Abstract
Purpose
Umbilical hernia with concomitant rectus abdominus diastasis (RAD) is potentially associated with higher recurrence. Open and laparoscopic techniques have already been described, however, recent endoscopic methods show great promise. Therefore, our aim was to establish the risks and benefits of performing total endoscopic-assisted linea alba reconstruction (TESLAR).
Methods
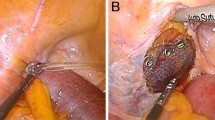
A retrospective review from 28/03/2018 to 01/05/2019 of TESLAR patients was undertaken. Data collected included medical history, operative notes and postoperative course. Statistical analyses were performed using univariate analysis. Operative technique began with a subcutaneous dissection from the lateral borders of anterior rectus sheath, lower costal margin, and pubic bone. The defect was defined and subsequently reduced. Anterior rectus sheath was subsequently plicated and if a mesh was inserted, an on-lay mesh was placed.
Results
21 patients were identified with an 8:13 male to female ratio. Mean age and BMI were 53.1 and 29.7, respectively. 19/21 patients reported post-operative complications requiring reintervention. 17/21 patients had a seroma, all requiring draining with a minority (5/21) requiring formal excision. Univariate analysis showed age (p < 0.001), BMI (p < 0.001) and female gender (p = 0.022) were significantly associated with repeated number of seroma aspirations.
Conclusion
TESLAR is associated with high rates of seroma and reintervention, including revisional surgery. Open repair should be considered as an alternative strategy for hernia and RAD repair.




Similar content being viewed by others
References
Brauman D (2008) Diastasis recti: clinical anatomy. Plast Reconstr Surg 122:1564–1569. https://doi.org/10.1097/PRS.0b013e3181882493
Mommers EHH, Ponten JEH, Al Omar AK et al (2017) The general surgeon’s perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc 31:4934–4949. https://doi.org/10.1007/s00464-017-5607-9
Mitura K, Skolimowska-Rzewuska M, Rzewuska A, Wyrzykowska D (2020) Is mesh always necessary in every small umbilical hernia repair? Comparison of standardized primary sutured versus patch repair: retrospective cohort study. Hernia J Hernias Abdom Wall Surg. https://doi.org/10.1007/s10029-020-02170-1
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia J Hernias Abdom Wall Surg 22:1–165. https://doi.org/10.1007/s10029-017-1668-x
Köhler G, Luketina R-R, Emmanuel K (2015) Sutured repair of primary small umbilical and epigastric hernias: concomitant rectus diastasis is a significant risk factor for recurrence. World J Surg 39:121–126. https://doi.org/10.1007/s00268-014-2765-y(Discussion 127)
Kaufmann R, Halm JA, Eker HH et al (2018) Mesh versus suture repair of umbilical hernia in adults: a randomised, double-blind, controlled, multicentre trial. Lancet Lond Engl 391:860–869. https://doi.org/10.1016/S0140-6736(18)30298-8
Christoffersen MW, Helgstrand F, Rosenberg J et al (2013) Lower reoperation rate for recurrence after mesh versus sutured elective repair in small umbilical and epigastric hernias. A nationwide register study. World J Surg 37:2548–2552. https://doi.org/10.1007/s00268-013-2160-0
Jessen ML, Öberg S, Rosenberg J (2019) Treatment options for abdominal rectus diastasis. Front Surg. https://doi.org/10.3389/fsurg.2019.00065
Veríssimo P, Nahas FX, Barbosa MV et al (2014) Is it possible to repair diastasis recti and shorten the aponeurosis at the same time? Aesthet Plast Surg 38:379–386. https://doi.org/10.1007/s00266-014-0272-z
Siddiky AH, Kapadia CR (2010) Laparoscopic plication of the linea alba as a repair for diastasis recti—a mesh free approach. J Surg Case Rep 2010:3. https://doi.org/10.1093/jscr/2010.5.3
Corvino A, Rosa DD, Sbordone C et al (2019) Diastasis of rectus abdominis muscles: patterns of anatomical variation as demonstrated by ultrasound. Pol J Radiol 84:e542–e548. https://doi.org/10.5114/pjr.2019.91303
Nahas FX (2001) An aesthetic classification of the abdomen based on the myoaponeurotic layer. Plast Reconstr Surg 108:1787–1795. https://doi.org/10.1097/00006534-200111000-00057(Discussion 1796–1797)
Schwarz J, Reinpold W, Bittner R (2017) Endoscopic mini/less open sublay technique (EMILOS)-a new technique for ventral hernia repair. Langenbecks Arch Surg 402:173–180. https://doi.org/10.1007/s00423-016-1522-0
Lockwood T (1998) Rectus muscle diastasis in males: primary indication for endoscopically assisted abdominoplasty. Plast Reconstr Surg 101:1685–1691. https://doi.org/10.1097/00006534-199805000-00042(Discussion 1692–1694)
Core GB, Mizgala CL, Bowen JC, Vasconez LO (1995) Endoscopic abdominoplasty with repair of diastasis recti and abdominal wall hernia. Clin Plast Surg 22:707–722
Eaves FF, Nahai F, Bostwick J (1996) Endoscopic abdominoplasty and endoscopically assisted miniabdominoplasty. Clin Plast Surg 23:599–616 (Discussion 617)
Shankar DA, Itani KMF, O’Brien WJ, Sanchez VM (2017) Factors associated with long-term outcomes of umbilical hernia repair. JAMA Surg 152:461–466. https://doi.org/10.1001/jamasurg.2016.5052
Venclauskas L, Silanskaite J, Kiudelis M (2008) Umbilical hernia: factors indicative of recurrence. Med Kaunas Lith 44:855–859
Ventral Hernia Working Group, Breuing K, Butler CE et al (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148:544–558. https://doi.org/10.1016/j.surg.2010.01.008
Köhler G, Koch OO, Antoniou SA et al (2014) Prevention of subcutaneous seroma formation in open ventral hernia repair using a new low-thrombin fibrin sealant. World J Surg 38:2797–2803. https://doi.org/10.1007/s00268-014-2691-z
Sforza M, Husein R, Atkinson C, Zaccheddu R (2017) Unraveling factors influencing early seroma formation in breast augmentation surgery. Aesthet Surg J 37:301–307. https://doi.org/10.1093/asj/sjw196
Köhler G, Fischer I, Kaltenböck R, Schrittwieser R (2018) Minimal invasive linea alba reconstruction for the treatment of umbilical and epigastric hernias with coexisting rectus abdominis diastasis. J Laparoendosc Adv Surg Tech A 28:1223–1228. https://doi.org/10.1089/lap.2018.0018
Miserez M, Jairam AP, Boersema GSA et al (2019) Resorbable synthetic meshes for abdominal wall defects in preclinical setting: a literature review. J Surg Res 237:67–75. https://doi.org/10.1016/j.jss.2018.11.054
Köckerling F, Botsinis MD, Rohde C et al (2017) Endoscopic-assisted linea alba reconstruction: new technique for treatment of symptomatic umbilical, trocar, and/or epigastric hernias with concomitant rectus abdominis diastasis. Eur Surg 49:71. https://doi.org/10.1007/s10353-017-0473-1
Claus CMP, Malcher F, Cavazzola LT et al (2018) Subcutaneous onlay laparoscopic approach (scola) for ventral hernia and rectus abdominis diastasis repair: technical description and initial results. Arq Bras Cir Dig ABCD Braz Arch Dig Surg 31:e1399. https://doi.org/10.1590/0102-672020180001e1399
Vasileiadou K, Kosmidis C, Anthimidis G et al (2017) Cyanoacrylate adhesive reduces seroma production after modified radical mastectomy or quadrantectomy with lymph node dissection—a prospective randomized clinical trial. Clin Breast Cancer 17:595–600. https://doi.org/10.1016/j.clbc.2017.04.004
Chen C-F, Lin S-F, Hung C-F, Chou P (2016) Risk of infection is associated more with drain duration than daily drainage volume in prosthesis-based breast reconstruction: a cohort study. Medicine (Baltimore) 95:e5605. https://doi.org/10.1097/MD.0000000000005605
Bellido Luque J, Bellido Luque A, Valdivia J et al (2015) Totally endoscopic surgery on diastasis recti associated with midline hernias. The advantages of a minimally invasive approach. Prospective cohort study. Hernia J Hernias Abdom Wall Surg 19:493–501. https://doi.org/10.1007/s10029-014-1300-2
Dudai M, Gilboa I (2019) Intraoperative hypertonic saline irrigation preventing seroma formation and reducing drain secretion in extended endoscopic hernia and linea alba reconstruction glue. Hernia J Hernias Abdom Wall Surg 23:1291–1296
Dudai M (2018) Extended endoscopic linea alba reconstruction glue (eELARG)-new technique for ventral hernias in combination with diastasis recti-abdominal muscles separation. Hernia 22:S185
Shirah, B, Shirah HA (2016) The effectiveness of polypropylene mesh in the open and laparoscopic repair of divarication of the recti. J Med Imp Surg.1:105. https://doi.org/10.4172/jmis.1000105
Shan C-X, Zhang W, Jiang D-Z et al (2010) Prevalence, risk factors, and management of seroma formation after breast approach endoscopic thyroidectomy. World J Surg 34:1817–1822. https://doi.org/10.1007/s00268-010-0597-y
Funding
The authors confirm that no external funding was received for this study.
Author information
Authors and Affiliations
Contributions
PW contributed to the study conception and design. Material preparation, data collection and analysis were performed by AK. The first draft of the manuscript was written by AK. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Aaron Kler and Paul Wilson declare that they have no conflicts of interests or competing interests.
Ethical approval
Ethical approval was waived following an ethics screen deemed that NHS Research Ethics Committee approval was not required by the NHS Health Research Authority.
Human and animal rights
The study was performed in accordance with the ethical standards of the Declaration of Helsinki and its later amendments.
Consent to participate
Informed verbal consent was obtained for participants to use data in this study.
Consent to publish
Informed verbal consent was obtained for participants to use data to be published.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kler, A., Wilson, P. Total endoscopic-assisted linea alba reconstruction (TESLAR) for treatment of umbilical/paraumbilical hernia and rectus abdominus diastasis is associated with unacceptable persistent seroma formation: a single centre experience. Hernia 24, 1379–1385 (2020). https://doi.org/10.1007/s10029-020-02266-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-020-02266-8