Abstract
Purpose
Preoperative assessment at extreme ages would identify patients at a high risk of developing postoperative complications. The objective of this study was to compare the usefulness of different risk scales in a series of nonagenarian surgical patients.
Methods
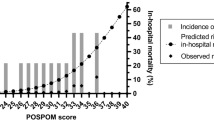
A total of 244 surgical nonagenarians, 148 women (60.7%), median age 91 years (IQR: 90–93), were analysed. The following scales were evaluated: preoperative status (ASA-PS, Charlson Comorbidity Index, Lee Index, Reiss Index, and surgical mortality probability model—S-MPM); intraoperative status (Surgical Apgar Score and SASA score), and, as output variables, surgical outcomes (morbidity measured by the Comprehensive Complication Index—CCI, and death). Univariate analysis and receiver operating characteristic curves (ROC) were performed. Area under ROC curves (AUROC) were evaluated to define the best predictors of poor outcomes.
Results
Operative mortality was 27.0%, and 73.4% presented some type of postoperative complication. Operative mortality was associated with the ASA-PS score (p < 0.001), Reiss Index (p < 0.001), Lee Index (p = 0.010), S-MPM (p < 0.001), Surgical Apgar Score (p < 0.001), SASA score (p < 0.001), and emergency surgery (p < 0.001). Postoperative complications were related to the ASA-PS score (p = 0.001), Reiss Index (p < 0.001), Lee Index (p < 0.001), S-MPM (p < 0.001), Surgical Apgar Score (p < 0.001) and SASA score (p < 0.001). The best predictors of operative mortality and complications were the SASA and Surgical Apgar Score (AUROCs > 0.88).
Conclusion
As in the general population, the Surgical Apgar Score and SASA score are the best predictors of operative mortality and morbidity in nonagenarian patients. These risk scales should be considered in the perioperative management of these patients.


Similar content being viewed by others
References
Dent E, Hoogendijk EO, Cardona-Morrell M, Hillman K. Frailty in emergency departments. Lancet. 2016;387:434.
Ho VP, Schiltz NK, Reimer AP, Madigan EA, Koroukian SM. High-risk comorbidity combinations in older patients undergoing emergency general surgery. J Am Geriatr Soc. 2019;67:503–10.
Vilches-Moraga A, Fox J, Paracha A, Gomez-Quintanilla A, Epstein J, Pearce L. Predicting in-hospital mortality in older general surgical patients. Ann R Coll Surg Engl. 2018;100:529–33.
Rix TE, Bates T. Pre-operative risk scores for the prediction of outcome in elderly people who require emergency surgery. World J Emerg Surg. 2007;2:16.
Farina-Castro R, Roque-Castellano C, Artiles-Armas M, Marchena-Gomez J. Emergency surgery and American Society of Anesthesiologists physical status score are the most influential risk factors of death in nonagenarian surgical patients. Geriatr Gerontol Int. 2019;19:293–8.
Panayi AC, Orkaby AR, Sakthivel D, Endo Y, Varon D, Roh D, Orgill DP, Neppl RL, Javedan H, Bhasin S, Sinha I. Impact of frailty on outcomes in surgical patients: a systematic review and meta-analysis. Am J Surg. 2019;218:393–400.
Dripps R. New classification of physical status. Anesthesiology. 1963;24:111.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Lee TH, Marcantonio ER, Mangione CM, Thomas EJ, Polanczyk CA, Cook EF, Sugarbaker DJ, Donaldson MC, Poss R, Ho KK, Ludwig LE, Pedan A, Goldman L. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–9.
Reiss R, Deutsch A, Nudelman I. Surgical problems in octogenarians: epidemiological analysis of 1,083 consecutive admissions. World J Surg. 1992;16:1011–7.
Glance LG, Lustik SJ, Hannan EL, Osler TM, Mukamel DB, Qian F, Dick AW. The Surgical Mortality Probability Model: derivation and validation of a simple risk prediction rule for noncardiac surgery. Ann Surg. 2012;255:696–702.
Gawande AA, Kwaan MR, Regenbogen SE, Lipsitz SA, Zinner MJ. An Apgar score for surgery. J Am Coll Surg. 2007;204:201–8.
Kinoshita M, Morioka N, Yabuuchi M, Ozaki M. New surgical scoring system to predict postoperative mortality. J Anesth. 2017;31:198–205.
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258:1–7.
de la Plaza LR, Ramia Angel JM, Bellon JM, Arteaga Peralta V, Garcia Amador C, Lopez Marcano AJ, Medina Velasco AA, Gonzalez Sierra B, Manuel VA. Clinical validation of the comprehensive complication index as a measure of postoperative morbidity at a surgical department: a prospective study. Ann Surg. 2018;268:838–44.
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–5.
Irlbeck T, Zwissler B, Bauer A. ASA classification: transition in the course of time and depiction in the literature. Anaesthesist. 2017;66:5–10.
Zerbib P, Kulick JF, Lebuffe G, Khoury-Helou A, Plenier I, Chambon JP. Emergency major abdominal surgery in patients over 85 years of age. World J Surg. 2005;29:820–5.
Pelavski AD, Lacasta A, Rochera MI, de Miguel M, Roige J. Observational study of nonogenarians undergoing emergency, non-trauma surgery. Br J Anaesth. 2011;106:189–93.
Racz J, Dubois L, Katchky A, Wall W. Elective and emergency abdominal surgery in patients 90 years of age or older. Can J Surg. 2012;55:322–8.
Kristensen SD, Knuuti J, Saraste A, Anker S, Botker HE, Hert SD, Ford I, Gonzalez-Juanatey JR, Gorenek B, Heyndrickx GR, Hoeft A, Huber K, Iung B, Kjeldsen KP, Longrois D, Luscher TF, Pierard L, Pocock S, Price S, Roffi M, Sirnes PA, Sousa-Uva M, Voudris V, Funck-Brentano C, Authors/Task Force Members. ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management: the joint task force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesth. Eur Hear J. 2014;35(35):2383–431.
Ford MK, Beattie WS, Wijeysundera DN. Systematic review: prediction of perioperative cardiac complications and mortality by the revised cardiac risk index. Ann Intern Med. 2010;152:26–35.
Lette J, Waters D, Bernier H, Champagne P, Lassonde J, Picard M, Cerino M, Nattel S, Boucher Y, Heyen F, Dube S. Preoperative and long-term cardiac risk assessment. Predictive value of 23 clinical descriptors, 7 multivariate scoring systems, and quantitative dipyridamole imaging in 360 patients. Ann Surg. 1992;216:192–204.
Hirano Y, Takeuchi H, Suda K, Oyama T, Nakamura R, Takahashi T, Kawakubo H, Wada N, Saikawa Y, Obara H, Jinno H, Hasegawa H, Tanabe M, Kitagawa Y. Clinical utility of the Revised Cardiac Risk Index in non-cardiac surgery for elderly patients: a prospective cohort study. Surg Today. 2014;44:277–84.
Boersma E, Kertai MD, Schouten O, Bax JJ, Noordzij P, Steyerberg EW, Schinkel AF, van Santen M, Simoons ML, Thomson IR, Klein J, van Urk H, Poldermans D. Perioperative cardiovascular mortality in noncardiac surgery: validation of the Lee cardiac risk index. Am J Med. 2005;118:1134–41.
Reiss R, Deutsch AA, Nudelman I, Gutman H. Multifactorial analysis of prognostic factors in emergency abdominal surgery in patients above 80 years. Analysis of 154 consecutive cases. Int Surg. 1989;74:93–6.
Leardi S, De Santis C, Ciuca B, Risetti A, Pietroletti R, Simi M. Risk indices in geriatric surgery: ASA index versus Reiss index. Minerva Chir. 1997;52:255–60.
Kenig J, Mastalerz K, Lukasiewicz K, Mitus-Kenig M, Skorus U. The Surgical Apgar Score predicts outcomes of emergency abdominal surgeries both in fit and frail older patients. Arch Gerontol Geriatr. 2018;76:54–9.
Kenig J, Mastalerz K, Mitus J, Kapelanczyk A. The Surgical Apgar score combined with comprehensive geriatric assessment improves short- but not long-term outcome prediction in older patients undergoing abdominal cancer surgery. J Geriatr Oncol. 2018;9:642–8.
Cihoric M, Toft Tengberg L, Bay-Nielsen M, Bang FN. Prediction of outcome after emergency high-risk intra-abdominal surgery using the Surgical Apgar Score. Anesth Analg. 2016;123:1516–21.
Haddow JB, Adwan H, Clark SE, Tayeh S, Antonowicz SS, Jayia P, Chicken DW, Wiggins T, Davenport R, Kaptanis S, Fakhry M, Knowles CH, Elmetwally AS, Geddoa E, Nair MS, Naeem I, Adegbola S, Muirhead LJ, London Surgical Research G. Use of the surgical Apgar score to guide postoperative care. Ann R Coll Surg Engl. 2014;96:352–8.
Artiles-Armas M, Roque-Castellano C, Conde-Martel A, Marchena-Gómez J. The Comprehensive Complication Index is related to frailty in elderly surgical patients. J Surg Res. 2019;244:218–24.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Fariña-Castro, R., Roque-Castellano, C., Artiles-Armas, M. et al. Usefulness of pre- and intraoperative risk scores in nonagenarian surgical patients. J Anesth 34, 650–657 (2020). https://doi.org/10.1007/s00540-020-02799-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-020-02799-3