sumowski JF, Leavitt VM (2013) Cognitive reserve in multiple sclerosis. Mult Scler J 19:1122–1127. https://doi.org/10.1177/1352458513498834
Meng X, D’Arcy C (2012) Education and dementia in the context of the cognitive reserve hypothesis: a systematic review with meta-analyses and qualitative analyses. PLoS One 7. https://doi.org/10.1371/journal.pone.0038268
van Hek M, Kraaykamp G, Wolbers MHJ (2016) Comparing the gender gap in educational attainment: the impact of emancipatory contexts in 33 cohorts across 33 countries. Educ Res Eval 22. https://doi.org/10.1080/13803611.2016.1256222
Rusmaully J, Dugravot A, Moatti JP et al (2017) Contribution of cognitive performance and cognitive decline to associations between socioeconomic factors and dementia: a cohort study. PLoS Med 14. https://doi.org/10.1371/journal.pmed.1002334
Cosentino S, Stern Y (2013) Consideration of cognitive reserve. In: Handbook on the neuropsychology of aging and dementia. 11–23
Leoń I, Garciá-García J, Roldań-Tapia L (2014) Estimating cognitive reserve in healthy adults using the cognitive reserve scale. PLoS One 9. https://doi.org/10.1371/journal.pone.0102632
Altieri M, Siciliano M, Pappacena S, et al (2018) Psychometric properties of the Italian version of the Cognitive Reserve Scale (I-CRS). Neurol Sci 39. https://doi.org/10.1007/s10072-018-3432-0
Wilson RS, Barnes LL, Bennett DA (2003) Assessment of lifetime participation in cognitively stimulating activities. J Clin Exp Neuropsychol 25. https://doi.org/10.1076/jcen.25.5.634.14572
Nucci M, Mapelli D, Mondini S (2012) Cognitive Reserve Index questionnaire (CRIq): a new instrument for measuring cognitive reserve. Aging Clin Exp Res 24. https://doi.org/10.3275/7800
Stanovich KE, Cunningham AE (1993) Where does knowledge come from? Specific associations between print exposure and information acquisition. J Educ Psychol 85. https://doi.org/10.1037/0022-0663.85.2.211
Staff RT, Murray AD, Deary IJ, Whalley LJ (2004) What provides cerebral reserve? Brain 127
Santangelo G, Bisecco A, Trojano L, et al (2018) Cognitive performance in multiple sclerosis: the contribution of intellectual enrichment and brain MRI measures. J Neurol 265. https://doi.org/10.1007/s00415-018-8905-9
Sumowski JF, Wylie GR, Deluca J, Chiaravalloti N (2010) Intellectual enrichment is linked to cerebral efficiency in multiple sclerosis: functional magnetic resonance imaging evidence for cognitive reserve. Brain 133. https://doi.org/10.1093/brain/awp307
Santangelo G, Altieri M, Gallo A, Trojano L (2019) Does cognitive reserve play any role in multiple sclerosis? A meta-analytic study. Mult Scler Relat Disord 30. https://doi.org/10.1016/j.msard.2019.02.017
Santangelo G, Altieri M, Enzinger C et al (2019) Cognitive reserve and neuropsychological performance in multiple sclerosis: a meta-analysis. Neuropsychology 33. https://doi.org/10.1037/neu0000520
Thompson AJ, Banwell BL, Barkhof F et al (2018) Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 17(2):162–173. https://doi.org/10.1016/S1474-4422(17)30470-2
Amato MP, Portaccio E, Goretti B et al (2006) The Rao’s Brief Repeatable Battery and Stroop Test: normative values with age, education and gender corrections in an Italian population. Mult Scler 12. https://doi.org/10.1177/1352458506070933
Ifantopoulou P, Artemiadis AK, Bakirtzis C et al (2019) Cognitive and brain reserve in multiple sclerosis––a cross-sectional study. Mult Scler Relat Disord 35. https://doi.org/10.1016/j.msard.2019.07.027
Artemiadis A, Bakirtzis C, Ifantopoulou P et al (2020) The role of cognitive reserve in multiple sclerosis: a cross-sectional study in 526 patients. Mult Scler Relat Disord 41:. https://doi.org/10.1016/j.msard.2020.102047
Sacco R, Santangelo G, Stamenova S et al (2016) Psychometric properties and validity of Beck Depression Inventory II in multiple sclerosis. Eur J Neurol 23:744–750. https://doi.org/10.1111/ene.12932
Santangelo G, Sacco R, Siciliano M et al (2016) Anxiety in multiple sclerosis: psychometric properties of the State-Trait Anxiety Inventory. Acta Neurol Scand 134:458–466. https://doi.org/10.1111/ane.12564
Maggi G, Altieri M, Ilardi CR, Santangelo G (2022) Validation of a short Italian version of the Barratt Impulsiveness Scale (BIS-15) in non-clinical subjects: psychometric properties and normative data. Neurol Sci. https://doi.org/10.1007/s10072-022-06047-2
Maggi G, D’Iorio A, Aiello EN et al (2023) Psychometrics and diagnostics of the Italian version of the Beck Depression Inventory-II (BDI-II) in Parkinson’s disease. Neurol Sci. https://doi.org/10.1007/s10072-023-06619-w
Altieri M, Maggi G, Rippa V, Santangelo G (2023) Evaluation of apathy in non-clinical populations: validation, psychometric properties, and normative data of the Italian version of Apathy-Motivation Index (AMI). Neurol Sci. https://doi.org/10.1007/s10072-023-06774-0
Altieri M, Maggi G, Giacobbe C, Santangelo G (2024) Psychometric properties and normative data of the Italian version of the Cognitive Function at Work Questionnaire: a screening tool for detecting subjective cognitive complaints at work. Neurol Sci. https://doi.org/10.1007/s10072-023-07265-y
Maggi G, Vitale C, Giacobbe C et al (2024) Validation of the Italian version of the Questionnaire for Impulsive-Compulsive Disorders in Parkinson’s Disease - Rating Scale (QUIP-RS) in an Italian Parkinson’s disease cohort. Neurol Sci. https://doi.org/10.1007/s10072-024-07304-2
Cronbach LJ (1951) Coefficient alpha and the internal structure of tests. Psychometrika 16:297–334. https://doi.org/10.1007/BF02310555
Schisterman EF, Perkins NJ, Liu A, Bondell H (2005) Optimal cut-point and its corresponding Youden index to discriminate individuals using pooled blood samples. Epidemiology 16. https://doi.org/10.1097/01.ede.0000147512.81966.ba
De Oliveira MO, Nitrini R, Yassuda MS, Brucki SMD (2014) Vocabulary is an appropriate measure of premorbid intelligence in a sample with heterogeneous educational level in brazil. Behav Neurol 2014. https://doi.org/10.1155/2014/875960
Lezak MD, Howieson DB, Loring DW et al (2004) Neuropsychological assessment. Oxford University Press, New York
Stern Y (2006) Cognitive reserve and Alzheimer disease. Alzheimer Dis Assoc Disord 20(2):112–117. https://doi.org/10.1097/01.wad.0000213815.20177.19
Ahmadi MM, Lu S, Chan Y et al (2017) Static and dynamic cognitive reserve proxy measures: interactions with Alzheimer’s disease neuropathology and cognition. J Alzheimers Dis Parkinsonism 07. https://doi.org/10.4172/2161-0460.1000390
Panico F, Sagliano L, Magliacano A et al (2023) The relationship between cognitive reserve and cognition in healthy adults: a systematic review. Curr Psychol 42. https://doi.org/10.1007/s12144-022-03523-y
Mattioli F, Bellomi F, Stampatori C et al (2011) Depression, disability and cognitive impairment in multiple sclerosis: a cross sectional Italian study. Neurol Sci 32. https://doi.org/10.1007/s10072-011-0624-2
Patel VP, Walker LAS, Feinstein A (2018) Revisiting cognitive reserve and cognition in multiple sclerosis: a closer look at depression. Mult Scler 24. https://doi.org/10.1177/1352458517692887
Siepman TAM, Janssens ACJW, De Koning I et al (2008) The role of disability and depression in cognitive functioning within 2 years after multiple sclerosis diagnosis. J Neurol 255. https://doi.org/10.1007/s00415-008-0814-x
Lynch SG, Parmenter BA, Denney DR (2005) The association between cognitive impairment and physical disability in multiple sclerosis. Mult Scler 11. https://doi.org/10.1191/1352458505ms1182oa
Sumowski JF, Chiaravalloti N, Wylie G, Deluca J (2009) Cognitive reserve moderates the negative effect of brain atrophy on cognitive efficiency in multiple sclerosis. J Int Neuropsychol Soc 15. https://doi.org/10.1017/S1355617709090912
Iqbal SA, Komal SA (2017) Analyzing the effectiveness of vocabulary knowledge scale on learning and enhancing vocabulary through extensive reading. Engl Lang Teach 10. https://doi.org/10.5539/elt.v10n9p36
Funding
Open access funding provided by Università degli Studi della Campania Luigi Vanvitelli within the CRUI-CARE Agreement. The research was partially supported by the Italian Ministry of Health.
The University of Campania “Luigi Vanvitelli” joined the Italy Transformative Agreement for the funding of article processing charge (APC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Antonio Gallo reports a relationship with Biogen that includes the following: consulting or advisory, speaking and lecture fees, and travel reimbursement. Antonio Gallo reports a relationship with Merck Serono that includes the following: consulting or advisory, speaking and lecture fees, and travel reimbursement. Antonio Gallo reports a relationship with Mylan ITALIA Srl that includes the following: consulting or advisory, speaking and lecture fees, and travel reimbursement. Antonio Gallo reports a relationship with Novartis that includes the following: consulting or advisory, speaking and lecture fees, and travel reimbursement. Antonio Gallo reports a relationship with Roche that includes the following: consulting or advisory, speaking and lecture fees, and travel reimbursement. Antonio Gallo reports a relationship with Sanofi Genzyme that includes the following: consulting or advisory, speaking and lecture fees, and travel reimbursement. Antonio Gallo reports a relationship with Teva Health that includes the following: consulting or advisory, speaking and lecture fees, and travel reimbursement.
Alvino Bisecco reports a relationship with Biogen that includes the following: consulting or advisory and speaking and lecture fees. Alvino Bisecco reports a relationship with Roche that includes the following: consulting or advisory and speaking and lecture fees. Alvino Bisecco reports a relationship with Merck & Co Inc that includes the following: consulting or advisory and speaking and lecture fees. Alvino Bisecco reports a relationship with Celgene Corp Los Angeles that includes the following: consulting or advisory and speaking and lecture fees. Alvino Bisecco reports a relationship with Sanofi Genzyme that includes the following: consulting or advisory and speaking and lecture fees.
Rosaria Sacco received compensation for consulting fees and speaking activities from Biogen Idec, Merck, Novartis, Sanofi, and Roche.
Ethical approval and informed consent
Participants provided informed consent. This study was approved by the Local Ethics Committees.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Gianpaolo Maggi and Manuela Altieri share co-first authorship.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maggi, G., Altieri, M., Risi, M. et al. Vocabulary knowledge as a reliable proxy of cognitive reserve in multiple sclerosis: a validation study. Neurol Sci 45, 3931–3938 (2024). https://doi.org/10.1007/s10072-024-07388-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-024-07388-w