Abstract
Background
Cervical posterior instrumentation and fusion is often performed to avoid post-laminectomy kyphosis. However, larger comparative analyses of cervical laminectomy with or without fusion are sparse.
Methods
A retrospective, two-center, comparative cohort study included patients after stand-alone dorsal laminectomy with (n = 91) or without (n = 46) additional fusion for degenerative cervical myelopathy with a median follow-up of 59 (interquartile range (IQR) 52) months. The primary outcome was the C2-7 Cobb angle and secondary outcomes were Neck Disability Index (NDI), modified Japanese Orthopaedic Association (mJOA) scale, revision rates, T1 slope and C2-7 sagittal vertical axis (C2-7 SVA) at final follow-up. Logistic regression analysis adjusted for potential confounders (i.e. age, operated levels, and follow-up). Results: Preoperative C2-7 Cobb angle and T1 slope were higher in the laminectomy group, while the C2-7 SVA was similar. The decrease in C2-7 Cobb angle from pre- to postoperatively was more pronounced in the laminectomy group (− 6° (IQR 20) versus −1° (IQR 7), p = 0.002). When adjusting for confounders, the decrease in C2-7 Cobb angle remained higher in the laminectomy group (coefficient − 12 (95% confidence interval (CI) −18 to −5), p = 0.001). However, there were no adjusted differences for postoperative NDI (− 11 (− 23 to 2), p = 0.10), mJOA, revision rates, T1 slope and C2-7 SVA. Conclusion: Posterior cervical laminectomy without fusion is associated with mild loss of cervical lordosis of around 6° in the mid-term after approximately five years, however without any clinical relevance regarding NDI or mJOA in well-selected patients (particularly in shorter segment laminectomies of < 3 levels).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Degenerative cervical myelopathy (DCM) is a major problem of the aging spine and occurs as a multifactorial process. It develops from different underlying pathologies, such as ossification of the posterior longitudinal ligament (OPLL) and ligamentum flavum, degenerative disc disease and cervical spondylosis with common progression over time. [1,2,3] Around 3% of patients become symptomatic per year with an average time to diagnosis of 6 years. Up to 20–60% develop a serious neurological deficit and the need for surgery. [4,5,6]
Posterior laminectomy [7] plus/minus fusion [8] or laminoplasty [9] are relevant approaches from posteriorly to treat DCM. These are usually chosen if the compressive forces of the spinal canal are located posteriorly without relevant foraminal stenosis or in OPLL. Around 70% of North American Spine Surgeons favor addressing multilevel cervical myelopathy with a posterior laminectomy plus fusion. [10] This may be due to the fact that laminectomy and fusion is considered superior in maintaining lordosis with lower kyphotic rates and more stable C2-7 angles compared to laminectomy alone. Yet, laminectomy and fusion has a complication rate of up to 10% for screw misplacement and a C5 palsy has been reported to occur in up to 12%. [8, 11,12,13] It is more time-consuming, leads to a higher blood loss, longer hospital stay, and adds additional costs of approximately 4700 US Dollars. [14, 15] The given rate of postlaminectomy kyphosis in the newer literature lies between 18–21%, while a recent study of Laiginhas reported a low kyphosis rate of only 4%. [16,17,18]
Studies examining the difference between laminoplasty versus fusion are somewhat common, [19,20,21,22,23,24] while comparisons of laminectomy without fusion versus fusion are still rare. [15, 25,26,27,28,29] For example, Kotter et al. focused on clinical outcomes and de Dios et al. showed no clear clinical benefit of one cohort over the other. [15, 25] Therefore, we aimed to question the need of an additional cervical posterior fusion after cervical laminectomy for cervical myelopathy.
Methods
Prior to starting with data collection, approval of the local ethics committees and informed consent from patients were obtained (BASEC Number 2020 – 00573 and CAPCR ID: 20–6023).
We performed a retrospective, two-center, comparative cohort study between 2002 to 2019. All patients with stand-alone dorsal laminectomy from one institution and additional fusion from another institution for DCM were included. This was feasible because in one institution those approaches were commonly done with laminectomy only, while in the other institution, these surgeries were commonly performed with additional fusion. Surgeries in the laminectomy group were done by 10 senior Orthopedic surgeons and 2 neurosurgeons at the Balgrist University Hospital Balgrist, Switzerland. In the laminectomy and fusion group, surgeries were all done by one neurosurgeon at the University Hospital in Toronto, Canada.
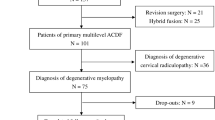
For the patient selection regarding the surgical approach in the laminectomy group, a similar approach to the one published by Farrokhi et al. was used. [30] Similar in- and exclusion criteria were selected for both groups. Other diseases than DCM (tumors of the spine, cervical trauma, vascular diseases) were not considered. The flow chart for in- and exclusion criteria can be found in Fig. 1. In the laminectomy group (n = 139), 93 patients were excluded (due to radiological follow-up < 1 year (n = 91) or missing radiological data on the C2-7 Cobb angle (n = 2), leaving 46 patients for analysis. In the fusion group, the sample was a convenience sample derived from another study, which studied patients that underwent cervical posterior laminectomy and instrumented fusion (n = 179). [26] After exclusion of certain patients (missing radiological data on the C2-7 Cobb angle (n = 66) or information about myelopathy (n = 4), prior surgery (n = 11), and radiological follow-up < 1 year (n = 7), there were 91 patienta available for further analysis. [26]
The primary outcome was development of kyphosis quantified by differences of C2-7 Cobb angles and secondary outcomes were quantifications of clinical consequences, measured by Neck Disability Index (NDI), modified Japanese Orthopaedic Association (mJOA) scale, revision rate and further radiological data. Measurements were done by three trained residents. The mJOA was calculated based on data from the available pre- and postoperative medical charts. Logistic regression analysis adjusted for potential confounders (i.e. age, operated levels and follow-up). The radiographic measurements are shown in Fig. 2. Lordosis was defined as an C2-7 cobb angle above 0°, kyphosis below 0° [31].
A X-ray of cervical spine with measurements of alignment. The C2-7 angle was measured as the angle between vertical lines drawn from lines parallel to the inferior endplates of C2 and C7 before surgery and at final follow-up. The T1 slope was the angle between the superior endplate of T1 and a horizontal line. The C2-7 sagittal vertical axis (C2-7 SVA) was measured as the distance of the C2 plumb line from the posterior superior end plate of C7. Postoperative x-rays after cervical larminectomy B without and C with fusion
Data are given as medians (interquartile range (IQR) with the addition of means and standard deviations (SD) where more information is needed) and absolute numbers (percentages (%)). Wilcoxon rank sum and chi-squared tests were used to compare pre- and postoperative values. Logistic regression used the Wald test. Age was chosen as an a priori counder, while levels and follow-up were chosen due to their preoperative difference in groups. In a further analysis, the preoperative radiographic measurements were taken into account by adjusting for the preoperative T1 slope. Stata (version IC 13.1; StataCorp LP, College Station, Texas, United States of America (USA)) was used for the analysis.
Results
The final analysis consisted of 137 patients. 46 patients (34%) underwent laminectomy only, while 91 (66%) had additional instrumented fusion. There were no significant differences in age (median 67 (IQR 15) versus 63 (14), p = 0.92) and gender (males: n = 35 (76%) versus n = 56 (62%), p = 0.09). There was also no difference in preoperative mJOA (14 (2) versus 14 (4), p = 0.11). The number of decompressed levels was lower in the laminectomy group (median and mean 2 (IQR and SD 1) versus 5 (IQR and SD1), p < 0.001). The follow-up time was longer in the laminectomy group (median 59 (IQR 80) and mean 74 (SD 47) versus 59 (IQR 38) and mean 53 (SD 34) months, p = 0.019).
Overall, there were more additional surgeries needed in the laminectomy group (n = 7 (15%) versus n = 4 (4%), p = 0.028) without differences in the time to revision (15 (IQR 136) versus 27 (27) months, p = 0.57). Additional surgeries in the laminectomy group were due adjacent segment degeneration (n = 1, after 170 months); skip level adjacent segment degeneration (n = 2; after 21 months after 140 months), postlaminectomy kyphosis (n = 2; foraminal stenosis after 15 months with 10° lordosis to 25° kyphosis; myelopathy after 16 months with 5° lordosis to 55° kyphosis), infection (n = 2 after 0 months and 2 months), and segment instability (n = 1, anterolisthesis after 141 months). All four revisions in the fusion group were due to distal adjacent segment disease. Two (4%) revisions for postlaminectomy kyphosis (due to foraminal stenosis after 15 months with 10° lordosis to 25° kyphosis and myelopathy after 16 months with 5° lordosis to 55° kyphosis) were needed in the laminectomy group after 21 months and 140 months, while none (0%) were needed in the laminectomy and fusion group (p = 0.046).
At final follow-up, the NDI was lower in the laminectomy group (12 (30%) versus 33 (36%) percent, p = 0.004). There were no differences in the mJOA (15 (IQR 5) versus 15 (3), p = 0.78) (Table 1).
Preoperatively, the C2-7 Cobb angle and T1 slope were higher in the laminectomy group (15 (18) versus 6 (10) degrees, p < 0.001, and 35 (13) versus 33 (18) degrees, p = 0.017, respectively). The preoperative C2-7 SVA was similar (30 (20) versus 23 (28) millimeters (mm), p = 0.25). Postoperatively, there were no differences considering C2-7 Cobb angle and T1 slope (10 (20) versus 5 (18) degrees, p = 0.19, and 24 (17 vs 36 (26) degrees, p = 0.42, respectively). The postoperative C2-7 SVA was lower in the laminectomy group (32 (24) versus 41 (29) mm, p = 0.025). The reduction in C2-7 Cobb angle and T1 slope from pre- to postoperative (at final follow-up) was more pronounced in the laminectomy group (− 6 (20) versus − 1 (7) degrees, p = 0.002, and − 1 (12) vs 3 (14) degrees, p = 0.010, respectively), without any difference in the C2-7 SVA (8 (14) versus 6 (18) mm, p = 0.75. (Table 2).
When adjusting for the confounders, age, operated levels, and follow-up, the decrease in C2-7 Cobb angle was more pronounced in the laminectomy group (− 10 (IQR − 17 to − 3), p = 0.004), but there were no differences for the NDI (coefficient − 11 (95% confidence interval (CI) − 25 to 2), p = 0.09), mJOA (0.3 (95% CI − 0.67 to 1.32), p = 0.513), revision rates (odds ratio 1.0 (95% CI 0.1 to 10), p = 0.99), T1 slope (− 3 (95% CI − 10 to 4), p = 0.42), and C2-7 SVA (0.5 (95% CI − 9 to 10) p = 0.92). (Table 3).
Discussion
The dogma that cervical laminectomy needs additional posterior instrumentation and fusion to avoid postlaminectomy kyphosis is based on limited evidence only. This is one of a few studies comparing laminectomy without fusion versus with additional fusion. [15, 25, 27, 29]. The main finding of our study with a relatively large sample size of 137 patients is a kyphotic change in the C2-7 Cobb angle of 6° after posterior cervical laminectomy compared to 1° after additional fusion after a follow-up of around five years. However, the NDI and number of revisions did not differ between these two groups once corrected for confounders. This indicates that, although additional fusion is associated with a more stable cervical alignment over time, the clinical outcome may be similar. These findings remained stable after adjusting for differences between groups including differences in age, operated levels and follow-up. The fusion as an additional surgical step carries potential additional risks compared to laminectomy alone, which evolve around hardware failure, screw misplacement, pseudarthrosis, and adjacent segment disease, which, in our study, did not pose an issue. [32] This shows that selective laminectomy is feasible in a well-selected patient cohort, especially when decompressing < 3 levels in a preexisting lordotic spine. When performing laminectomy alone, it is crucial to limit post-laminectomy kyphosis by avoiding facetectomy over 25% and a resection of 50% or more of the joint capsule. [11, 16, 33,34,35]
One of the problems is that there is no clear definition of cervical kyphosis. For example, a study group around Grob et al. gave the definition of 4 to − 4° for a straight spine, > 4° for a kyphotic spine and < 4° for a lordotic spine. [36] Löfgren et al. used 5° kyphosis as the cut-off value. [27] Other studies, as the one by Batzdorf and Batzdorff divided the cervical shape into different patterns. [37] Therefore, an exact differentiation of the different shapes and comparison of the different studies seems difficult and different rates of postoperative laminectomy kyphosis might not only find their origin in different surgical techniques and surgeons, but also within different definitions and measurement methods. We therefore opted to provide the changes in absolute values in the degree of kyphosis instead of using arbitrary cut-off values.
The given rate of kyphotic progression for laminectomy without fusion in the literature ranges between 0–48% [38, 39] in older studies, while nowadays, it seems to be lower (i.e. around 18–25%). [16, 17] Akbar et al. proposed a physiologic lordotic cervical spine. Yet, they also state that it must not always be lordotic, but can be straight or kyphotic in the presence of no neurological deficits. [40] Kim et al. found kyphosis in 26% of an asymptomatic collective, whereof 17% were non-reducible. [41] Le Huec confirmed these findings with one-third of patients having an asymptomatic kyphosis. [42]. Therefore, the kyphotic progression of 6° in our patient cohort without additional fusion does not seem clinically relevant.
Most existing comparisons of the literature compare laminoplasty versus laminectomy and fusion [20] or laminoplasty versus laminectomy. [39] Newer studies show a trend toward laminectomy compared toward laminoplasty. [39, 43] A review comparing 7 studies in the presence of OPLL showed superiority of laminectomy and fusion over laminoplasty in maintaining cervical lordosis (p = − 0.01, standardized mean difference − 0.13 (95% CI − 2.03 to − 0.24)). [28] The group around Kotter and Fehlings performed a retrospective post hoc analysis of a prospective observational study. They included 208 out of 757 patients, which were prospectively enrolled in the AO Spine North America or international studies at 26 global sites and a follow up of 24 months. 22 received laminectomy alone while 186 received laminectomy with additional fusion. Patients were evaluated with the mJOA, Nurick score, NDI and SF 36 quality of life measure. An analytic approach was made to evaluate differences at a follow up of 24 months. Preoperative demographics were comparable. Patients with instrumented fusion had a significantly longer duration of surgery (231 min versus 107 min, p < 0.001)) at a comparable length of hospital stay. While patients receiving laminectomy and fusion had clinically meaningful improvements in functional impairment (∆mJOA = 2.48, ∆Nurick = 1.19), patients receiving laminectomies alone did not (∆mJOA = 0.78, ∆Nurick 0.29). Significant changes in the mJOA and Nurick scores from preoperative to 24-months postoperative (mJOA: − 1.70, p = 0.0266; Nurick: − 0.90, p = 0.0241) could be found. The perioperative complications were comparable (p = 0.879). Better functional improvement in DCM patients after laminectomy and fusion was concluded. [25] Our study counteracts to these findings reporting a low radiographic progression of kyphotic deformity without clinical relevance (similar NDI and mJOA) in similar patient cohorts with an increased sample size for laminectomy patients.
The group of de Dios et al. compared the largest group of myelopathy patients from the national Swedish Register with laminectomy alone (n = 412) versus laminectomy with additional fusion (n = 305) in a total of 717 patients. The average operated segments were 3 versus 4, respectively, with a follow-up of five years. They found no differences in clinical outcome, but longer length of hospital stays and implant costs of US $4,700. A major drawback of their study is that data were based on a registry. Therefore, there was high loss to follow-up until five years of 73% leaving a total of 193 patients (n = 93 in the laminectomy group and n = 100 in the fusion group). Imaging was also only available for 68% and 73% of the initial patients, respectively, and postoperative images were not available. Our study, therefore, adds valuable data to the literature in reporting the radiological postoperative course of disease in a large patient cohort. [15]
The group of Löfgren et al. conducted a retrospective cohort study analyzing a group of myelopathy patients (n = 60), who were operated with laminectomy alone for at least 3 levels with an average follow up of 8 years. [27] Congenital stenosis and compressions primary due posterior structures were included. Contraindications were clear kyphosis (> 5°) or instability with a spondylolisthesis (> 2 mm). [44, 45] Mean C2-7 Cobb angle remained similar throughout the postoperative course (9° (SD 9°) preoperatively, 3.4° (11°) postoperatively, and 10° (15°) at the final follow up). The study group did not report an association between sagittal alignment and clinical outcome. [27] This is in line with our findings, while our patient cohort was substantially larger.
Revesz et al. performed a retrospective clinical study with data from the Swedish Spine Registry. 66 individuals treated with laminectomy and fusion were age-matched to 132 patients treated with laminectomy alone. The fusion group had one more segment fused than the laminectomy group (4 versus 3). Both groups showed an improvement in the European Myelopathy Scale (EMS), the Neck Disability Index (NDI), the Numeric Rating Scale (NRS) and EQ-5D Index (EQ-5D) from baseline to 1 year (p ≤ 0.011). There was no additional improvement after 2 years (p ≥ 0.09) with similar values for both groups (e.g. EQ-5D of 0.67 and 0.66, respectively), while NDI was significantly lower in the laminectomy alone group versus the fusion group (NDI of 39 and 27 (p = 0.045)). The study therefore showed similar results and a similar effectiveness of laminectomy with instrumented fusion and laminectomy alone in DCM patients. [29]
Our study is limited by its retrospective nature with potential bias by different patient cohorts. For example, many patients had insufficient data (especially available x-rays) for analysis and, therefore, had to be excluded introducing a potential bias. Yet, we were not able to identify any specific patterns in missing data indicating this bias could also be minimal. Furthermore, preoperative NDI scores were not availble. However, having preoperative mJOA values appears sufficient in providing the clinical severity of the disease. This was addressed by using regression analysis accounting for confounders including differences in decompressed levels, which was lower in the laminectomy group. Additionally, patients were from different continents, which likely introduced other heterogeneity in the patient sample and surgical techniques not addressed in this study. However, this also brings a strength to this study with limitation of bias, because both institutions always adhered to their own strict treatment algorithm favoring laminectomy alone in one institution and additional fusion in the other institution. Another strength lies in a larger sample size including radiological and clinical data. We only evaluated degenerative cervical myelopathy patients, so postlaminectomy kyphosis may still be an issue for other diagnoses, such as tumor resections.
Conclusion
Posterior cervical laminectomy without fusion is associated with a small loss of cervical lordosis around 6° and potentially more revision surgeries in the mid-term after five years; without any clinical relevance regarding the NDI in well-selected patients (particularly in shorter segment laminectomies < 3 levels). Although laminectomy without fusion had more revision surgeries, revisions due to adjacent segment disease were similar.
Data availability
All data analyzed during this study are included in this article.
References
Wilson JR et al (2017) State of the art in degenerative cervical myelopathy: an update on current clinical evidence. Neurosurgery 80(3S):S33–S45
Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG (2015) Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine 40(12):E675–E693
Tetreault L et al (2015) Degenerative cervical myelopathy: a spectrum of related disorders affecting the aging spine. Neurosurgery 77(Suppl 4):S51-67
Sadasivan KK, Reddy RP, Albright JA (1993) The natural history of cervical spondylotic myelopathy. Yale J Biol Med 66(3):235–242
Karadimas SK, Erwin WM, Ely CG, Dettori JR, Fehlings MG (2013) Pathophysiology and natural history of cervical spondylotic myelopathy. Spine 38(22S):S21–S36
Tetreault LA et al (2017) Change in function, pain, and quality of life following structured nonoperative treatment in patients with degenerative cervical myelopathy: a systematic review. Global Spine J 7(3 Suppl):42S-52S
Lu JJ (2007) Cervical laminectomy: technique. Neurosurgery 60(1):S149–S153
Chang V et al (2014) Clinical results of cervical laminectomy and fusion for the treatment of cervical spondylotic myelopathy in 58 consecutive patients. Surg Neurol Int 5(Suppl 3):S133–S137
Hirano Y et al (2018) History and evolution of laminoplasty. Neurosurg Clin N Am 29(1):107–113
Manzano GR et al (2012) A prospective, randomized trial comparing expansile cervical laminoplasty and cervical laminectomy and fusion for multilevel cervical myelopathy. Neurosurgery 70(2):264–277
McAllister BD, Rebholz BJ, Wang JC (2012) Is posterior fusion necessary with laminectomy in the cervical spine? Surg Neurol Int 3(Suppl 3):S225–S231
Al-Mefty O et al (1988) Myelopathic cervical spondylotic lesions demonstrated by magnetic resonance imaging. J Neurosurg 68(2):217–222
Epstein NE, Hollingsworth R (2015) C5 Nerve root palsies following cervical spine surgery: a review. Surg Neurol Int 6(Suppl 4):S154–S163
Goh BC et al (2020) Laminoplasty versus laminectomy and fusion for cervical spondylotic myelopathy: a cost analysis. Spine J 20(11):1770–1775
de Dios E, Heary RF, Lindhagen L, MacDowall A (2022) Laminectomy alone versus laminectomy with fusion for degenerative cervical myelopathy: a long-term study of a national cohort. European Spine J 31(2):334–345
Kaptain GJ et al (2000) Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg 93(2 Suppl):199–204
van Geest S et al (2015) Long-term follow-up of clinical and radiological outcome after cervical laminectomy. Eur Spine J 24(Suppl 2):229–235
Laiginhas AR et al (2015) Long-term clinical and radiological follow-up after laminectomy for cervical spondylotic myelopathy. Surg Neurol Int 6:162
He X et al (2020) Is laminectomy and fusion the better choice than laminoplasty for multilevel cervical myelopathy with signal changes on magnetic resonance imaging? A comparison of two posterior surgeries. BMC Musculoskelet Disord 21(1):423
Lau D et al (2017) Laminoplasty versus laminectomy with posterior spinal fusion for multilevel cervical spondylotic myelopathy: influence of cervical alignment on outcomes. J Neurosurg Spine 27(5):508–517
Zhao H, Ren R, Ma W, Xu S, Peng L, Zhong Z, Zheng Y (2022) Comparison of laminoplasty vs laminectomy for cervical spondylotic myelopathy: a systematic review and meta-analysis. Front Surg 8:790593
Yuan X et al (2019) Comparison of laminectomy and fusion vs laminoplasty in the treatment of multilevel cervical spondylotic myelopathy: a meta-analysis. Medicine (Baltimore) 98(13):e14971
Nakashima H et al (2022) Comparison of laminoplasty and posterior fusion surgery for cervical ossification of posterior longitudinal ligament. Sci Rep 12(1):748
Liu FY et al (2016) Laminoplasty versus laminectomy and fusion for multilevel cervical compressive myelopathy: a meta-analysis. Medicine (Baltimore) 95(23):e3588
Kotter MRN et al (2020) Surgical outcomes following laminectomy with fusion versus laminectomy alone in patients with degenerative cervical myelopathy. Spine 45(24):1696–1703
Rienmüller A et al. (2022) Posterior cervical decompression and instrumented fusion with and without inclusion of C2: a retrospective study. Manuscript in preparation
Lofgren H et al (2020) Sagittal alignment after laminectomy without fusion as treatment for cervical spondylotic myelopathy: follow-up of minimum 4 years postoperatively. Global Spine J 10(4):425–432
Ma L et al (2018) Comparison of laminoplasty versus laminectomy and fusion in the treatment of multilevel cervical ossification of the posterior longitudinal ligament: A systematic review and meta-analysis. Medicine (Baltimore) 97(29):e11542
Revesz DF, Charalampidis A, Gerdhem P (2022) Effectiveness of laminectomy with fusion and laminectomy alone in degenerative cervical myelopathy. Eur Spine J 31(5):1300–1308
Farrokhi MR et al (2016) An evidence-based stepwise surgical approach to cervical spondylotic myelopathy: a narrative review of the current literature. World Neurosurg 94:97–110
Kim B et al (2016) Relationship between T1 slope and loss of lordosis after laminoplasty in patients with cervical ossification of the posterior longitudinal ligament. Spine J 16(2):219–225
Badiee RK et al (2020) Complications following posterior cervical decompression and fusion: a review of incidence, risk factors, and prevention strategies. J Spine Surg 6(1):323–333
Zdeblick TA et al (1992) Cervical stability after foraminotomy. A biomechanical in vitro analysis. J Bone Joint Surg Am 74(1):22–27
Nowinski GP, Visarius H, Nolte LP, Herkowitz HN (1993) A biomechanical comparison of cervical laminaplasty and cervical laminectomy with progressive facetectomy. Spine 18(14):1995–2004
Albert TJ, Vacarro A (1998) Postlaminectomy kyphosis. Spine 23(24):2738–2745
Grob D, Frauenfelder H, Mannion AF (2007) The association between cervical spine curvature and neck pain. Eur Spine J 16(5):669–678
Batzdorf U, Batzdorff A (1988) Analysis of cervical spine curvature in patients with cervical spondylosis. Neurosurgery 22(5):827–836
Kato Y et al (1998) Long-term follow-up results of laminectomy for cervical myelopathy caused by ossification of the posterior longitudinal ligament. J Neurosurg 89(2):217–223
Nurboja B, Kachramanoglou C, Choi D (2012) Cervical laminectomy vs laminoplasty: is there a difference in outcome and postoperative pain? Neurosurgery 70(4):965–970
Akbar M et al (2018) Normal sagittal profile of the cervical spine–must the cervical spine always be lordotic? Orthopade 47(6):460–466
Kim SW et al (2018) Analysis of cervical spine alignment in currently asymptomatic individuals: prevalence of kyphotic posture and its relationship with other spinopelvic parameters. Spine J 18(5):797–810
Le Huec JC, Demezon H, Aunoble S (2015) Sagittal parameters of global cervical balance using EOS imaging: normative values from a prospective cohort of asymptomatic volunteers. Eur Spine J 24(1):63–71
Ohtonari T et al (2020) Facet joint- and nuchal ligament-sparing laminectomy is not inferior to conventional open-door laminoplasty from clinical and radiologic perspectives. World Neurosurg 137:e321–e327
Tamai K, Buser Z, Paholpak P, Sessumpun K, Nakamura H, Wang JC (2018) Can C7 slope substitute the T1 slope?: an analysis using cervical radiographs and kinematic MRIs. Spine 43(7):520–525
Ye IB et al (2020) Can C7 slope be used as a substitute for T1 slope? Radiograph Anal Global Spine J 10(2):148–215
Acknowledgements
We thank the Balgrist Foundation for the financial support to do the patients follow up. We also thank the radiologic staff from Balgrist Radiologist Department, the Unit for clinical and applied research (UCAR) at the Balgrist Campus; especially R. Schüpbach and T. Götschi for their inputs and help during data collection and for designing the study. The abstract of this manuscript was presented at the annual conference of Swiss Orthopaedics in 2022.
Funding
Open access funding provided by University of Zurich. The costs of the appointment were free for the patients as the study was paid out of the Balgrist / UZH Research funds.
Author information
Authors and Affiliations
Contributions
TJ and OTW: conception and design, acquisition of data, analysis and interpretation of data, drafting the manuscript. AKM and CL: acquisition of data. EMM, MGF, JMS, and MF: conception and design, analysis and interpretation of data. All: revision of the manuscript, final approval of the version to be published.
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare no conflict of interests.
Ethical approval
Ethics approval was provided by the local ethics committee (BASEC Number 2020 – 00573 and CAPCR ID: 20–6023).
Consent to participate
Informed consent was obtained where necessary by the ethics committee.
Consent for publication
Ethics approval was provided by the local ethics committee (BASEC Number 2020 – 00573 and CAPCR ID: 20–6023), and informed consent was obtained where deemed necessary by the ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jentzsch, T., Wetzel, O.T., Malhotra, A.K. et al. Cervical kyphosis after posterior cervical laminectomy with and without fusion. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08260-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08260-3