Abstract
Objectives
The aim of this study was to evaluate the clinical efficacy of the adjunctive use of Nd:YAG laser (1064 nm) to full-mouth scaling and root planning (FMS), in stage III/IV periodontitis patients.
Materials and methods
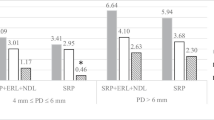
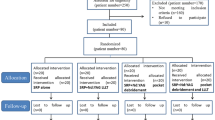
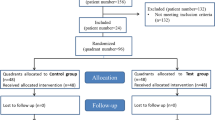
Sixty stage III/IV periodontitis patients were randomly assigned to three groups. The control group received FMS, laser 1 group received combined FMS/single Nd:YAG laser irradiation (3 W, 150 mJ, 20 Hz,100 μs), and laser 2 group received combined FMS/double Nd:YAG laser irradiation with 1-week interval (2.0 W, 200 mJ, 10 Hz, 100 μs). PD, CAL, FMPS, GI, FMBS, and GR were evaluated at baseline, 6 weeks, 3, 6, and 12 months after treatment. Patient-reported outcomes were evaluated 1 week after treatment.
Results
A significant improvement (p < 0.001) for all clinical parameters was observed during the entire study period, with the exception of mean CAL gain for the laser 2 group at 12 months. The percentage of pockets ≤ 4 mm was significantly higher compared to baseline for all groups throughout the study, with no inter-group differences at any time point. Patient-reported analgesic consumption was higher for laser 1 group.
Conclusions
The adjunctive use of Nd:YAG laser irradiation was similarly effective to FMS alone, during the entire study period. A slightly higher, though not statistically significant improvement was reported for PD at 6 and 12 months after a single post-FMS application of Nd:YAG laser for pocket epithelium removal and coagulation.
Clinical relevance
Additional Nd:YAG laser application for sulcular epithelium removal and coagulation may provide minor long-term improvements compared to FMS or laser irradiation for pocket disinfection and detoxification.
Trial registration
ISRCTN26692900. Registration date: 09/06/2022




Similar content being viewed by others
Notes
PCPUNC 15 mm probe, Hu-Friedy® Hu-Friedy Chicago, IL, USA.
Piezon Master, EMS, Nyon, Switzerland.
HuFriedy® Hu-Friedy Chicago, IL, USA.
Sealed Envelope Ltd. 2021. Create a blocked randomization list. [Online] Available from: https://www.sealedenvelope.com/simple-randomiser/v1/lists
Fotona XP-2, Model:M001-14F, Code: 69283.
GraphPad InStat version 3.10 for Windows, GraphPad Software, San Diego California USA, ww.graphpad.com.
References
Cobb CM (1996) Non-surgical pocket therapy: mechanical. Ann Periodontol 1(1):443–490. https://doi.org/10.1902/annals.1996.1.1.443
Suvan J, Leira Y, Moreno Sancho FM, Graziani F, Derks J, Tomasi C (2020) Subgingival instrumentation for treatment of periodontitis. A systematic review. J Clin Periodontol 47(Suppl 22):155–175. https://doi.org/10.1111/jcpe.13245
Van der Weijden GA, Timmerman MF (2020) A systematic review on the clinical efficacy of subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol 29(Suppl 3):55-71; discussion 90-51. https://doi.org/10.1034/j.1600-051X.29.s3.3.x
Buchanan SA, Robertson PB (1987) Calculus removal by scaling/root planing with and without surgical access. J Periodontol 58(3):159–163. https://doi.org/10.1902/jop.1987.58.3.159
Tomasi C, Koutouzis T, Wennström JL (2008) Locally delivered doxycycline as an adjunct to mechanical debridement at retreatment of periodontal pockets. J Periodontol 79(3):431–439. https://doi.org/10.1902/jop.2008.070383
Heitz-Mayfield LJ, Trombelli L, Heitz F, Needleman I, Moles D (2002) A systematic review of the effect of surgical debridement vs non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol 29(Suppl 3):92–102. https://doi.org/10.1034/j.1600-051X.29.s3.5.x
Jervøe-Storm PM, Semaan E, AlAhdab H, Engel S, Fimmers R, Jepsen S (2006) Clinical outcomes of quadrant root planing versus full-mouth root planing. J Clin Periodontol 33(3):209–215. https://doi.org/10.1111/j.1600-051X.2005.00890.x
Quirynen M, Bollen CM, Vandekerckhove BN, Dekeyser C, Papaioannou W, Eyssen H (1995) Full- vs. partial-mouth disinfection in the treatment of periodontal infections: short-term clinical and microbiological observations. J Dent Res 74(8):1459–1467. https://doi.org/10.1177/00220345950740080501
Quirynen M, Mongardini C, de Soete M, Pauwels M, Coucke W, van Eldere J, vanSteenberghe D (2000) The rôle of chlorhexidine in the one-stage full-mouth disinfection treatment of patients with advanced adult periodontitis, Long-term clinical and\microbiological observations. J Clin Periodontol 27(8):578–589. https://doi.org/10.1034/j.1600-051x.2000.027008578.x
Santuchi CC, Cortelli SC, Cortelli JR, Cota LO, Alencar CO, Costa FO (2015) Pre-and post-treatment experiences of fear, anxiety, and pain among chronic periodontitis patients treated by scaling and root planing per quadrant versus one-stage full-mouth disinfection: a 6-month randomized controlled clinical trial. J Clin Periodontol 42(11):1024–1031. https://doi.org/10.1111/jcpe.12472
Eberhard J, Jepsen S, Jervøe-Storm PM, Needleman I, Worthington HV (2015) Full-mouth treatment modalities (within 24 hours) for chronic periodontitis in adults. Cochrane Database Syst Rev 17(4):CD004622. https://doi.org/10.1002/14651858.CD004622.pub3
Fang H, Han M, Li QL, Cao CY, Xia R, Zhang ZH (2016) Comparison of full-mouth disinfection and quadrant-wise scaling in the treatment of adult chronic periodontitis: a systematic review and meta-analysis. J Periodontal Res 51(4):417–430. https://doi.org/10.1111/jre.12326
Aoki A, Mizutani K, Schwarz F et al (2000) (2015) Periodontal and peri-implant wound healing following laser therapy. Periodontol 68(1):217–269. https://doi.org/10.1111/prd.12080
Cobb CM (2000) (2017) Lasers and the treatment of periodontitis: the essence and the noise. Periodontol 75(1):205–295. https://doi.org/10.1111/prd.12137
White JM, Goodis HE, Rose CL (1991) Rose, use of the pulsed Nd:YAG laser for intraoral soft tissue surgery. Lasers Surg Med 11(5):455–461. https://doi.org/10.1002/lsm.1900110511
Coluzzi DJ (2004) Fundamentals of dental lasers: science and instruments. Dent Clin North Am 48(4):751–770. https://doi.org/10.1016/j.cden.2004.05.003
Gold SI, Vilardi MA (1994) Pulsed laser beam effects on gingiva. J Clin Periodontol 21(6):391–396. https://doi.org/10.1111/j.1600-051X.1994.tb00735.x
Giannelli M, Bani D, Viti C et al (2012) Comparative evaluation of the effects of different photoablative laser irradiation protocols on the gingiva of periodontopathic patients. Photomed Laser Surg 30(4):222–230. https://doi.org/10.1089/pho.2011.3172
Ting CC, Fukuda M, Watanabe T, Sanaoka A, Mitani A, Noguchi T (2014) Morphological alterations of periodontal pocket epithelium following Nd:YAG laser irradiation. Photomed Laser Surg 32(12):649–657. https://doi.org/10.1089/pho.2014.3793
Yukna RA, Carr RL, Evans GH (2007) Histologic evaluation of an Nd:YAG laser-assisted new attachment procedure in humans. Int J Periodontics Restorative Dent 27(6):577–587
Nevins ML, Camelo M, Schupbach P, Kim SW, Kim DM, Nevins M (2012) Human clinical and histologic evaluation of laser-assisted new attachment procedure. Int J Periodontics Restorative Dent 32(5):497–507
Sgolastra F, Severino M, Petrucci A, Gatto R, Monaco A (2014) Nd:YAG laser as an adjunctive treatment to nonsurgical periodontal therapy: a meta-analysis. Lasers Med Sci 29(3):87–895
Schwarz F, Aoki A, Becker J, Sculean A (2008) Laser application in non-surgical periodontal therapy: a systematic review. J Clin Periodontol 35(8 Suppl):29–44. https://doi.org/10.1111/j.1600-051X.2008.01259.x
Slot DE, Kranendonk AA, Paraskevas S, Van der Weijden F (2009) The effect of a pulsed Nd:YAG laser in non-surgical periodontal therapy. J Periodontol 80(7):1041–1056. https://doi.org/10.1902/jop.2009.080571
Chambrone L, Ramos UD, Reynolds MA (2018) Infrared lasers for the treatment of moderate to severe periodontitis: an American Academy of Periodontology best evidence review. J Periodontol 89(7):743–765. https://doi.org/10.1902/jop.2017.160504
Armitage GC (1999) Development of a classification system for periodontal diseases and conditions. Ann Periodontol 4(1):1–6. https://doi.org/10.1902/annals.1999.4.1.1
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol 89(Suppl 1):S159–S172. https://doi.org/10.1002/JPER.18-0006
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25(4):229–235
Lin LI (1989) A concordance correlation coefficient to evaluate reproducibility. Biometrics 45(1):255–268
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8(2):135–160. https://doi.org/10.1177/096228029900800204
Raffetto N (2004) Lasers for initial periodontal therapy. Dent Clin North Am 48(4):923–936. https://doi.org/10.1016/j.cden.2004.05.007
de Andrade AK, Feist IS, Pannuti CM, Cai S, Zezell DM, De Micheli G (2008) Nd:YAG laser clinical assisted in class II furcation treatment. Lasers Med Sci 23(4):341–347. https://doi.org/10.1007/s10103-007-0482-6
Qadri T, Poddani P, Javed F, Tunér J, Gustafsson A (2010) A short-term evaluation of Nd:YAG laser as an adjunct to scaling and root planing in the treatment of periodontal inflammation. J Periodontol 1(8):1161–1166. https://doi.org/10.1902/jop.2010.090700
Eltas A, Orbak R (2012) Clinical effects of Nd:YAG laser applications during nonsurgical periodontal treatment in smoking and nonsmoking patients with chronic periodontitis. Photomed Laser Surg 30(7):360–366. https://doi.org/10.1089/pho.2011.3184
Eltas A, Orbak R (2012) Effect of 1,064-nm Nd:YAG laser therapy on GCF IL-1β and MMP-8 levels in patients with chronic periodontitis. Lasers Med Sci 27(3):543–550. https://doi.org/10.1007/s10103-011-0939-5
Dortaj D, Bassir SH, Hakimiha N, Hong H, Aslroosta H, Fekrazad R, Moslemi N (2022) Efficacy of Nd:YAG laser-assisted periodontal therapy for the management of periodontitis: a double-blind split-mouth randomized controlled clinical trial. J Periodontol 93(5):662–672. https://doi.org/10.1002/JPER.21-0242
Dilsiz A, Sevinc S (2015) Trauma from instrumentation after non-surgical periodontal treatment with ultrasonic scalers and Nd:YAG laser. Acta Odontol Scand 73(2):144–149. https://doi.org/10.3109/00016357.2014.961955
Mills MP, Rosen PS, Chambrone L et al (2018) American Academy of Periodontology best evidence consensus statement on the efficacy of laser therapy used alone or as an adjunct to non-surgical and surgical treatment of periodontitis and peri-implant diseases. J Periodontol 89(7):737–742. https://doi.org/10.1002/JPER.17-0356
Grzech-Leśniak K, Belvin BR, Lewis JP, Golob Deeb J (2020) Treatment with Nd:YAG laser irradiation combined with sodium hypochlorite or hydrogen peroxide irrigation on periodontal pathogens: an in vitro study. Photobiomodul Photomed Laser Surg 39(1):46–52. https://doi.org/10.1089/photob.2019.4775
Slot DE, Timmerman MF, Versteeg PA, van der Velden U, van der Weijden FA (2012) Adjunctive clinical effect of a water-cooled Nd:YAG laser in a periodontal maintenance care programme: a randomized controlled trial. J Clin Periodontol 39(12):1159–1165. https://doi.org/10.1111/jcpe.12007
Mizutani K, Aoki A, Coluzzi D et al (2016) Lasers in minimally invasive periodontal and peri-implant therapy. Periodontol 200071(1):185–212. https://doi.org/10.1111/prd.12123
Coluzzi DJ (2002) Lasers and soft tissue curettage: an update. Compend Contin Educ Dent 23(11A):1104–1111
White JM, Fagan MC, Goodis HE (1994) Intrapulpal temperatures during pulsed Nd:YAG laser treatment of dentin, in vitro. J Periodontol 65(3):255–259. https://doi.org/10.1902/jop.1994.65.3.255
Aoki A, Sasaki KM, Watanabe H, Ishikawa I (2004) Lasers in nonsurgical periodontal therapy. Periodontol 2000(36):59–97. https://doi.org/10.1111/j.1600-0757.2004.03679.x
Arisu HD, Turkoz E, Bala O (2006) Effects of Nd:YAG laser irradiation on osteob-last cell cultures. Lasers Med Sci 21(3):175–180. https://doi.org/10.1007/s10103-006-0398-6
Sağlam M, Köseoğlu S, Taşdemir I, Erbak Yılmaz H, Savran L, Sütçü R (2017) Combined application of Er:YAG and Nd:YAG lasers in treatment of chronic periodontitis. A split-mouth, single-blind, randomized controlled trial. J Periodontal Res 52(5):853–862. https://doi.org/10.1111/jre.12454
Grzech-Leśniak K, Sculean A, Gašpirc B (2018) Laser reduction of specific microorganisms in the periodontal pocket using Er:YAG and Nd:YAG lasers: a randomized controlled clinical study. Lasers Med Sci 33(7):1461–1470. https://doi.org/10.1007/s10103-018-2491-z
Loos BG, Needleman I (2020) Endpoints of active periodontal therapy. J Clin Periodontol 47(Suppl 22):61–71. https://doi.org/10.1111/jcpe.13253
Slot DE, Kranendonk AA, Van der Reijden WA et al (2011) Adjunctive effect of a water-cooled Nd:YAG laser in the treatment of chronic periodontitis. J Clin Periodontol 38(5):470–478. https://doi.org/10.1111/j.1600-051X.2010.01695.x
Sanz M, Bäumer A, Buduneli N et al (2015) Effect of professional mechanical plaque removal on secondary prevention of periodontitis and the complications of gingival and periodontal preventive measures: consensus report of group 4 of the 11th European Workshop on Periodontology on effective prevention of periodontal and peri-implant diseases. J Clin Periodontol 42(Suppl16):S214–S220. https://doi.org/10.1111/jcpe.12367
Johnson GK, Hill M (2004) Cigarette smoking and the periodontal patient. J Periodontol 75(2):196–209. https://doi.org/10.1902/jop.2004.75.2.196
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
P.M., I.K. and N.M. have made substantial contributions to conception and design of the study. A.P. has been involved in data collection. N.M. has been involved in the patients’ therapies. D.N. has been involved in data collection, interpretation and statistical analysis. P.M., E.P., I.K. and N.M. have been involved in drafting the article. All authors have been involved in revising it critically and have given final approval of the version to be published. The authors report no conflict of interest to this study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
A written informed consent was obtained from all study participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Markou, N., Papadelli, A., Nikolidakis, D. et al. Adjunctive Nd:YAG laser irradiation in the treatment of stage III/IV periodontitis: a 12-month, randomized, controlled trial. Clin Oral Invest 27, 3045–3056 (2023). https://doi.org/10.1007/s00784-023-04908-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-04908-4