Abstract
Purpose
Mind–body practices such as qigong, tai chi, or yoga combine physical movements, deep breathing, and meditation techniques aiming to improve how people self-care. Our purpose was to develop an overview of systematic reviews to summarize the available evidence on the effectiveness of mind–body practices for cancer-related symptoms management.
Methods
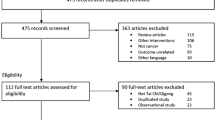
CINAHL, Embase, PsycINFO, PubMed, and the Cochrane Library were used to search systematic reviews with meta-analysis from inception until March 2022. Cancer-related symptoms such as fatigue, pain, psychological measures, and overall quality of life were chosen as outcomes of interest. The methodological quality of each systematic review was assessed using AMSTAR 2. Citation matrices were developed, and the corrected covered area was calculated to explore the potential primary study overlap.
Results
A total of 38 systematic reviews comprising 134 distinct primary studies and 129 separate meta-analyses were included. The items of AMSTAR 2 regarding the review protocol, the reasons to choose a specific research design, and the provision of a list of studies that justify their exclusion were scarcely performed. The primary study overlap was moderate for qigong trials and high for both tai chi and yoga trials. Mainly, we found that qigong showed promising effects to reduce fatigue. Tai chi produced positive effects in reducing anxiety. Yoga improved anxiety, depression, distress, stress, and overall quality of life. Finally, the effects of mind–body practices on pain were inconsistent.
Conclusions
Qigong, tai chi, and yoga could be effective approaches to relief cancer-related symptoms in adults with different cancer diagnoses.



Similar content being viewed by others
Data availability
Not applicable.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Tuo JY, Bi JH, Yuan HY et al (2022) Trends of stomach cancer survival: a systematic review of survival rates from population-based cancer registration. J Dig Dis 23:22–32. https://doi.org/10.1111/1751-2980.13070
Maajani K, Jalali A, Alipour S et al (2019) The global and regional survival rate of women with breast cancer: a systematic review and meta-analysis. Clin Breast Cancer 19:165–177. https://doi.org/10.1016/j.clbc.2019.01.006
Maher J, Petchey L, Greenfield D et al (2018) Implementation of nationwide cancer survivorship plans: experience from the UK. J Cancer Policy 15:76–81. https://doi.org/10.1016/j.jcpo.2018.01.002
Rogers K, McCabe C, Dowling S (2021) What are the holistic experiences of adults living long-term with the consequences of cancer and its treatment? A qualitative evidence synthesis. Eur J Oncol Nurs 50:101864. https://doi.org/10.1016/j.ejon.2020.101864
Goyena R, Fallis A (2019) Throwing light on the consequences of cancer and its treatment. J Chem Inf Model 53:1689–1699
Almeida SN, Elliott R, Silva ER, Sales CMD (2019) Fear of cancer recurrence: a qualitative systematic review and meta-synthesis of patients’ experiences. Clin Psychol Rev 68:13–24. https://doi.org/10.1016/J.CPR.2018.12.001
Tauber NM, O’Toole MS, Dinkel A et al (2019) Effect of psychological intervention on fear of cancer recurrence: a systematic review and meta-analysis. J Clin Oncol 37:2899–2915. https://doi.org/10.1200/JCO.19.00572
Marlow LAV, Waller J, Wardle J (2015) Does lung cancer attract greater stigma than other cancer types? Lung Cancer 88:104–107. https://doi.org/10.1016/J.LUNGCAN.2015.01.024
Iskandar AC, Rochmawati E, Wiechula R (2021) Experiences and perspectives of suffering in cancer: a qualitative systematic review. Eur J Oncol Nurs Off J Eur Oncol Nurs Soc 54:102041. https://doi.org/10.1016/j.ejon.2021.102041
Foster C, Fenlon D (2011) Recovery and self-management support following primary cancer treatment. Br J Cancer 105:S21–S28
Chou FY (2019) Cancer illness perception and self-management of Chinese patients. Asia-Pacific J Oncol Nurs 6:57–63. https://doi.org/10.4103/apjon.apjon-56-18
Harley C, Pini S, Bartlett YK, Velikova G (2015) Defining chronic cancer: patient experiences and self-management needs. BMJ Support Palliat Care 5:343–350. https://doi.org/10.1136/bmjspcare-2012-000200rep
Fasczewski KS, Garner LM, Clark LA et al (2022) Medical therapeutic yoga for multiple sclerosis: examining self-efficacy for physical activity, motivation for physical activity, and quality of life outcomes. Disabil Rehabil 44:106–113. https://doi.org/10.1080/09638288.2020.1760364
Payne H, Roberts A, Jarvis J (2020) The bodymind approach® as transformative learning to promote self-management for patients with medically unexplained symptoms. J Transform Educ 18:114–137. https://doi.org/10.1177/1541344619883892
Murley B, Haas B, Hermanns M et al (2019) Influence of tai chi on self-efficacy, quality of life, and fatigue among patients with cancer receiving chemotherapy: a pilot study brief. J Holist Nurs Off J Am Holist Nurses’ Assoc 37:354–363. https://doi.org/10.1177/0898010119867557
Bai M, Lazenby M (2015) A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med 18:286–298. https://doi.org/10.1089/jpm.2014.0189
Gothe NP, Khan I, Hayes J et al (2019) Yoga effects on brain health: a systematic review of the current literature. Brain Plast 5:105–122. https://doi.org/10.3233/BPL-190084
Cui L, Tao S, Yin H-C et al (2021) Tai Chi chuan alters brain functional network plasticity and promotes cognitive flexibility. Front Psychol 12:665419. https://doi.org/10.3389/fpsyg.2021.665419
Husebø AML, Husebø TL (2017) Quality of life and breast cancer: how can mind−body exercise therapies help? An overview study. Sport (Basel, Switzerland) 5. https://doi.org/10.3390/sports5040079
Zou L, Xiao T, Cao C et al (2021) Tai chi for chronic illness management: synthesizing current evidence from meta-analyses of randomized controlled trials. Am J Med 134:194-205.e12. https://doi.org/10.1016/j.amjmed.2020.08.015
So WWY, Lu EY, Cheung WM, Tsang HWH (2020) Comparing mindful and non-mindful exercises on alleviating anxiety symptoms: a systematic review and meta-analysis. Int J Environ Res Public Health 17:1–16. https://doi.org/10.3390/ijerph17228692
Li J, Shen J, Wu G et al (2018) Mindful exercise versus non-mindful exercise for schizophrenia: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract 32:17–24. https://doi.org/10.1016/j.ctcp.2018.04.003
Meng T, Hu S, Cheng Y, et al (2021) Qigong for women with breast cancer: an updated systematic review and meta-analysis. Complement Ther Med 60:N.PAG-N.PAG. https://doi.org/10.1016/j.ctim.2021.102743
Kuo C-C, Wang C-C, Chang W-L et al (2021) Clinical effects of Baduanjin qigong exercise on cancer patients: a systematic review and meta-analysis on randomized controlled trials. Evidence-Based Complement Altern Med 1–10. https://doi.org/10.1155/2021/6651238
Ni X, Chan RJ, Yates P et al (2019) The effects of Tai Chi on quality of life of cancer survivors: a systematic review and meta-analysis. Support Care Cancer 27:3701–3716. https://doi.org/10.1007/s00520-019-04911-0
Song S, Yu J, Ruan Y et al (2018) Ameliorative effects of Tai Chi on cancer-related fatigue: a meta-analysis of randomized controlled trials. Support Care Cancer 26:2091–2102. https://doi.org/10.1007/s00520-018-4136-y
Armer JS, Lutgendorf SK (2020) The impact of yoga on fatigue in cancer survivorship: a meta-analysis. JNCI Cancer Spectr 4:pkz098. https://doi.org/10.1093/jncics/pkz098
Gonzalez M, Pascoe MC, Yang G et al (2021) Yoga for depression and anxiety symptoms in people with cancer: a systematic review and meta-analysis. Psycho-Oncology 30(8):1196–208. https://doi.org/10.1002/pon.5671
Ioannidis J (2017) Next-generation systematic reviews: prospective meta-analysis, individual-level data, networks and umbrella reviews. Br J Sports Med 51:1456–1458
Bougioukas KI, Liakos A, Tsapas A et al (2018) Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol 93:9–24. https://doi.org/10.1016/j.jclinepi.2017.10.002
Richardson WS, Wilson MC, Nishikawa J, Hayward RS (1995) The well-built clinical question: a key to evidence-based decisions. ACP J Club 123:A12–A13
Krnic Martinic M, Pieper D, Glatt A, Puljak L (2019) Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol 19:1–12. https://doi.org/10.1186/s12874-019-0855-0
Andrews J, Guyatt G, Oxman AD et al (2013) GRADE guidelines: 14. Going from evidence to recommendations: The significance and presentation of recommendations. J Clin Epidemiol 66:719–725. https://doi.org/10.1016/j.jclinepi.2012.03.013
BJ S, BC R, G W, et al (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358. https://doi.org/10.1136/bmj.j4008
Pieper D, Antoine SL, Mathes T et al (2014) Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol 67:368–375. https://doi.org/10.1016/j.jclinepi.2013.11.007
Higgins JPT, Altman DG, Gotzsche P, et al (2011) The Cochrane Collaboration´s tool for assessing risk of bias in randomsed trials. BMJ 18:d5928. doi.gov/22008217.
Yin J, Tang L, Dishman RK (2020) The efficacy of Qigong practice for cancer-related fatigue: A systematic review and meta-analysis of randomized controlled trials. Ment Health Phys Act 19:100347. https://doi.org/10.1016/j.mhpa.2020.100347
Zeng Y, Luo T, Xie H et al (2014) Health benefits of qigong or tai chi for cancer patients: a systematic review and meta-analyses. Complement Ther Med 22:173–186
Zeng Y, Xie X, Cheng ASK (2019) Qigong or Tai Chi in cancer care: an updated systematic review and meta-analysis. Curr Oncol Rep 21:1–6
Cheung DST, Takemura N, Smith R et al (2021) Effect of qigong for sleep disturbance-related symptom clusters in cancer: a systematic review and meta-analysis. Sleep Med 85:108–122. https://doi.org/10.1016/j.sleep.2021.06.036
Duan L, Xu Y, Li M (2020) Effects of mind-body exercise in cancer survivors: a systematic review and meta-analysis. Evidence-Based Complement Altern Med 2020:13. https://doi.org/10.1155/2020/7607161
Tao W-W, Jiang H, Tao X-M et al (2016) Effects of acupuncture, Tuina, Tai Chi, Qigong, and Traditional Chinese medicine Five-Element Music Therapy on symptom management and quality of life for cancer patients: a meta-analysis. J Pain Symptom Manag 51:728–747. https://doi.org/10.1016/j.jpainsymman.2015.11.027
Lin W-F, Zhong M-F, Zhou Q-H et al (2019) Efficacy of complementary and integrative medicine on health-related quality of life in cancer patients: a systematic review and meta-analysis. Cancer Manag Res 11:6663–6680. https://doi.org/10.2147/CMAR.S195935
Zeng Y, Huang M, Cheng ASK et al (2014) Meta-analysis of the effects of exercise intervention on quality of life in breast cancer survivors. Breast Cancer 21:262–274. https://doi.org/10.1007/s12282-014-0521-7
Lee MS, Choi T-Y, Ernst E (2010) Tai chi for breast cancer patients: a systematic review. Breast Cancer Res Treat 120:309–316. https://doi.org/10.1007/s10549-010-0741-2
Xiang Y, Lu L, Chen X, Wen Z (2017) Does Tai Chi relieve fatigue? A systematic review and meta-analysis of randomized controlled trials. PLoS One 12. https://doi.org/10.1371/journal.pone.0174872
Luo X-C, Liu J, Fu J, et al (2020) Effect of Tai Chi Chuan in breast cancer patients: A systematic review and meta-analysis. Front Oncol 10. https://doi.org/10.3389/fonc.2020.00607
Liu L, Tan H, Yu S et al (2020) The effectiveness of tai chi in breast cancer patients: a systematic review and meta-analysis. Complement Ther Clin Pract 38:101078
Pan Y, Yang K, Shi X, et al (2015) Tai Chi Chuan exercise for patients with breast cancer: a systematic review and meta-analysis. Evidence-based Complement Altern Med 1–15. https://doi.org/10.1155/2015/535237
Cai Q, Cai SB, Chen JK et al (2022) Tai Chi for anxiety and depression symptoms in cancer, stroke, heart failure, and chronic obstructive pulmonary disease: a systematic review and meta-analysis. Complement Ther Clin Pract 46:101510. https://doi.org/10.1016/j.ctcp.2021.101510
Chen Y-W, Hunt MA, Campbell KL et al (2016) The effect of Tai Chi on four chronic conditions-cancer, osteoarthritis, heart failure and chronic obstructive pulmonary disease: a systematic review and meta-analyses. Br J Sports Med 50:397–407. https://doi.org/10.1136/bjsports-2014-094388
Yi L-J, Tian X, Jin Y-F et al (2021) Effects of yoga on health-related quality, physical health and psychological health in women with breast cancer receiving chemotherapy: a systematic review and meta-analysis. Ann Palliat Med 10:1961–1975. https://doi.org/10.21037/apm-20-1484
Duong N, Davis H, Robinson PD et al (2017) Mind and body practices for fatigue reduction in patients with cancer and hematopoietic stem cell transplant recipients: a systematic review and meta-analysis. Crit Rev Oncol Hematol 120:210–216
Lin H-P, Kuo Y-H, Tai W-Y, Liu H-E (2021) Exercise effects on fatigue in breast cancer survivors after treatments: a systematic review and meta-analysis. Int J Nurs Pract e12989. https://doi.org/10.1111/ijn.12989
Pan Y, Yang K, Wang Y et al (2017) Could yoga practice improve treatment-related side effects and quality of life for women with breast cancer? A systematic review and meta-analysis. Asia-Pacific J Clin Oncol 13:e79–e95
Lin K-Y, Hu Y-T, Chang K-J, et al (2011) Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a Meta-Analysis. Evidence-based Complement Altern Med 8:1–12. 2011/659876
Zhang J, Yang K, Tian J, Wang C (2012) Effects of yoga on psychologic function and quality of life in women with breast cancer: a meta-analysis of randomized controlled trials. J Altern Complement Med 18:994–1002. https://doi.org/10.1089/acm.2011.0514
Cramer H, Lauche R, Klose P et al (2017) Yoga for improving health-related quality of life, mental health and cancer-related symptoms in women diagnosed with breast cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010802.pub2
O’Neill M, Samaroo D, Lopez C, et al (2020) the effect of yoga interventions on cancer-related fatigue and quality of life for women with breast cancer: a systematic review and meta-analysis of randomized controlled trials. Integr Cancer Ther 19. https://doi.org/10.1177/1534735420959882
Cramer H, Lange S, Klose P et al (2012) Yoga for breast cancer patients and survivors: a systematic review and meta-analysis. BMC Cancer 12:1–13
Zuo X-L, Li Q, Gao F et al (2016) Effects of yoga on negative emotions in patients with breast cancer: a meta-analysis of randomized controlled trials. Int J Nurs Sci 3:299–306. https://doi.org/10.1016/j.ijnss.2016.07.009
Patsou ED, Alexias GD, Anagnostopoulos FG, Karamouzis MV (2017) Effects of physical activity on depressive symptoms during breast cancer survivorship: a meta-analysis of randomised control trials. ESMO Open 2:e000271. https://doi.org/10.1136/esmoopen-2017-000271
Shneerson C, Taskila T, Gale N et al (2013) The effect of complementary and alternative medicine on the quality of life of cancer survivors: a systematic review and meta-analyses. Complement Ther Med 21:417–429. https://doi.org/10.1016/j.ctim.2013.05.003
Dong B, Xie C, Jing X et al (2019) Yoga has a solid effect on cancer-related fatigue in patients with breast cancer: a meta-analysis. Breast Cancer Res Treat 177:5–16. https://doi.org/10.1007/s10549-019-05278-w
Hsueh E-J, Loh E-W, Lin JJ-A, Tam K-W (2021) Effects of yoga on improving quality of life in patients with breast cancer: a meta-analysis of randomized controlled trials. Breast Cancer 28:264–276. https://doi.org/10.1007/s12282-020-01209-6
Song J, Wang T, Wang Y et al (2021) The effectiveness of yoga on cancer-related fatigue: a systematic review and meta-analysis. Oncol Nurs Forum 48(2):207–228. https://doi.org/10.1188/21.ONF.207-228
Tomlinson D, Diorio C, Beyene J, Sung L (2014) Effect of exercise on cancer-related fatigue: a meta-analysis. Am J Phys Med Rehabil 93:675–686
Buffart LM, van Uffelen JGZ, Riphagen II et al (2012) Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer 12:1–21
Easwaran K, Gopalasingam Y, Green DD et al (2021) Effectiveness of Tai Chi for health promotion for adults with health conditions: a scoping review of Meta-analyses. Disabil Rehabil 43:2978–2989. https://doi.org/10.1080/09638288.2020.1725916
Jiang M, Ma Y, Yun B et al (2020) Exercise for fatigue in breast cancer patients: an umbrella review of systematic reviews. Int J Nurs Sci 7:248–254. https://doi.org/10.1016/j.ijnss.2020.03.001
Huang J, Liu H, Chen J et al (2021) The effectiveness of Tai Chi in patients with breast cancer: an overview of systematic reviews and meta-analyses. J Pain Symptom Manag 61:1052–1059. https://doi.org/10.1016/j.jpainsymman.2020.10.007
Olsson Möller U, Beck I, Rydén L, Malmström M (2019) A comprehensive approach to rehabilitation interventions following breast cancer treatment - a systematic review of systematic reviews. BMC Cancer 19:1–20. https://doi.org/10.1186/s12885-019-5648-7
Huang J, Liu H, Chen J et al (2021) The effectiveness of Tai Chi in patients with breast cancer: an overview of systematic reviews and meta-analyses. J Pain Symptom Manage 61:1052–1059. https://doi.org/10.1016/j.jpainsymman.2020.10.007
Pj K, Baumgarden J, Schneider R et al (2019) Qigong and Tai Chi as therapeutic exercise: survey of systematic reviews and meta-analyses addressing physical health conditions. Altern Ther Heal Med 25:48–53
Yildiz Kabak V, Gursen C, Aytar A et al (2021) Physical activity level, exercise behavior, barriers, and preferences of patients with breast cancer–related lymphedema. Support Care Cancer 29:3593–3602. https://doi.org/10.1007/s00520-020-05858-3
Sattar S, Haase KR, Bradley C et al (2021) Barriers and facilitators related to undertaking physical activities among men with prostate cancer: a scoping review. Prostate Cancer Prostatic Dis 24:1007–1027. https://doi.org/10.1038/s41391-021-00399-0
Frikkel J, Götte M, Beckmann M et al (2020) Fatigue, barriers to physical activity and predictors for motivation to exercise in advanced cancer patients. BMC Palliat Care 19:1–11. https://doi.org/10.1186/s12904-020-00542-z
Lavallée JF, Abdin S, Faulkner J, Husted M (2019) Barriers and facilitators to participating in physical activity for adults with breast cancer receiving adjuvant treatment: a qualitative metasynthesis. Psychooncology 28:468–476. https://doi.org/10.1002/pon.4980
Wong J, McAuley E, Trinh L (2018) Physical activity programming and counseling preferences among cancer survivors: a systematic review. Int J Behav Nutr Phys Act 15(1):48. https://doi.org/10.1186/s12966-018-0680-6
Dipietro L, Campbell WW, Buchner DM et al (2019) Physical activity, injurious falls, and physical function in aging: an umbrella review. Med Sci Sports Exerc 51:1303–1313. https://doi.org/10.1249/MSS.0000000000001942
Cuenca-Martínez F, Calatayud J, Suso-Martí L, et al (2022) Behavior modification techniques on patients with chronic pain in the context of COVID-19 telerehabilitation: an umbrella review. Int J Environ Res Public Health 19:. https://doi.org/10.3390/ijerph19095260
Torres A, Tennant B, Ribeiro-Lucas I et al (2018) Umbrella and systematic review methodology to support the 2018 physical activity guidelines advisory committee. J Phys Act Health 15:805–810. https://doi.org/10.1123/jpah.2018-0372
Cuenca-Martínez F, La Touche R, Varangot-Reille C et al (2022) Effects of neural mobilization on pain intensity, disability, and mechanosensitivity: an umbrella review with meta-meta-analysis. Phys Ther. https://doi.org/10.1093/ptj/pzac040
Granholm A, Alhazzani W, Møller MH (2019) Use of the GRADE approach in systematic reviews and guidelines. Br J Anaesth 123:554–559
Hoffmann TC, Glasziou PP, Boutron I et al (2014) Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 348:g1687. https://doi.org/10.1136/bmj.g1687
Whiting P, Savović J, Higgins JPT et al (2016) ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol 69:225–234. https://doi.org/10.1016/j.jclinepi.2015.06.005
Swierz MJ, Storman D, Zajac J et al (2021) Similarities, reliability and gaps in assessing the quality of conduct of systematic reviews using AMSTAR-2 and ROBIS: systematic survey of nutrition reviews. BMC Med Res Methodol 21:261. https://doi.org/10.1186/s12874-021-01457-w
Author information
Authors and Affiliations
Contributions
MJMF is the guarantor and conceived the study. MJCH, MJMF, and JMC wrote the first draft of the protocol and manuscript. MJCH conducted article screening. JMC extracted data. JMC and MJCH assisted in interpreting the data. AMHR, JMC, and PGG conducted data analysis. All authors contributed importantly to the content and style of the protocol and manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. This study does not involve human participants.
Consent for publication
Not applicable.
Competing interests
None.
Provenance and peer review
Not commissioned; externally peer-reviewed.
Disclaimer
This content has been supplied by the authors. It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the authors and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Casuso-Holgado, M.J., Heredia-Rizo, A.M., Gonzalez-Garcia, P. et al. Mind–body practices for cancer-related symptoms management: an overview of systematic reviews including one hundred twenty-nine meta-analyses. Support Care Cancer 30, 10335–10357 (2022). https://doi.org/10.1007/s00520-022-07426-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07426-3