Abstract
Purpose
Communication between patients and professionals is one major aspect of the support offered to cancer patients. The European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Group (QLG) has developed a cancer-specific instrument for the measurement of different issues related to the communication between cancer patients and their health care professionals.
Methods
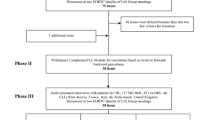
Questionnaire development followed the EORTC QLG Module Development Guidelines. A provisional questionnaire was pre-tested (phase III) in a multicenter study within ten countries from five cultural areas (Northern and South Europe, UK, Poland and Taiwan). Patients from seven subgroups (before, during and after treatment, for localized and advanced disease each, plus palliative patients) were recruited. Structured interviews were conducted. Qualitative and quantitative analyses have been performed.
Results
One hundred forty patients were interviewed. Nine items were deleted and one shortened. Patients’ comments had a key role in item selection. No item was deleted due to just quantitative criteria. Consistency was observed in patients’ answers across cultural areas. The revised version of the module EORTC QLQ-COMU26 has 26 items, organized in 6 scales and 4 individual items.
Conclusions
The EORTC COMU26 questionnaire can be used in daily clinical practice and research, in various patient groups from different cultures. The next step will be an international field test with a large heterogeneous group of cancer patients.
Similar content being viewed by others
References
Moore PM, Rivera Mercado S, Grez Artigues M, Lawrie TA (2013) Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev Mar 28:3
American Society of Clinical Oncology (1998) Cancer care during the last phase of life. J Clin Oncol 16:1986–1996
Committeee on Cancer Survivorship, Institute of Medicine (2006) From cancer patient to cancer survivor: lost in transition. National Academics of Sciences, Washington
Institute of Medicine (2001) Crossing the quality chasm: a new health system for the 21st century. National Academy Press, Washington, DC
De Vries AM, de Roten Y, Meystre C, Passchier J, Despland JN, Stiefel F (2014) Clinician characteristics, communication, and patient outcome in oncology: a systematic review. Psychooncology 23:375–381
Ansmann L, Kowalski C, Ernstmann N, Ommen O, Pfaff H (2012) Patients’ perceived support from physicians and the role of hospital characteristics. Int J Qual Health Care 24:501–508
Epstein AS, Morrison RS (2012) Palliative oncology: identity, progress, and the path ahead. Ann Oncol 23:43–48
Fallowfield L (2009) The challenge of interacting with patients in oncology. Eur J Cancer 45:445–446
Stewart M, Belle Brown J, Hammerton J, Donner A, Gavin A, Holliday RL, Whelan T, Leslie K, Cohen I, Weston W, Freeman T (2007) Improving communication between doctors and breast cancer patients. Ann Fam Med 5:387–394
Ong LM, Visser MR, Lammes FB, de Haes JC (2000) Doctor-patient communication and cancer patients’ quality of life and satisfaction. Patient Educ Couns 41:145–156
Neumann M, Wirtz M, Bollschweiler E, Mercer SW, Warm M, Wolf J, Pfaff H (2007) Determinants and patient-reported long-term outcomes of physician empathy in oncology: a structural equation modelling approach. Patien Educ Couns 69:63–75
Trudel TG, Leduc N, Dumont S (2014) Perceived communication between physicians and breast cancer patients as a predicting factor of patients’ health-related quality of life: a longitudinal analysis. Psychooncology 23:531–538
Farin E, Nagl M (2013) The patient-physician relationship in patients with breast cancer: influence on changes in quality of life after rehabilitation. Qual Life Res 22:283–294
Fallowfield L, Jenkins V (2004) Communicating sad, bad, and difficult news in medicine. Lancet 363:312–319
Street RL Jr, Elwyn G, Epstein RM (2012) Patient preferences and healthcare outcomes: an ecological perspective. Expert Rev Pharmacoecon Outcomes Res 12:167–180
Carlson LE, Feldman-Stewart D, Tishelman C, Brundage MD, SCRN Communication Team (2005) Patient-professional communication research in cancer: an integrative review of research methods in the context of a conceptual framework. Psychooncology 14:812–828
Feldman-Stewart D, Brundage MD, Tishelman C, SCRN Communication Team (2005) A conceptual framework for patient-professional communication: an application to the cancer context. Psychooncology 14:801–809
Morgan M (2008) The doctor–patient relationship. In: Scambler G (ed) Sociology as applied to medicine. Saunders/Elsevier, Edinburgh, pp 49–65
Institute of Medicine (2001) Crossing the quality chasm: a new health system for the 21st century. National Academy Press, Washington
Epstein RM, Street RL Jr (2007) Patient-centered communication in cancer care: promoting healing and reducing suffering. National Cancer Institute, Bethesda, MD, USA
Surbone A (2008) Cultural aspects of communication in cancer care. Support Care Cancer 16:235–240
Epstein RM, Franks P, Fiscella F, Shields CG, Meldrum SC, Kravitz RL, Duberstein PR (2005) Measuring patient-centered communication in patient–physician consultations: theoretical and practical issues. Soc Sci Med 61:1516–1528
Lawson MT (2002) Nurse practitioner and physician communication styles. Appl Nurs Res 15:60–66
Iasevoli M, Giantin V, Voci A, Valentini E, Zurlo A, Maggi S, Siviero P, Orrù G, Crepaldi G, Pegoraro R, Manzato E (2012) Discussing end-of-life care issues with terminally ill patients and their relatives: comparisons among physicians, nurses and psychologists. Aging Clin Exp Res 24:35–42
Arraras JI, Greimel E, Sezer O, Chie WC, Bergenmar M, Costantini A, Young T, Vlasic KK, Velikova G (2010) An international validation study of the EORTC QLQ-INFO25 questionnaire: an instrument to assess the information given to cancer patients. Eur J Cancer 46:2726–2738
Johnson C, Aaronson N, Blazeby J, Bottomley A, Fayers P, Koller M, Kuliś D, Ramage J, Sprangers M, Velikova G, Young T (2011) EORTC Quality of Life Group module development guidelines, fourth edn. EORTC QL Group, Brussels
Arraras JI, Kuljanic K, Sztankay M, Wintner LM, Costantini A, Chie WC, Liavaag AH, Greimel E, Bredart A, Arnott M, Young T, Koller M (2015) Initial phases in the development of a European Organisation for Research and Treatment of Cancer communication-specific module. Psychooncology 24:236–240
Cull A, Sprangers M, Bjordal K, Johnson C, Scott N, BottomleyA (2002) EORTC Quality of Life Group translation procedure, second edn. EORTC, Brussels
Costantini A, Baile WF, Lenzi R, Costantini M, Ziparo V, Marchetti P, Grassi L (2009) Overcoming cultural barriers to giving bad news: feasibility of training to promote truth-telling to cancer patients. J Cancer Educ 24:180–185
Arraras JI, Greimel E, Chie WC, Sezer O, Bergenmar M, Costantini A, Young T, Vlasic KK, Velikova G, European Organisation for Research, Treatment of Cancer Quality of Life Group (2013) Cross-cultural differences in information disclosure evaluated through the EORTC questionnaires. Psychooncology 22:268–275
Mazor KM, Beard RL, Alexander GL, Arora NK, Firneno C, Gaglio B, Greene SM, Lemay CA, Robinson BE, Roblin DW, Walsh K, Street RL Jr, Gallagher TH (2013) Patients’ and family members’ views on patient-centered communication during cancer care. Psychooncology 22:2487–2495
Hack T (2005) Psycho-oncology special issue on communication. Psychooncology 14:797–798
Arraras JI, Wright S, Greimel E, Holzner B, Kuljanic-Vlasic K, Velikova G, Eisemann M, Visser A, EORTC Quality of Life Group (2004) Development of a questionnaire to evaluate the information needs of cancer patients: the EORTC questionnaire. Patient Educ Coun 54:235–241
Tobin GA (2012) Breaking bad news: a phenomenological exploration of Irish nurses’ experiences of caring for patients when a cancer diagnosis is given in an acute care facility (part 1). Cancer Nurs 35:E21–E29
Eid A, Petty M, Hutchins L, Thompson R (2009) “Breaking bad news”: standardized patient intervention improves communication skills for hematology-oncology fellows and advanced practice nurses. J Cancer Educ 24:154–159
Wuensch A, Tang T, Goelz T, Zhang Y, Stubenrauch S, Song L, Hong Y, Zhang H, Wirsching M, Fritzsche K (2013) Breaking bad news in China—the dilemma of patients’ autonomy and traditional norms. A first communication skills training for Chinese oncologists and caretakers. Psychooncology 22:1192–1195
Mauri E, Vegni E, Lozza E, Parker PA, Moja EA (2009) An exploratory study on the Italian patients’ preferences regarding how they would like to be told about their cancer. Support Care Cancer 17:1523–1530
Acknowledgments
The study was supported by grants from EORTC Quality of Life Group (grant number EORTC QLG 006/2012) and the Instituto de Salud Carlos III (Spain) (grant number PI12-02293) that supported the collection of the data.
The work of L. M. W. and M. S. was supported by the Austrian National Bank (ÖNB, project number 14492) and the Austrian Science Fund (FWF, grant number P26930).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
The protocol was approved by local ethical committees according to national requirements and followed the Declaration of Helsinki of 1975, as revised in 2008.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Arraras, J.I., Wintner, L.M., Sztankay, M. et al. EORTC QLQ-COMU26: a questionnaire for the assessment of communication between patients and professionals. Phase III of the module development in ten countries. Support Care Cancer 25, 1485–1494 (2017). https://doi.org/10.1007/s00520-016-3536-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3536-0