Abstract
Objectives
The aim of this study was to investigate whether the use of adjunctive Nd:YAG (1064 nm) laser irradiation to full-mouth scaling and root planing (FM-SRP) may offer additional benefit in the systemic inflammatory status of the patient, as depicted in a variety of systemic biomarkers over FM-SRP alone, up to 12 months after treatment.
Materials and methods
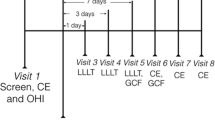
A total of 60 otherwise healthy stage III/IV periodontal patients were equally distributed in 3 groups. The control group received FM-SRP. In laser A group, 1 week after FM-SRP, Nd:YAG laser irradiation was delivered in periodontal pockets with PD ≥ 4 mm using specific settings (3 W, 150 mJ, 20 Hz, 100 μs). In laser B group Nd:YAG laser irradiation was delivered twice, 1 week after FM-SRP and 1 week later with different settings compared to laser A (2 W, 200 mJ, 10 Hz, 100 μs).
Results
A significant reduction (p = 0.038) of IL-1β serum levels at the 6-month time point was observed for laser A group. IL-6 was found statistically significantly increased (p = 0.011) in the control group at the 6-week time point, whereas no difference was reported for the laser-treated groups (laser A, laser B).
Conclusions
The adjunctive use of Nd:YAG laser irradiation, prevented from IL-6 increase after FM-SRP, 6 weeks after treatment. Similarly, Nd:YAG laser irradiation (3 W, 150 mJ, 20 Hz,100 μs) was associated with significantly lower IL-1β levels, 6 months post-operatively.
Clinical relevance
Additional Nd:YAG laser application to FM-SRP may provide a potential beneficial effect on systemic inflammation.
Trial registration number
ISRCTN26692900.
Registration date
09/06/2022.






Similar content being viewed by others
Change history
19 October 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00784-023-05340-4
Notes
PCPUNC 15 mm probe, Hu-Friedy® Hu-Friedy, Chicago, IL, USA.
Piezon Master, EMS, Nyon, Switzerland.
HuFriedy® Hu-Friedy Chicago, IL, USA.
Sealed Envelope Ltd. 2021. Create a blocked randomization list. [Online] Available from: https://www.sealedenvelope.com/simple-randomiser/v1/lists
Fotona XP-2, Model:M001-14F, Code: 69,283.
References
Hajishengallis G (2015) Periodontitis: from microbial immune subversion to systemic inflammation. Nat Rev Immunol 15(1):30–44. https://doi.org/10.1038/nri3785
Needleman I, Garcia R, Gkranias N, Kirkwood KL, Kocher T, Iorio AD, Moreno F, Petrie A (2018) Mean annual attachment, bone level, and tooth loss: a systematic review. J Periodontol 89(Suppl 1):S120–S139. https://doi.org/10.1002/JPER.17-0062
Needleman I, McGrath C, Floyd P, Biddle A (2004) Impact of oral health on the life quality of periodontal patients. J Clin Periodontol 31(6):454–457. https://doi.org/10.1111/j.1600-051X.2004.00498.x
Tonetti MS, Van Dyke TE (2013) Periodontitis and atherosclerotic cardiovascular disease: consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseases. J Periodontol 84(Suppl 4S):S24–S29. https://doi.org/10.1902/jop.2013.1340019
Chapple IL, Genco R (2013) Diabetes and periodontal diseases: consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseases. J Periodontol 84(4 Suppl):S106–S112. https://doi.org/10.1902/jop.2013.1340011
Paraskevas S, Huizinga JD, Loos BG (2008) A systematic review and meta-analyses on C-reactive protein in relation to periodontitis. J Clin Periodontol 35(4):277–290. https://doi.org/10.1111/j.1600-051X.2007.01173.x
Buhlin K, Hultin M, Norderyd O, Persson L, Pockley AG, Rabe P, Klinge B, Gustafsson A (2009) Risk factors for atherosclerosis in cases with severe periodontitis. J Clin Periodontol 36(7):541–549. https://doi.org/10.1111/j.1600-051X.2009.01430.x
Garlet GP (2010) Destructive and protective roles of cytokines in periodontitis: a re-appraisal from host defense and tissue destruction viewpoints. J Dent Res 89(12):1349–1363. https://doi.org/10.1177/0022034510376402
Preshaw PM, Taylor JJ (2011) How has research into cytokine interactions and their role in driving immune responses impacted our understanding of periodontitis? J Clin Periodontol 38(Suppl 11):60–84. https://doi.org/10.1111/j.1600-051X.2010.01671.x
Cekici A, Kantarci A, Hasturk H (2000) Van Dyke TE (2014) Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontol 64(1):57–80. https://doi.org/10.1111/prd.12002
Graves DT, Cochran D (2003) The contribution of interleukin-1 and tumor necrosis factor to periodontal tissue destruction. J Periodontol 74(3):391–401. https://doi.org/10.1902/jop.2003.74.3.391
Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S, Beglundh T, Sculean A, Tonetti MS (2020) EFP workshop participants and methodological consultants. Treatment of stage I-III periodontitis-The EFP S3 level clinical practice guideline. J Clin Periodontol 47(Suppl 22):4–60. https://doi.org/10.1111/jcpe.13290
Suvan J, Leira Y, Moreno Sancho FM, Graziani F, Derks J, Tomasi C (2020) Subgingival instrumentation for treatment of periodontitis A systematic review. J Clin Periodontol 47(Suppl 22):155–175. https://doi.org/10.1111/jcpe.13245
D’Aiuto F, Orlandi M, Gunsolley JC (2013) Evidence that periodontal treatment improves biomarkers and CVD outcomes. J Clin Periodontol 40(Suppl 14):S85-105. https://doi.org/10.1111/jcpe.12061
Orlandi M, Graziani F (2000) D’Aiuto F (2020) Periodontal therapy and cardiovascular risk. Periodontol 83(1):107–124. https://doi.org/10.1111/prd.12299
Jervøe-Storm PM, Semaan E, AlAhdab H, Engel S, Fimmers R, Jepsen S (2006) Clinical outcomes of quadrant root planing versus full-mouth root planing. J Clin Periodontol 33(3):209–215. https://doi.org/10.1111/j.1600-051X.2005.00890.x
Quirynen M, Bollen CM, Vandekerckhove BN, Dekeyser C, Papaioannou W, Eyssen H (1995) Full- vs. partial-mouth disinfection in the treatment of periodontal infections: short-term clinical and microbiological observations. J Dent Res 74(8):1459–1467. https://doi.org/10.1177/00220345950740080501
Quirynen M, Mongardini C, de Soete M, Pauwels M, Coucke W, van Eldere J, van Steenberghe D (2000) The rôle of chlorhexidine in the one-stage full-mouth disinfection treatment of patients with advanced adult periodontitis. Long-term clinical and microbiological observations. J Clin Periodontol 27(8):578–89. https://doi.org/10.1034/j.1600-051x.2000.027008578.x
Morozumi T, Yashima A, Gomi K, Ujiie Y, Izumi Y, Akizuki T, Mizutani K, Takamatsu H, Minabe M, Miyauchi S, Yoshino T, Tanaka M, Tanaka Y, Hokari T, Yoshie H (2018) Increased systemic levels of inflammatory mediators following one-stage full-mouth scaling and root planing. J Periodontal Res 53(4):536–544. https://doi.org/10.1111/jre.12543
Tonetti MS, D’Aiuto F, Nibali L, Donald A, Storry C, Parkar M, Suvan J, Hingorani AD, Vallance P, Deanfield J (2007) Treatment of periodontitis and endothelial function. N Engl J Med 356(9):911–920. https://doi.org/10.1056/NEJMoa063186
Graziani F, Cei S, Orlandi M, Gennai S, Gabriele M, Filice N, Nisi M, D’Aiuto F (2015) Acute-phase response following full-mouth versus quadrant non-surgical periodontal treatment: a randomized clinical trial. J Clin Periodontol 42(9):843–852. https://doi.org/10.1111/jcpe.12451
Graziani F, Gennai S, Marruganti C, Peric M, Ghiadoni L, Marhl U, Petrini M (2023) Acute-phase response following one-stage full-mouth versus quadrant non-surgical periodontal treatment in subjects with comorbid type 2 diabetes: a randomized clinical trial. J Clin Periodontol 50(4):487–499. https://doi.org/10.1111/jcpe.13760
Lofthus JE, Waki MY, Jolkovsky DL, Otomo-Corgel J, Newman MG, Flemmig T, Nachnani S (1991) Bacteremia following subgingival irrigation and scaling and root planing. J Periodontol 62(10):602–607. https://doi.org/10.1902/jop.1991.62.10.602
D’Aiuto F, Nibali L, Mohamed-Ali V, Vallance P, Tonetti MS (2004) Periodontal therapy: a novel non-drug-induced experimental model to study human inflammation. J Periodontal Res 39(5):294–299. https://doi.org/10.1111/j.1600-0765.2004.00741.x
Johnston W, Paterson M, Piela K, Davison E, Simpson A, Goulding M, Ramage G, Sherriff A, Culshaw S (2020) The systemic inflammatory response following hand instrumentation versus ultrasonic instrumentation-a randomized controlled trial. J Clin Periodontol 47(9):1087–1097. https://doi.org/10.1111/jcpe.13342
Sanz M, Marco Del Castillo A, Jepsen S, Gonzalez-Juanatey JR, D’Aiuto F, Bouchard P, Chapple I, Dietrich T, Gotsman I, Graziani F, Herrera D, Loos B, Madianos P, Michel JB, Perel P, Pieske B, Shapira L, Shechter M, Tonetti M, Vlachopoulos C, Wimmer G (2020) Periodontitis and cardiovascular diseases: consensus report. J Clin Periodontol 47(3):268–288. https://doi.org/10.1111/jcpe.13189
Cobb CM (2000) (2017) Lasers and the treatment of periodontitis: the essence and the noise. Periodontol 75(1):205–295. https://doi.org/10.1111/prd.12137
Coluzzi D, Anagnostaki E, Mylona V, Parker S, Lynch E (2020) Do lasers have an adjunctive role in initial non-surgical periodontal therapy? A systematic review. Dent J (Basel) 8(3):93. https://doi.org/10.3390/dj8030093
White JM, Goodis HE, Rose CL (1991) Use of the pulsed Nd:YAG laser for intraoral soft tissue surgery. Lasers Surg Med 11(5):455–461. https://doi.org/10.1002/lsm.1900110511.\
Coluzzi DJ (2004) Fundamentals of dental lasers: science and instruments. Dent Clin North Am 48(4):751–770. https://doi.org/10.1016/j.cden.2004.05.003
Sgolastra F, Severino M, Petrucci A, Gatto R, Monaco A (2014) Nd:YAG laser as an adjunctive treatment to nonsurgical periodontal therapy: a meta-analysis. Lasers Med Sci 29(3):887–895. https://doi.org/10.1007/s10103-013-1293-6
Schwarz F, Aoki A, Becker J, Sculean A (2008) Laser application in non-surgical periodontal therapy: a systematic review. J Clin Periodontol 35(8 Suppl):29–44. https://doi.org/10.1111/j.1600-051X.2008.01259.x
Slot DE, Kranendonk AA, Paraskevas S, Van der Weijden F (2009) The effect of a pulsed Nd:YAG laser in non-surgical periodontal therapy. J Periodontol 80(7):1041–56. https://doi.org/10.1902/jop.2009.080571
Chambrone L, Ramos UD, Reynolds MA (2018) Infrared lasers for the treatment of moderate to severe periodontitis: an American Academy of Periodontology best evidence review. J Periodontol 89(7):743–765. https://doi.org/10.1902/jop.2017.160504
Liu CM, Hou LT, Wong MY, Lan WH (1999) Comparison of Nd:YAG laser versus scaling and root planing in periodontal therapy. J Periodontol 70(11):1276–1282. https://doi.org/10.1902/jop.1999.70.11.1276
Qadri T, Poddani P, Javed F, Tunér J, Gustafsson A (2010) A short-term evaluation of Nd:YAG laser as an adjunct to scaling and root planing in the treatment of periodontal inflammation. J Periodontol 81(8):1161–1166. https://doi.org/10.1902/jop.1999.70.11.1276
Gómez C, Domínguez A, García-Kass AI, García-Nuñez JA (2011) Adjunctive Nd:YAG laser application in chronic periodontitis: clinical, immunological, and microbiological aspects. Lasers Med Sci 26(4):453–463. https://doi.org/10.1007/s10103-010-0795-8
Miyazaki A, Yamaguchi T, Nishikata J, Okuda K, Suda S, Orima K, Kobayashi T, Yamazaki K, Yoshikawa E, Yoshie H (2003) Effects of Nd:YAG and CO2 laser treatment and ultrasonic scaling on periodontal pockets of chronic periodontitis patients. J Periodontol 74(2):175–180. https://doi.org/10.1902/jop.2003.74.2.175
Javed F, Kellesarian SV, Al-Kheraif AA, Ranna V, Qadri T, Yunker M, Malmstrom H, Romanos GE (2016) Effect of Nd:YAG laser-assisted non-surgical periodontal therapy on clinical periodontal and serum biomarkers in patients with and without coronary artery disease: a short-term pilot study. Lasers Surg Med 48(10):929–935. https://doi.org/10.1002/lsm.22483
Markou N, Papadelli A, Nikolidakis D, Pepelassi E, Madianos P, Karoussis IK (2023) Adjunctive Nd:YAG laser irradiation in the treatment of stage III/IV periodontitis: a 12-month, randomized, controlled trial. Clin Oral Investig 27(6):3045–3056. https://doi.org/10.1007/s00784-023-04908-4
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol 89(Suppl 1):S159–S172. https://doi.org/10.1002/JPER.18-0006
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25(4):229–235
Davé S, Van Dyke T (2008) The link between periodontal disease and cardiovascular disease is probably inflammation. Oral Dis 14(2):95–101. https://doi.org/10.1111/j.1601-0825.2007.01438.x
Tonetti MS, Imboden MA, Lang NP (1998) Neutrophil migration into the gingival sulcus is associated with transepithelial gradients of interleukin-8 and ICAM-1. J Periodontol 69(10):1139–1147. https://doi.org/10.1902/jop.1998.69.10.1139
Ioannidou E, Malekzadeh T, Dongari-Bagtzoglou A (2006) Effect of periodontal treatment on serum C-reactive protein levels: a systematic review and meta-analysis. J Periodontol 77(10):1635–1642. https://doi.org/10.1902/jop.2006.050443
Demmer RT, Trinquart L, Zuk A, Fu BC, Blomkvist J, Michalowicz BS, Ravaud P, Desvarieux M (2013) The influence of anti-infective periodontal treatment on C-reactive protein: a systematic review and meta-analysis of randomized controlled trials. Plos One 8(10):e77441. https://doi.org/10.1371/journal.pone.0077441
Freitas CO, Gomes-Filho IS, Naves RC, Nogueira Filho Gda R, Cruz SS, Santos CA, Dunningham L, Miranda LF, Barbosa MD (2012) Influence of periodontal therapy on C-reactive protein level: a systematic review and meta-analysis. J Appl Oral Sci 20(1):1–8. https://doi.org/10.1590/s1678-77572012000100002
Gupta B, Sawhney A, Patil N, Yadav M, Tripathi S, Sinha S, Sharma S, Gupta S (2015) Effect of surgical periodontal therapy on serum C-reactive protein levels using ELISA in both chronic and aggressive periodontitis patient. J Clin Diagn Res 9(10):ZC01-5
de Souza AB, Okawa RT, Silva CO, Araújo MG (2017) Short-term changes on C-reactive protein (CRP) levels after non-surgical periodontal treatment in systemically healthy individuals. Clin Oral Investig 21(1):477–484. https://doi.org/10.1007/s00784-016-1817-0
Moritz A, Schoop U, Goharkhay K, Schauer P, Doertbudak O, Wernisch J, Sperr W (1998) Treatment of periodontal pockets with a diode laser. Lasers Surg Med 22(5):302–311. https://doi.org/10.1002/(sici)1096-9101(1998)22:5%3c302::aid-lsm7%3e3.0.co;2-t
Romanos GE, Henze M, Banihashemi S, Parsanejad HR, Winckler J, Nentwig GH (2004) Removal of epithelium in periodontal pockets following diode (980 nm) laser application in the animal model: an in vitro study. Photomed Laser Surg 22:177–183
Abduljabbar T, Vohra F, Kellesarian SV, Javed F (2017) Efficacy of scaling and root planning with and without adjunct Nd:YAG laser therapy on clinical periodontal parameters and gingival crevicular fluid interleukin 1-beta and tumor necrosis factor-alpha levels among patients with periodontal disease: a prospective randomized split-mouth clinical study. J Photochem Photobiol B 169:70–74. https://doi.org/10.1016/j.jphotobiol.2017.03.001
Dortaj D, Bassir SH, Hakimiha N, Hong H, Aslroosta H, Fekrazad R, Moslemi N (2022) Efficacy of Nd:YAG laser-assisted periodontal therapy for the management of periodontitis: a double-blind split-mouth randomized controlled clinical trial. J Periodontol 93(5):662–672. https://doi.org/10.1002/JPER.21-0242
Saglam M, Kantarci A, Dundar N, Hakki SS (2014) Clinical and biochemical effects of diode laser as an adjunct to nonsurgical treatment of chronic periodontitis: a randomized, controlled clinical trial. Lasers Med Sci 29:37–46. https://doi.org/10.1007/s10103-012-1230-0
Qadri T, Javed F, Johannsen G, Gustafsson A (2015) Role of diode lasers (800–980 nm) as adjuncts to scaling and root planing in the treatment of chronic periodontitis: a systematic review. Photomed Laser Surg 33(11):568–575. https://doi.org/10.1089/pho.2015.3914
Slot DE, Jorritsma KH, Cobb CM, Van der Weijden FA (2014) The effect of the thermal diode laser (wavelength 808–980 nm) in non-surgical periodontal therapy: a systematic review and meta-analysis. J Clin Periodontol 41(7):681–692. https://doi.org/10.1111/jcpe.12233
Aoki A, Sasaki KM, Watanabe H, Ishikawa I (2004) Lasers in nonsurgical periodontal therapy. Periodontol 2000(36):59–97. https://doi.org/10.1111/j.1600-0757.2004.03679.x
Ting CC, Fukuda M, Watanabe T, Sanaoka A, Mitani A, Noguchi T (2014) Morphological alterations of periodontal pocket epithelium following Nd:YAG laser irradiation. Photomed Laser Surg 32(12):649–657. https://doi.org/10.1089/pho.2014.3793
Ben Hatit Y, Blum R, Severin C, Maquin M, Jabro MH (1996) The effects of a pulsed Nd:YAG laser on subgingival bacterial flora and on cementum: an in vivo study. J Clin Laser Med Surg 14(3):137–143. https://doi.org/10.1089/clm.1996.14.137
Ezber A, Taşdemir İ, Yılmaz HE, Narin F, Sağlam M (2023) Different application procedures of Nd:YAG laser as an adjunct to scaling and root planning in smokers with stage III grade C periodontitis: a single-blind, randomized controlled trial. Ir J Med Sci 192(1):457–466. https://doi.org/10.1007/s11845-022-02940-z
Grzech-Leśniak K, Sculean A, Gašpirc B (2018) Laser reduction of specific microorganisms in the periodontal pocket using Er:YAG and Nd:YAG lasers: a randomized controlled clinical study. Lasers Med Sci 33(7):1461–1470. https://doi.org/10.1007/s10103-018-2491-z
Grzech-Leśniak K, Belvin BR, Lewis JP, Golob Deeb J (2020) Treatment with Nd:YAG laser irradiation combined with sodium hypochlorite or hydrogen peroxide irrigation on periodontal path- ogens: an in vitro study. Photobiomodul Photomed Laser Surg 39(1):46–52. https://doi.org/10.1089/photob.2019.4775
Eltas A, Orbak R (2012) Effect of 1,064-nm Nd:YAG laser therapy on GCF IL-1β and MMP-8 levels in patients with chronic periodontitis. Lasers Med Sci 27(3):543–550. https://doi.org/10.1007/s10103-011-0939-5
Behle JH, Sedaghatfar MH, Demmer RT, Wolf DL, Celenti R, Kebschull M, Belusko PB, Herrera-Abreu M, Lalla E, Papapanou PN (2009) Heterogeneity of systemic inflammatory responses to periodontal therapy. J Clin Periodontol 36(4):287–294. https://doi.org/10.1111/j.1600-051X.2009.01382.x
Ramich T, Asendorf A, Nickles K, Oremek GM, Schubert R, Nibali L, Wohlfeil M, Eickholz P (2018) Inflammatory serum markers up to 5 years after comprehensive periodontal therapy of aggressive and chronic periodontitis. Clin Oral Investig 22(9):3079–3089. https://doi.org/10.1007/s00784-018-2398-x
Birkedal-Hansen H (1993) Role of cytokines and inflammatory mediators in tissue destruction. J Periodontal Res 28(6 Pt 2):500–510. https://doi.org/10.1111/j.1600-0765.1993.tb02113.x
Willerson JT, Ridker PM (2004) Inflammation as a cardiovascular risk factor. Circulation 109(21 Suppl 1):II2-10. https://doi.org/10.1161/01.CIR.0000129535.04194.38
Irwin CR, Myrillas TT (1998) The role of IL-6 in the pathogenesis of periodontal disease. Oral Dis 4(1):43–47. https://doi.org/10.1111/j.1601-0825.1998.tb00255.x
Author information
Authors and Affiliations
Contributions
I.K., N.M., and P.M. have made substantial contributions to conception and design of the study. N.M. has been involved in the patients’ therapies. M.S. and N.M. were involved in data and statistical analysis. N.M, I.K., E.P., and P.M., have been involved in drafting the article. All authors have been involved in revising it critically and have given final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
A written informed consent was obtained from all study participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: This article was originally published with all the captions of the published figures do not provide the right information.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Markou, N., Pepelassi, E., Madianos, P. et al. Systemic inflammatory markers following adjunctive Nd:YAG (1064 nm) laser irradiation to step 2 of periodontal therapy: a 12-month, randomized, controlled trial. Clin Oral Invest 27, 6925–6935 (2023). https://doi.org/10.1007/s00784-023-05309-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05309-3