Abstract
Background
Hyperparathyroidism persists in up to 50% of pediatric kidney transplant recipients. The aims of this study were to describe the evolution of parathyroid hormone (PTH) in the first year after transplantation and to identify factors associated with hyperparathyroidism.
Methods
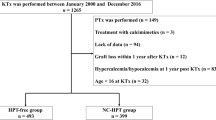
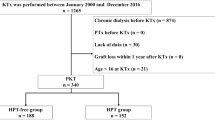
This retrospective study included children who underwent kidney transplantation at the University Hospitals of Ghent, Leuven, Rotterdam, or Amsterdam. Data from 149 patients were collected before and up to 12 months after transplantation. Severe hyperparathyroidism was defined as PTH 2-fold above the reference value. Factors associated with hyperparathyroidism and severe hyperparathyroidism were identified using multivariate logistic regression analysis.
Results
Before transplantation, 97 out of 137 patients (71%) had hyperparathyroidism. The probability of hyperparathyroidism and severe hyperparathyroidism declined from 0.49 and 0.17 to 0.29 and 0.09 at 3 and 12 months after transplantation, respectively. BMI SDS (β: 0.509; p = 0.011; 95% CI: 1.122–2.468), eGFR (β: − 0.227; p = 0.030; 95% CI: 0.649–0.978), and pre-transplant hyperparathyroidism (β: 1.149; p = 0.039; 95% CI: 1.062–9.369) were associated with hyperparathyroidism 12 months after transplantation. Pre-transplant hyperparathyroidism (β: 2.115; p = 0.044; 95% CI: 1.055–65.084), defined as intact parathormone (iPTH) levels > 65 ng/l (6.9 pmol/l) or 1-84 PTH > 58 ng/l (6.2 pmol/l), was associated with severe hyperparathyroidism at 3 months. Only eGFR (β: − 0.488; p = 0.010; 95% CI: 0.425–0.888) was inversely associated with severe hyperparathyroidism at 9 months after transplantation.
Conclusions
Allograft function remains the main determinant of severe hyperparathyroidism after transplantation. Our findings emphasize the importance of BMI and pre-transplant PTH control.



Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CKD:
-
Chronic kidney disease
- CKD-MBD:
-
Chronic kidney and disease-mineral and bone isorder
- CKiD:
-
Chronic kidney disease in children
- CI:
-
Confidence interval
- eGFR:
-
Estimated glomerular filtration rate
- FGF-23:
-
Fibroblast growth factor-23
- IQR:
-
Inter quartile range
- iPTH:
-
intact Parathormone
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- PTH:
-
Parathyroid hormone
- SDS:
-
Standard deviation score
- UNL:
-
Upper limit of normal range
- 25(OH)D:
-
25-Hydroxyvitamin D
References
Di Lullo L, House A, Gorini A, Santoboni A, Russo D, Ronco C (2015) Chronic kidney disease and cardiovascular complications. Heart Fail Rev 20:259–272
Falkiewicz K, Bidzinska B, Demissie M, Boratynska M, Zmonarski SC, Tworowska K, Klinger M, Milewicz A, Patrzalek D (2005) Influence of vitamin D receptor gene polymorphisms on secondary hyperparathyroidism and bone density after kidney transplantation. Transplant Proc 37:1023–1025
Guzzo I, Di Zazzo G, Laurenzi C, Rava L, Giannone G, Picca S, Dello Strologo L (2011) Parathyroid hormone levels in long-term renal transplant children and adolescents. Pediatr Nephrol 26:2051–2057
Matsuda-Abedini M, Portale AA, Shah A, Neuhaus J, McEnhill M, Mathias RS (2006) Persistent secondary hyperparathyroidism after renal transplantation in children. Pediatr Nephrol 21:413–418
Lou I, Foley D, Odorico SK, Leverson G, Schneider DF, Sippel R, Chen H (2015) How well does renal transplantation cure hyperparathyroidism? Ann Surg 262:653–659
Wesseling-Perry K, Tsai EW, Ettenger RB, Juppner H, Salusky IB (2011) Mineral abnormalities and long-term graft function in pediatric renal transplant recipients: a role for FGF-23? Nephrol Dial Transplant 26:3779–3784
Arbeiter AK, Buscher R, Petersenn S, Hauffa BP, Mann K, Hoyer PF (2009) Ghrelin and other appetite-regulating hormones in paediatric patients with chronic renal failure during dialysis and following kidney transplantation. Nephrol Dial Transplant 24:643–646
Dura-Trave T, Gallinas-Victoriano F, Chueca-Guindulain MJ, Berrade-Zubiri S, Urretavizcaya-Martinez M, Ahmed-Mohamed L (2019) Assessment of vitamin D status and parathyroid hormone during a combined intervention for the treatment of childhood obesity. Nutr Diabetes 9:18
Hu X, Ma X, Luo Y, Xu Y, Xiong Q, Pan X, Xiao Y, Bao Y, Jia W (2018) Associations of serum fibroblast growth factor 23 levels with obesity and visceral fat accumulation. Clin Nutr 37:223–228
Shroff R, Knott C, Gullett A, Wells D, Marks SD, Rees L (2011) Vitamin D deficiency is associated with short stature and may influence blood pressure control in paediatric renal transplant recipients. Pediatr Nephrol 26:2227–2233
Tuchman S, Kalkwarf HJ, Zemel BS, Shults J, Wetzsteon RJ, Foerster D, Strife CF, Leonard MB (2010) Vitamin D deficiency and parathyroid hormone levels following renal transplantation in children. Pediatr Nephrol 25:2509–2516
Courbebaisse M, Thervet E, Souberbielle JC, Zuber J, Eladari D, Martinez F, Mamzer-Bruneel MF, Urena P, Legendre C, Friedlander G, Prie D (2009) Effects of vitamin D supplementation on the calcium-phosphate balance in renal transplant patients. Kidney Int 75:646–651
Prytula A, Cransberg K, Raes A (2017) CYP3A4 is a crosslink between vitamin D and calcineurin inhibitors in solid organ transplant recipients: implications for bone health. Pharm J 17:481–487
Prytula A, Cransberg K, Raes A (2019) Drug-metabolizing enzymes CYP3A as a link between tacrolimus and vitamin D in renal transplant recipients: is it relevant in clinical practice? Pediatr Nephrol 34:1201–1210
Uslu Gokceoglu A, Comak E, Dogan CS, Koyun M, Akbas H, Akman S (2014) Magnesium excretion and hypomagnesemia in pediatric renal transplant recipients. Ren Fail 36:1056–1059
Haffner D, Leifheit-Nestler M (2019) CKD-MBD post kidney transplantation. Pediatr Nephrol. https://doi.org/10.1007/s00467-019-04421-5
Van de Cauter J, Sennesael J, Haentjens P (2011) Long-term evolution of the mineral metabolism after renal transplantation: a prospective, single-center cohort study. Transplant Proc 43:3470–3475
Lau WL, Obi Y, Kalantar-Zadeh K (2018) Parathyroidectomy in the management of secondary hyperparathyroidism. Clin J Am Soc Nephrol 13:952–961
Jenabi A, Jabbari M, Ziaie H (2017) Comparing the values of intact parathormone and 1- 84 PTH to predict hyperparathyroidism in hemodialysis patients. J Nephropathol 6:248–253
Wang AY, Akizawa T, Bavanandan S, Hamano T, Liew A, Lu KC, Lumlertgul D, Oh KH, Zhao MH, Ka-Shun Fung S, Obi Y, Sumida K, Choong LHL, Goh BL, Hao CM, Kwon YJ, Tarng DC, Zuo L, Wheeler DC, Tsukamoto Y, Fukagawa M (2019) 2017 Kidney Disease: Improving Global Outcomes (KDIGO) Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) guideline update implementation: Asia Summit Conference Report. Kidney Int Rep 4:1523–1537
Kovacevic B, Ignjatovic M, Zivaljevic V, Cuk V, Scepanovic M, Petrovic Z, Paunovic I (2012) Parathyroidectomy for the attainment of NKF-K/DOQI™ and KDIGO recommended values for bone and mineral metabolism in dialysis patients with uncontrollable secondary hyperparathyroidism. Langenbeck's Arch Surg 397:413–420
Schwartz GJ, Schneider MF, Maier PS, Moxey-Mims M, Dharnidharka VR, Warady BA, Furth SL, Munoz A (2012) Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int 82:445–453
Filler G, Lee M (2018) Educational review: measurement of GFR in special populations. Pediatr Nephrol 33:2037–2046
Ref. 1-20050604-NP/2-20/F v, kul © (2004) Groeicurve meisjes (2 - 20 jaar)
Ref. 1-20050604-NP/2-20/M v, kul © (2005) Groeicurve jongens (2 - 20 jaar)
TNO (2010) Groeidiagram meisjes 1-21 jaar Vijfde landelijke groeistudie
TNO (2010) Groeidiagram Jongens 1-21 jaar. Vijfde Landelijke Groeistudie
Flegal KM, Tabak CJ, Ogden CL (2006) Overweight in children: definitions and interpretation. Health Educ Res 21:755–760
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320:1240–1243
Bonthuis M, Busutti M, van Stralen KJ, Jager KJ, Baiko S, Bakkaloglu S, Battelino N, Gaydarova M, Gianoglio B, Parvex P, Gomes C, Heaf JG, Podracka L, Kuzmanovska D, Molchanova MS, Pankratenko TE, Papachristou F, Reusz G, Sanahuja MJ, Shroff R, Groothoff JW, Schaefer F, Verrina E (2015) Mineral metabolism in European children living with a renal transplant: a European society for paediatric nephrology/european renal association-European dialysis and transplant association registry study. Clin J Am Soc Nephrol 10:767–775
Kim DH, Lee JH, Han DJ, Park YS (2018) Risk factors for persistent hyperparathyroidism in children with stable renal function after kidney transplantation. Pediatr Transplant. https://doi.org/10.1111/petr13238
Ketteler M, Block GA, Evenepoel P, Fukagawa M, Herzog CA, McCann L, Moe SM, Shroff R, Tonelli MA, Toussaint ND, Vervloet MG, Leonard MB (2017) Executive summary of the 2017 KDIGO Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) guideline update: what’s changed and why it matters. Kidney Int 92:26–36
Hu MC, Shiizaki K, Kuro-o M, Moe OW (2013) Fibroblast growth factor 23 and Klotho: physiology and pathophysiology of an endocrine network of mineral metabolism. Annu Rev Physiol 75:503–533
Haffner D, Schuler U (2014) Metabolic bone disease after renal transplantation. Curr Opin Pediatr 26:198–206
Wesseling-Perry K, Pereira RC, Tsai E, Ettenger R, Juppner H, Salusky IB (2013) FGF23 and mineral metabolism in the early post-renal transplantation period. Pediatr Nephrol 28:2207–2215
Ladhani M, Lade S, Alexander SI, Baur LA, Clayton PA, McDonald S, Craig JC, Wong G (2017) Obesity in pediatric kidney transplant recipients and the risks of acute rejection, graft loss and death. Pediatr Nephrol 32:1443–1450
Kaur K, Jun D, Grodstein E, Singer P, Castellanos L, Teperman L, Molmenti E, Fahmy A, Frank R, Infante L, Sethna CB (2018) Outcomes of underweight, overweight, and obese pediatric kidney transplant recipients. Pediatr Nephrol 33:2353–2362
Reinehr T, de Sousa G, Alexy U, Kersting M, Andler W (2007) Vitamin D status and parathyroid hormone in obese children before and after weight loss. Eur J Endocrinol 157:225–232
Roy B, Curtis ME, Fears LS, Nahashon SN, Fentress HM (2016) Molecular mechanisms of obesity-induced osteoporosis and muscle atrophy. Front Physiol 7:439
Nogueira PC, Rey N, Said MH, Cochat P (1997) Evolution of hyperparathyroidism after renal transplantation in children--effect of pre-emptive transplantation and duration of dialysis. Nephrol Dial Transplant 12:984–987
Hasegawa K, Motoyama O, Shishido S, Aikawa A (2019) Mineral disorders in pediatric pre-emptive kidney transplantation. Pediatr Int 61:587–594
Nakai K, Fujii H, Ishimura T, Fujisawa M, Nishi S (2017) Incidence and risk factors of persistent hyperparathyroidism after kidney transplantation. Transplant Proc 49:53–56
Cunningham J, Locatelli F, Rodriguez M (2011) Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol 6:913–921
Vetter T, Lohse MJ (2002) Magnesium and the parathyroid. Curr Opin Nephrol Hypertens 11:403–410
Preka E, Wan M, Price KL, Long DA, Aitkenhead H, Shroff R (2020) Free 25-hydroxyvitamin-D concentrations are lower in children with renal transplant compared with chronic kidney disease. Pediatr Nephrol 35:1069–1079
Harambat J, Kunzmann K, Azukaitis K, Bayazit AK, Canpolat N, Doyon A, Duzova A, Niemirska A, Sozeri B, Thurn-Valsassina D, Anarat A, Bessenay L, Candan C, Peco-Antic A, Yilmaz A, Tschumi S, Testa S, Jankauskiene A, Erdogan H, Rosales A, Alpay H, Lugani F, Arbeiter K, Mencarelli F, Kiyak A, Donmez O, Drozdz D, Melk A, Querfeld U, Schaefer F (2017) Metabolic acidosis is common and associates with disease progression in children with chronic kidney disease. Kidney Int 92:1507–1514
Verghese PS (2017) Pediatric kidney transplantation: a historical review. Pediatr Res 81:259–264
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vanderstraeten, K., De Pauw, R., Knops, N. et al. Body mass index is associated with hyperparathyroidism in pediatric kidney transplant recipients. Pediatr Nephrol 36, 977–986 (2021). https://doi.org/10.1007/s00467-020-04796-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04796-w