Abstract
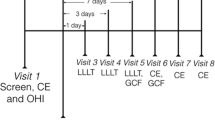
In recent years, the use of laser radiation has been investigated as an alternative or adjunctive tool to conventional procedures employed in the treatment of periodontal disease. Various beneficial characteristics of Nd:YAG laser radiation, such as hemostatic and bactericidal effects, might lead to improved treatment outcomes. The objective of the present study was to examine the clinical, microbiological, and anti-inflammatory efficacy of Nd:YAG laser periodontal pocket irradiation as an adjunct to scaling and root planing (SRP). Thirty patients with chronic periodontitis (CP) were randomly assigned in parallel groups to receive SRP alone or SRP followed by Nd:YAG laser (λ = 1,064 nm) (SRP+NDL). Probing pocket depth (PPD), bleeding on probing (BOP), and plaque index (PI) were recorded, and samples of gingival crevicular fluid (GCF) and subgingival microbiota were taken at baseline and post-therapy (4 and 8 weeks after treatment). The laser therapy was performed 1 day after the SRP procedure. The GCF samples were analyzed for interleukin-1beta (IL-1β), tumor necrosis factor alpha (TNF-α), and total antioxidative status (TAS). Microbiological samples were cultured and analyzed for ten bacteria. No statistically significant differences were detected for clinical or microbiological variables between SRP and SRP+NDL treatments. However, levels of IL-1 β in GCF were significantly lower after SRP+NDL treatment when compared to IL-1 β levels obtained by SRP alone after 4 weeks of treatment. Levels of TNF-α were significantly lower after the SRP+NDL treatment during post-therapy. TAS of GCF increased during post-therapy after the SRP+NDL treatment. However, after SRP alone, it remained constant. In this short-term clinical study Nd:YAG laser radiation in the treatment of CP is showed to be a potential adjunct to conventional SRP.



Similar content being viewed by others
References
Armitage GC (1999) Development of a classification system for periodontal diseases and conditions. Ann Periodontol 4:1–7
Potera C (1999) Forging a link between biofilms and disease. Science 19(283)(5409):1837–1839
Socransky SS, Haffajee AD (2002) Dental biofilms: difficult therapeutic targets. Periodontol 28:12–55
Waterman WH, Sha’afi RI (1995) A mitogen-activated protein kinase independent pathway involved in the phosphorylation and activation of cytosolic phospholipase A2 in human neutrophils stimulated with tumor necrosis factor-alpha. Biochem Biophys Res Commun 209 (Suppl.1): 271–278
Batista AC, Silva TA, Chun JH, Lara VS (2002) Nitric oxide synthesis and severity of human periodontal disease. Oral Dis 8 (Suppl.5):254–260
Chapple ILC (1997) Reactive oxygen species and antioxidants in inflammatory diseases. J Clin Periodontol 24(Suppl 5):287–296
Chapple ILC, Brock GR, Milward MR, Ling N, Matthews JB (2007) Compromised GCF total antioxidant capacity in periodontitis: cause or effect? J Clin Periodontol 34:103–110
Abbas AK, Litchtman AH, Pober JS (2000) Cellular and molecular immunology, chapter 3, 4th edn. WB Saunders, Philadelphia
Gowen M, Mundy GR (1986) Actions of recombinant IL-α and interferon-α on bone resorption in vitro. J Immunol 136:2478–2482
Billingham ME (1987) Cytokines as inflammatory mediators. Br Med Bull 43:350–357
Takatis DN, Schneerberger G, Dziak R (1988) Recombinant interleukin-1 stimulates prostraglandin E2 production by osteoblastic cells: synergy with parathyroid hormone. Calc Tiss Inter 42:358–362
Bertolini DR, Nedwin GE, Bringman TS, Smith DD, Mundy GR (1986) Stimulation of bone resorption and inhibition of bone formation in vitro by human tumor necrosis factors. Nature 319:516–518
Meikle MC, Atkinson SJ, Ward RV, Murphy J, Reynolds JJ (1989) Gingival fibroblasts degrade type 1 collagen films when stimulated with tumor necrosis factor and IL-1 evidence that breakdown is mediated by metalloproteinase. J Periodontal Res 24:207–213
Graves DT, Cochran D (2003) The contribution of interleukin-1 and tumor necrosis factor to periodontal tissue destruction. J Periodontol 74:391–401
Hock J, Krishnan V, Onyia J, Bidwell J, Milas J, Stanislaus D (2001) Osteoblast apoptosis and bone turnover. J Bone Min Res 16:975–984
Cugini MA, Haffajee AD, Smith C, Kent RL Jr, Sokransky SS (2000) The effect of scaling and root planning on the clinical and microbiological parameters of periodontal diseases: 12-month results. J Clin Periodontol 27:30–36
Kreisler M, Meyer Ch, Daubländer M, Willershausen-Zönnchen B, d’Hoedt B (2001) Effect of diode laser irradiation on the attachment rate of periodontal ligament cells: an in vitro study. J Periodontol 72:1312–1317
Kreisler M, Kohnen W, Marinello C, Schoof J, Langnau E, Jansen B, d’Hoedt B (2003) Antimicrobial efficacy of semiconductor laser irradiation on implant surfaces. Int J Oral Maxillofacial Implants 18:706–711
Liu CM, Hou LT, Wong MY, Lan WH (1999) Comparison of Nd:YAG laser versus scaling and root planning in periodontal therapy. J Periodontol 70:1276–1282
Schwarz F, Sculean A, Berakdar M, Szathmari L, Georg T, Becker J (2003) In vivo and in vitro effects of an Er:YAG laser, a GaAlAs diode laser, and scaling and root planning on periodontally diseased root surfaces: a comparative histologic study. Lasers Surg Med 32:359–366
Schwarz F, Aoki A, Sculean A, Becker J (2009) The impact of laser application on periodontal and peri-implant wound healing. Periodontol 51:79–108
Chapple ILC, Landini G, Griffiths GS, Patel NC, Ward RSN (1999) Calibration of the Periotron 8000® and 6000® by polynomial regression. J Periodontal Res 34:79–86
Ben Hatit Y, Blum R, Severin C, Maquin M, Jabro MH (1996) The effects of a pulsed Nd:YAG laser on subgingival bacterial flora on cementum: an in vivo study. J Clin Laser Med Surg 14:137–143
Neill ME, Melloning JT (1997) Clinical efficacy of the Nd:YAG laser for combination periodontitis therapy. Pract Periodontics Aesthet Dent 9 (Suppl.6):1–5
Radvar M, MacFarlane TW, MacKenzie D, Whitters CJ, Payne AP, Kinane DF (1996) An evaluation of the Nd:YAG laser in periodontal pocket therapy. British Dent J 57:180–185
Bader HI (2000) Use of laser in periodontic. Dent Clin North Am 44:779–91
Gómez C, Bisheimer M, Costela A, García-Moreno I, García A, García JA (2009) Evaluation of the effects of Er:YAG and Nd:YAG lasers and ultrasonic instrumentation on root surfaces. Photomed Laser Surg 27:43–48
Miyazaki A, Yamaguchi T, Nishikata J, Okuda K, Suda S, Orima K, Kobayashi T, Yamazaki K, Yoshikawa E, Yoshie H (2003) Effects of Nd:YAG and CO2 laser treatment and ultrasonic scaling on periodontal pockets of chronic periodontitis patients. J Periodontol 74:175–180
Faizuddin M, Bharathi SH, Rohini NV (2003) Estimation of interleukin-1 beta levels in the gingival crevicular fluid in health and in inflammatory periodontal disease. J Periodontal Res 38:111–114
Goutoudi P, Diza E, Arvantidou M (2004) Effect of periodontal therapy on crevicular fluid interleukin-1β and interleukin-10 levels in chronic periodontitis. J Dent 32:511–520
Orozco A, Gemmel E, Bickel M, Seymour GJ (2006) Interleukin 1β, interleukin-12 and interleukin-18 levels in gingival fluid and serum of patients with gingivitis and periodontitis. Oral Microbiol Immunol 21:256–260
Shimizu N, Yamaguchi M, Goseki T, Shibata Y, Takiguchi A, Iwasawa T, Abiko Y (1995) Inhibition of prostaglandin E2 and interleukin 1β production by low-power laser irradiation in stretched human periodontal ligament cells. J Dent Res 74:1382–1388
Funk JO, Kruse A, Kirchner H (1992) Cytokine production after helium-neon laser irradiation in cultures of human peripheral blood mononuclear cells. J Photochem Photobiol B: Biol 16:347–355
Kana J, Hutschenreiter G, Haina D, Waidelich W (1981) Effect of low-power density irradiation on healing of open skin wounds in rats. Arch Surg 116:294–296
Safavi SM, Kazemi B, Esmaeili M, Fallah A (2008) Effects of low-level He-Ne laser irradiation on the gene expression of IL-1β, TNF-α, IFN, TGF, bFGF, and PDGF in rat’s gingival. Lasers Med Sci 23:331–335
Domínguez A, Gómez C, García-Kass AI, García-Núñez JA (2010) IL-1β, TNF-α, total antioxidative status and microbiological findings in chronic periodontitis treated with fluorescence-controlled Er:YAG laser radiation. Lasers Surg Med 42:24–31
Teng YT (2003) The role of oxygen radicals in human disease with particular acquired immunity and periodontal disease progression. Crit Rev Oral Dis 6:138–151
Brock GR, Matthews J, Butterworth C, Chapple ILC (2002) Plasma and crevicular fluid antioxidant defense in periodontitis and health. J Dent Res 81 (Spec Iss A): Abstract 1524
Tsai CC, Chen HS, Chen SL, Ho YP, Ho KY, Wu YM, Hung CC (2005) Lipid peroxidation: a possible role in the induction and progression of chronic periodontitis. J Periodontal Res 40:378–384
Gibson MT, Mangat D, Gagliano G, Wilson M, Fletcher J, Bulman J, Newman HN (1994) Evaluation of the efficacy of a redox agent in the treatment of chronic periodontitis. J Clin Periodontol 21:690–700
Wilson M, Gibson M, Strahan D, Harvey W (1992) A preliminary evaluation of the use of a redox agent in the treatment of chronic periodontitis. J Periodontal Res 27:522–527
Ower PC, Ciantar M, Newman HN, Wilson M, Bulman JS (1995) The effects on chronic periodontitis of a subgingivally-placed redox agent in a slow release device. J Clin Periodontol 22:494–500
Sbordone L, Ramaglia L, Gulleta E, Iacono V (1990) Recolonization of the subgingival microflora after scaling and root planning in human periodontitis. J Periodontol 61:579–584
Socransky SS, Haffajee AD, Cugini MA, Smit C, Kent RL Jr (1998) Microbial complexes in subgingival plaque. J Clin Periodontol 25:134–144
Harper DS, Robinson PJ (1987) Correlation of histometric, microbial, and clinical indicators of periodontal disease status before and after root planning. J Clin Periodontol 14:190–196
Moritz A, Gutknecht N, Doertbudak O, Goharkhay K, Schoop U, Schauer P, Sperr W (1997) Bacterial reduction in periodontal pockets through irradiation with a diode laser: a pilot study. J Clin Laser Med Surg 15:33–37
Acknowledgments
The work described in the present study was supported by Intramural Project 200880I215 of the Spanish CSIC. In addition, the authors wish to thank Schütz Dental Group, Weil-Dental GmbH Enterprise for lending us their Nd:YAG laser system. The authors report no conflicts of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gómez, C., Domínguez, A., García-Kass, A.I. et al. Adjunctive Nd:YAG laser application in chronic periodontitis: clinical, immunological, and microbiological aspects. Lasers Med Sci 26, 453–463 (2011). https://doi.org/10.1007/s10103-010-0795-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-010-0795-8