Abstract
Wide ranges of age and weight in pediatric patients makes renal replacement therapy (RRT) in acute kidney injury (AKI) challenging, particularly in the pediatric intensive care unit (PICU), wherein children are often hemodynamically unstable. Standard hemodialysis (HD) is difficult in this group of children and continuous veno-venous hemofiltration/dialysis (CVVH/D) has been the accepted modality in the developed world. Unfortunately, due to cost constraints, CVVH/D is often not available and peritoneal dialysis (PD) remains the common mode of RRT in resource-poor facilities. Acute PD has its drawbacks, and intermittent HD (IHD) done slowly over a prolonged period has been explored as an alternative. Various modes of slow sustained IHD have been described in the literature with the recently introduced term prolonged intermittent RRT (PIRRT) serving as an umbrella terminology for all of these modes. PIRRT has been widely accepted in adults with studies showing it to be as effective as CVVH/D but with an added advantage of being more cost-effective. Pediatric data, though scanty, has been promising. In this current review, we elaborate on the practical aspects of undertaking PIRRT in children as well as summarize its current status.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI) continues to contribute significantly towards morbidity and mortality in critically ill children and there has been an ongoing intense search to identify any early interventions [1]. Recent trials have generated some evidence in favor of avoidance of fluid overload as well as early initiation of renal replacement therapy (RRT) in reducing mortality [2,3,4]. AKI in pediatric intensive care units (PICU) is often secondary to sepsis/shock and these children are usually hypotensive and on various types of vasopressor support despite being fluid overloaded [3, 5]. Standard extra-corporeal RRT such as conventional intermittent hemodialysis (IHD) in this subgroup of AKI can be problematic since it is likely to aggravate hypotension and precipitate catastrophic events [5,6,7]. Peritoneal dialysis (PD), although feasible even among hemodynamically unstable patients [8], does have its drawbacks [9,10,11]. There is the theoretical risk of intra-peritoneal distention and worsening of ventilation parameters among ventilated children, although clinical evidence has been contrasting [11,12,13,14]. Moreover, unlike HD, one cannot control the rate of ultra-filtration in PD, which can be erratic [8,9,10]. Hence, continuous veno-venous hemofiltration/dialysis (CVVH/D) has been preferred, especially in developed countries, for a slow but continuous mode of extra-corporeal RRT [2, 15,16,17]. Unfortunately, CVVH/D requires expensive sophisticated machines and consumables, trained staff, and is usually very labor intensive. Hybrid therapies providing RRT over an extended period but on an intermittent basis (prolonged intermittent RRT i.e., PIRRT) using standard HD machines has been envisaged to include the best of both these worlds, i.e., slow sustained modality of CVVH/D ensuring hemodynamic stability and better biochemical clearance along with cost-effectiveness of conventional IHD (Table 1). Although evidence has accumulated in its favor, this has primarily been among adults, with pediatric literature still scanty [18,19,20,21,22,23,24,25,26,27]. In this review, we aim to summarize the current status of PIRRT with a focus on children.
Definition of prolonged intermittent renal replacement therapy (PIRRT)
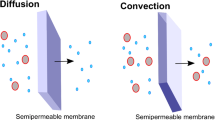
Broadly speaking, any extracorporeal mode of RRT given intermittently over a prolonged session (i.e., ≥6 h) can be defined as PIRRT [28]. Hence the original description of hemodialysis by Kolff (duration = 690 min, blood flow of 116 ml/min) could be described as the initial PIRRT [29, 30]. Subsequent development in the field of HD saw the acceptance of standard IHD as 3–4 h duration with a high blood flow (Qb) and dialysate flow (Qd). The concept of hybrid therapy combining the efficiency of HD and the hemodynamic stability of CVVH was re-explored by Kudoh in 1988 (slow continuous HD), and after its use by Schlaeper et al. among a cohort of critically ill adults, it has become quite in vogue [31,32,33]. Thereafter, various modifications in dialysis prescription have been undertaken, primarily influenced by available machines and the dialysis unit requirements, such as the type of case loads encountered, resource needs, and available expertise. Table 2 explains the multiple terminologies in use describing the hybrid varieties of extra-corporeal RRT. The use of PIRRT as an umbrella terminology describing both diffusive and or convective methods of extended extra-corporeal blood purification is becoming the accepted norm. In this review, the term PIRRT and sustained low-efficiency HD (SLED) will be used interchangeably. Although the duration has been fixed as ≥6 h, rate of Qb and Qd can be variable. Overall Qb is usually ≤5 ml/kg/min and Qd ≤ twice the Qb. Lack of a rigid definition is often construed as a major disadvantage but can be in fact advantageous in its flexibility both in terms of duration and intensity, which can be adjusted as per patient requirement and the HD unit’s capability.
Indications for PIRRT
Indications for initiating RRT in a pediatric intensive care unit (PICU) are varied and include [43, 44]:
-
Non-obstructive oliguria with fluid overload 10% above baseline.
-
Refractory metabolic acidosis or hyperkalemia
-
Uremic organ involvement (pericarditis, encephalopathy, neuropathy, myopathy)
-
Severe refractory dysnatremia (Na+ > 160 or <115 meq/l)
-
Overdose with a dialyzable drug
-
Neonatal hyperammonemia and other inborn errors of metabolism
-
Coagulopathy requiring large amounts of blood products in patients at risk of pulmonary edema or acute respiratory distress syndrome (ARDS)
-
Refractory edema not responding to high-dose diuretics.
The uniqueness of children admitted to the ICU does influence the choice of mode of RRT. Critically ill children usually end up having a high obligatory fluid requirement due to hyper-catabolic state. Other reasons are the need for blood products to combat co-existing coagulopathy and multiple antibiotics and inotrope infusions. In the presence of oliguria/anuria, administering a high volume of intravenous fluid is likely to precipitate pulmonary edema. This mandates removal of fluid by RRT (ultrafiltration (UF)), but is challenging as these children are often hypotensive and on multiple vasopressor support. The hemodynamic advantage of CVVH/D over IHD has been attributed to a slower UF rate, as the same UF goal is achieved over 24 h instead of the standard 3–4 h. PIRRT also has a similar advantage but at a lower cost [18,19,20,21,22,23,24,25,26,27]. Additionally, unlike CVVH/D, PIRRT allows sufficient time for any ancillary procedures/treatments such as imaging or surgical interventions. The choice of PIRRT or CVVH/D is also influenced by availability of CVVH/D machines and trained staff, as well as cost implications. As evidenced by various reports primarily consisting of adult studies, PIRRT can be used as the initial modality as well as in transition from CVVH/D to IHD once the patient is stable enough to discontinue CVVH/D, but still not sufficiently hemodynamically stable to sustain IHD [13,14,15,16,17]. Although PIRRT is still not the primary mode of RRT, surveys have pointed to it being increasingly acknowledged as a feasible mode of dialysis in the adult ICU [45,46,47,48].
Dialysis setup required for PIRRT
The setup for PIRRT is classically similar to IHD with some modification to the HD machine.
Machines for PIRRT
The prerequisite for performing PIRRT is the ability to extend the dialysis session length beyond the conventional 4–5 h of IHD and the ability to vary the Qb and Qd. Hence, any machine with the ability to lower the Qb/Qd and increase the duration of HD can be used for PIRRT. Traditionally, the same machines used for IHD have been tweaked to cater for PIRRT to make it cost-effective. In fact, in a busy HD unit it may be economical to use the same machine for maintenance IHD during daytime and for PIRRT overnight. Unfortunately, few HD machines are able to provide the low range of Qb/Qd, which are often required for critically ill hemodynamically unstable small children. Fresenius Medical Care Company has been the pioneer in marketing HD machines with additional specification for PIRRT. These machines can be classified as single pass (uses dialysate generated online from reverse osmosis purified water and bicarbonate proportioning system) or batch machine (dialysate generated from prepackaged salts and sterile water that is stored in the machine). The single-pass machines such as the 2008, 4008, and now 5008 series, or the batch dialysate machine such as the Genius machine, have been used worldwide [20, 38,39,40,41,42].
The advantages of batch dialysate machines include: user friendliness, ultrapure dialysate, and no need for on-the-spot water purification, as access to ultrapure water (required for high flux dialyzers and hemodiafiltration) is available in a limited number of ICUs. The Genius (batch dialysate) machine utilizes a dual-headed roller pump for both blood and dialysate flow; hence the ratio of Qb/Qd is 1 with this machine. The dialysate is contained in a 75- or 90-l jacketed tank to maintain thermal stability; fresh dialysate, which has a lower specific gravity, is drawn from the top of the tank while spent dialysate with a higher specific gravity is discharged into the bottom of the tank. An ultraviolet tube is located in the center of the tank to prevent bacterial contamination and growth. The machine requires dedicated tubing sets, which do not have a bubble chamber. This avoids an air–blood interface and decreases clotting risk. Using a flow of 70 ml/min and a 75-l dialysate tank, a session of 18 h can be carried out with a single batch of dialysate. A separate ultrafiltration pump removes a portion of the dialysate from the closed loop into a separate receptacle.
Single-pass machines from various manufacturers have been more frequently utilized for PIRRT, and a comparison of some of the commonly available machines is shown in Table 3. The ArrT plus 5008 series, the AK200 Ultra machines, and the ARTIS machine possess additional unique features of cold sterilization or ultrafiltration of the dialysate, which results in a 4-log reduction of bacteria and a 2-log reduction in endotoxin, producing a sterile, pyrogen-free fluid suitable for intravenous infusion. This enables them to add convection clearance (though not allowed in the United States of America) to the predominant diffusion clearance of standard HD machines. This has been described as sustained low-efficiency daily diafiltration (SLEDD-f). They do require ultrapure water and sterile dry powder concentrates for the dialysate preparation. High flux dialyzers or hemo-filters from the AV 600 series, having UF coefficients >20 ml/mmHg/h, are required for this treatment. At least a part of the replacement fluid should be delivered pre-filter and the blood flow has to be proportionally higher than usual in order to avoid a filtration fraction >20%. Giving part of the replacement fluid pre filter reduces the viscosity of the fluid caused by the high ultrafiltration rates and therefore decreases the chances of filter clotting. The volume of fluid required is higher with pre-dilution but not necessarily so when only a part of it is given pre filter. Moreover, as the fluid is prepared online, cost is not a major issue (around USD 0.14 per liter in an Indian center). Blood flow needs to be higher in post- as compared to pre-dilution replacement in order not to exceed the chosen filtration fraction.
Prerequisites for performing SLEDD-f:
-
1.
Sterile dry powder concentrates (Bicart and Bibag): This has replaced the liquid bicarbonate concentrate, which traditionally predisposes to bacterial growth. The acid concentrate is also a powder or a liquid with a low pH, depending on the configuration of the machine.
-
2.
Ultrapure water: This is generated by either a system in the ICU or a portable reverse osmosis (RO) system. The European Union (EU) standard of ultrapure water (bacterial count of 0.1 cfu/ml and an endotoxin level of 0.03 EU /ml) needs to be consistently maintained. Several systems have been utilized to provide this, including double-pass (RO) and an electro-deionizer or an ultrafiltration system online. The important feature of any system is elimination of a storage tank and a frequent disinfection cycle at least daily, preferably with heat.
-
3.
Cold sterilization or controlled ultrafiltration: This technology pioneered by Gambro and now available with Fresenius and other users makes use of 2 or 3 ultrafilters in the dialysate flow path operating in cross flow mode. The ultrafilters have a pore size of 0.05 μm, surface area of >2 m2 and are located after the dialysate mixing chamber. The dialysate is thus filtered prior to being delivered to the dialyzer with a 2-log reduction in its bacterial and endotoxin load. A portion of the dialysate is then passed through a second ultrafilter repeating the process, and this fluid which is sterile and has a 10,000 times lower concentration of endotoxin than normal dialysate is delivered directly into the blood circuit at a predetermined rate. The integrity of the ultrafilters is cyclically tested using a pressure holding test.
The process of cold sterilization by ultrafiltration was validated by Lebedo [49] for the Gambro system. It was shown that whereas 90% of the incoming water had bacterial growth and 35% had endotoxin detectable after three ultrafiltrations, no bacteria could be detected even in 30 l of infusate fluid. Similarly, Vasalaki validated the Fresenius system on 216 samples and showed levels in online substitution fluid comparable with that in commercially available bags meeting pharmacopeia standards [50]. Thus, the online system allows an almost unlimited supply of a sterile bicarbonate-based substitution fluid for replacement. The online plus system delivers the replacement fluid into the venous or arterial bubble chamber according to the rate set for the substitution pump, while the machine’s software ensures that the ultrafiltration pump removes an amount equal to the sum of replacement fluid and desired ultrafiltration from the blood compartment. The 5008 system has two substitution pumps with the ability to deliver replacement fluid either pre- or post-filter or both. One dry powder bicarbonate cartridge generally allows around 160 to 200 l of dialysate generation. With a dialysate flow of 100 ml/min and a replacement of 30 ml/kg/h for a 20-kg child, a treatment could actually be run for 24 h, making it even more efficient than CRRT.
Extra-corporeal circuit
Similar to IHD, the extra-corporeal volume (volume of blood tubing + dialyzer) should be less than 10% of the child’s total blood volume for PIRRT. If this is not possible, even with the use of size-specific blood tubing, one may need to prime the tubing + dialyzer with either colloid or crystalloid. The dialyzer used can be the same as in IHD (appropriate for the body surface area of the child). High flux dialyzers or hemofilters (AV series-Fresenius) will be needed if hemofiltration, i.e., convection component of clearance is to be added. The FX Paed dialyzer from Fresenius made of helixone deserves a special mention as it is suitable for very small children with a surface area of 0.2 m2, and requires a priming volume of just 18 ml. This dialyzer has a clearance of 65 to 75 ml/min and a UF coefficient of 7 ml/h/mmHg at blood flow rate of 30–100 ml/min. The large UF coefficient in such a small dialyzer allows ease of use for PIRRT even with additional convective clearance.
Prescription for PIRRT (Table 4)
PIRRT is more commonly done in the PICU, and vascular access is usually by cuffed or non-cuffed HD catheter of size appropriate for the child’s weight (detail available at http://pcrrt.com/ProtocolsAccess.html). Even in the unlikely presence of arterio-venous fistula (AVF), catheters are preferred, as the chance of needle dislodgment and subsequent bleeding is minimized. This is important given the prolonged duration of the sessions in contrast to standard HD.
Children in the PICU are quite different compared to those on chronic/maintenance HD. They are usually vasoconstricted by catecholamine treatment, may have hypoalbuminemia, low intravascular volumes, fluid overload, and are less likely to tolerate standard ultrafiltration without a precipitous drop in blood pressure. The target ultrafiltration will be determined by the balance between the degree of fluid overload, the obligatory fluid intake (comprising nutrition, blood products, antibiotics, and inotrope infusions) and the hemodynamic stability of the child. Achieving target ultrafiltration without disturbing hemodynamic stability is a special advantage of PIRRT compared to conventional HD, with only a minority of patients (<20%) requiring discontinuation of the HD due to refractory hypotension [27, 28, 34, 41, 51, 52]. A randomized controlled trial (RCT) compared cardiovascular stability between PIRRT and CVVH in adults. No significant differences in inotrope dose or numbers were seen between the two groups [38]. Limited pediatric data and author’s experience also suggest SLED to be well tolerated with adequate fluid removal [27].
The rates of Qb and Qd in PIRRT are decided based on the hemodynamic stability and are usually similar to those used in CVVH (Table 5). The Qd (dialysate flow rate) is kept low (usually ≤2 × Qb), which allows the same amount of dialysate to be used as in a standard HD session with higher flow rates despite longer sessions. The low Qd also helps in hemodynamic stability. The blood flow should be set based on the dialysate flow to allow a better saturation in diffusive mode. Usually, a Qd/Qb of 1.6 to 2 is considered to provide satisfactory dialysate saturation. Duration needs to be individualized as per the clinical status of the child and can vary between 6 to 18 h. As stated before, if SLEDD-f is being used, the blood flow may have to be adjusted according to the replacement fluid rate so that the filtration fraction does not exceed 20%.
Standard dialysate fluid consists of sodium, potassium, calcium, and bicarbonate, the concentration of which can be varied as per the clinical requirement. Similar to conventional HD, higher sodium or calcium can enable better hemodynamic stability. Compared to conventional IHD, PIRRT offers better small solute clearance. Large molecule clearance can be improved with the use of a high flux dialyzer and hemofiltration/hemodiafiltration, i.e., SLEDD-f [47]. An important finding reported with PIRRT has been low phosphate levels, which sometimes have to be replaced either intravenously or added to the dialysate [20]. Even though albumin is not lost, amino acid loses can be significant, requiring supplementation if PIRRT has to be continued for a longer period [38].
Anticoagulation in PIRRT
Unlike CVVH/D, PIRRT without anticoagulation is feasible, albeit with some risk of circuit clotting. Use of anticoagulation in PIRRT evokes mixed opinion as to whether to anticoagulate or not, and if anticoagulation is considered, whether to go for an unfractionated heparin or regional citrate anticoagulation protocol. A number of studies have examined the advantages and disadvantages of each of these protocols, although most of these trials were done in the adult population. The incidences of extracorporeal circuit clotting in these studies have varied between 26 and 46% with no anticoagulation and 10–26% with heparinization/citrate, respectively [23, 34,35,36,37, 39, 41, 42, 53,54,55,56].
No anticoagulation
Unlike CVVH/D, avoidance of anticoagulation is feasible in SLED with frequent saline flushing. In a study by Berbece et al. involving critical care patients on SLED for a mean duration of 8 h with blood and dialysate flow rates of 200 and 350 ml/min, respectively, anticoagulation with heparin was used in 35% of treatments and saline flushes in 65%. This study was done in comparison with continuous renal replacement therapy (CRRT) with citrate and heparin anticoagulation. The incidence of filter clotting in SLED therapy was 18% with heparin use and 29% without anticoagulation. There were no major adverse events reported [34]. In another study by Marshall et al., involving critically ill patients on SLED for a mean duration of 10.4 h with blood and dialysate flow rates of 201 ± 7.5 and 100 ml/min respectively, 41 of 145 treatments were without anticoagulation. The incidence of extracorporeal circuit clotting in this study was 26%, without a statistically significant difference between rates of clotting in heparin and heparin-free treatments [23]. Recently, Kitchlu et al. explored clinical outcomes in SLED therapy without anticoagulation compared to CRRT with citrate and heparin anticoagulation. The mean duration of SLED therapy was 7.11 h with blood and dialysate flow rates of 200 and 350 ml/min, respectively. The majority of SLED treatments (86.2%) were done without anticoagulation, but no significant differences in complications were noted [55]. All of these studies have demonstrated the feasibility of conducting PIRRT without anticoagulation, which is considered to be a major advantage of PIRRT over CVVH/D. It is generally suggested that that blood flow rate may have to be increased by 20 to 25% for an anticoagulation-free session provided it is hemodynamically tolerated [52, 56]. Removal of extra volumes of saline used for flushes should be considered and included in the ultrafiltration rate calculation. This can be problematic in a hemodynamically unstable child, but because of the slow and prolonged nature of PIRRT, this is often possible, albeit with some increased risk of circuit clotting. Madison and Depner at the University of California Davis studied 336 SLEDD sessions using saline flushes, 87 using citrate dialysate, and 72 with regional citrate anticoagulation [57]. The incidence of clotting with premature termination was 26% among saline flushes, 14% among citrate dialysate group (p = 0.005), and 2% among those receiving regional citrate anticoagulation 2% (p = 0.026).
Unfractionated heparin
As discussed above, use of unfractionated heparin in PIRRT does reduce the incidence of extracorporeal circuit clotting, but unfortunately this comes with the disadvantage of the higher risk of bleeding and thrombocytopenia requiring careful monitoring of activated partial thromboplastin time (APTT) and platelet count. PIRRT in contrast to CVVH/D requires a lower cumulative dose of anticoagulation although the amount of difference has varied between different studies [23, 37].
Regional citrate anticoagulation
Regional citrate anticoagulation (RCA) has evolved as an alternative form of anticoagulation, which is safe and yet effective [35, 36, 53, 54]. Fiaccadori et al. demonstrated the use of a simplified citrate-based protocol in SLED, which is less expensive and does not require monitoring of citrate accumulation [36]. The only disadvantage is that many hemodialysis units do not have sufficient experience in using citrate-based anticoagulation protocols.
Prostacyclin
There have been reports from Italy of using prostacyclin as an anticoagulant in SLED. However, it is expensive and further research is required to validate its use in routine practice [58]. Overall, it is generally advocated that the choice of anticoagulation (if used) should be made based on the local unit’s experience.
One has to keep in mind that most of the studies have been in adults, and children with their proportionately higher body surface area make direct correlation difficult. The only pediatric study by Lee et al. used a blood flow rate of 5 ml/kg/min for children who weighed 20–40 kg and 200 ml/min if weight > 40 kg, and a dialysate flow rate of 260 ml/min. Duration of therapy was 8–10 h/day and anticoagulation with unfractionated heparin was done in 76.6% of treatments with a bolus of 10–20 IU/kg and maintenance dose of 5–10 IU/kg/h. Adjusted doses of heparin were used if any of the following risk factors were present, i.e., APTT >75 s, international normalized ratio > 2, activated clotting time (ACT) >275, platelet count <50,000/μl and increased risk of bleeding. There were no bleeding complications observed in this study [27]. In our own experience, we have been able to conduct most of the SLED sessions in children with altered clotting off anticoagulation without any significant increase in adverse effects.
Dialysis dose
Determining the dosing of PIRRT in terms of duration, frequency, and dialysate or replacement fluid rate is difficult. Urea kinetic modeling (UKM) has been used to predict adequacy of dialysis in chronic RRT, but is unreliable in a non-steady evolving state such as AKI. Additionally, there is an as-yet-unanswered question regarding the relative merits of removal of small vs. large molecules. The rationale of encouraging middle-molecule clearance lies in its postulated benefit in removal of inflammatory mediators, which may have a role in the pathophysiology of systemic inflammatory response syndrome in critically ill patients [27, 59]. However, there is no concrete data that middle-molecule clearance shows a survival advantage in these patients [60,61,62].
Although there is no pediatric data on solute removal in PIRRT, it is helpful to understand the adult-based studies in this regard for prescribing PIRRT in critically ill children. An excellent study on kinetic modeling compared effective dose delivery by three acute dialysis therapies: CVVH, daily HD, and SLED [63]. A modified equivalent renal clearance (EKR) approach was used to account for the initial unsteady state during the dialysis. Effective small-solute clearance in CVVH was found to be 8% and 60% higher than in SLED and daily HD, respectively. Differences in favor of CVVH were more pronounced clearance for middle and large solute categories, likely due to a combination of convection and continuous operation. If one were to extrapolate from UKM data based on IHD and CRRT studies, PIRRT should provide at a minimum a weekly StdKt/Vurea of 2 when compared to IHD, or a weekly StdKt/Vurea of 6 when compared to CVVH [28]. It has been shown that undertaking PIRRT with Qd 350 ml/min, Qb 200 ml/min, hemofiltration 1 l/h and duration of 8 h/day for 6 days may be comparable to CRRT at 20 to 25 ml/kg/h [34]. From the study by Kielstein et al., it can be extrapolated that clearance obtained from 12 h of PIRRT is comparable to 23 h of CRRT [38]. They found a comparable urea reduction ratio between PIRRT and CVVH although the PIRRT patients were dialyzed for 11.7 ± 0.1 h compared with 23.3 ± 0.2 h for CRRT patients.
Monitoring during PIRRT
As PIRRT is most often used in ICUs on critically ill children, close monitoring of vital parameters is obviously an integral part. In ICUs, intra-arterial BP monitoring will be useful but for hemodynamically stable child non-invasive BP monitoring (such as with Dynamap) should suffice. PIRRT is very effective in solute removal because of its long duration and, unlike IHD, sometimes potassium, phosphate, and magnesium levels can dip, which can result in neuromuscular problems including difficulty in weaning off the ventilator. Hence, most of the PIRRT protocol includes the regular monitoring of phosphorous and magnesium in addition to the standard monitoring of urea, creatinine, and electrolytes, i.e., sodium, potassium, chloride, and calcium [21, 40, 41]. To factor in the risk of anticoagulation use, monitoring of APTT has been recommended in some studies, and the goal has ranged from 10 s above baseline to 1.5 times the normal value [21, 42, 64].
Outcomes
Even though there is a lack of robust evidence in favor of any specific dialysis modality for AKI [65,66,67], CVVH/D has been long held as the preferred choice for acutely ill patients and even KDIGO guidelines support its use [2, 66]. As mentioned above, evidence has been accumulating in favor of PIRRT as a viable alternative to CVVH/D.
Clearance/efficacy
Using single-pool UKM, SLED has been shown to offer very effective small solute clearance (Kt/V 1.3–1.5) and lower small solute disequilibrium compared to IHD, and provides equally effective azotemia control compared to CVVH [63]. Further improvement in middle- and large-molecule clearance can be achieved by adding convection clearance, i.e., by the use of hemodiafiltration (e.g., Fresenius Genius, and 5008 and 5008 S machines), although this is still not approved in the United States. A recent meta-analysis showed that compared to CRRT, IHD showed a trend towards higher incidence of dialysis dependence, albeit this result was primarily seen in observational cohorts rather than in RCTs [67]. The increased incidence of non-recovery of renal function may be attributed to the higher rates of incidental hypotension in IHD. PIRRT, being a hybrid technique, should theoretically provide better hemodynamic stability than IHD while achieving comparable clearance. Clinically, this was demonstrated by Wu et al., where better hemodynamic stability resulted in a negative indirect effect on mortality rate [7]. In one of the largest RCTs involving PIRRT, Schwenger et al. randomized 232 surgical ICU patients to either CVVH (35 ml/kg/h) or SLED using single-pass batch dialysate (12 h of dialysis with a blood flow rate of 100 to 120 ml/min) [37]. In addition to the absence of any difference in hemodynamic stability during treatments, the SLED group required fewer days of mechanical ventilation, fewer blood transfusions and was associated with decreased cost and nursing time. The recent systematic review by Zhang et al. also showed similar results in favor of PIRRT [21].
Mortality
Similar mortality outcome has been described by most of the RCTs comparing PIRRT with CVVH. In the large RCT by Schwenger et al., the 90-day mortality was comparable in both arms: 49.6% in SLED compared to 55.6% among those who underwent CVVH [37]. Likewise, meta-analysis has also failed to show any mortality benefit of CVVH over PIRRT [16]. Interestingly, summation of observational studies identified in the systematic review has shown a reduction in mortality trends favoring PIRRT, which has been postulated to be related to the decreased need for anti-coagulation in PIRRT [16]. Importantly, irrespective of the type of study, i.e., RCT or observational, PIRRT was found to be similar in efficacy to CVVH for fluid removal, solute clearance (urea, creatinine, phosphate), need for escalating vasopressor and mortality, or renal outcomes.
Complications
Serious complications on PIRRT have been reported to be low. A study by Caires et al. reported serious complications in only 0.7% (n = 3) sessions (arrhythmias and one death related to the procedure) in a total of 421 sessions [20]. Although this study excluded patients on epinephrine >0.2 mcg/kg/min or refractory hypotension, positive data have been reported even among more critically ill subjects. Ponce et al. observed serious complications (ventricular tachycardia or increase of nor-epinephrine dosage >1 mcg/kg/min) in only 1.4% of the sessions among a group of patients receiving nor-epinephrine (0.3 to 1 mcg/kg/min) [68]. The hemodynamic stability of PIRRT has been shown to have a stable effect on the mean arterial pressure [7] and this has been demonstrated to have a positive effect in a cohort of uremic patients with brain hemorrhage [13].
Cost-effectiveness
A significant advantage of PIRRT over CVVH/D has been its cost-effectiveness which is likely to make it very useful in any resource-constrained facilities. Schwenger et al. clearly demonstrated that SLED requires less nursing time and is significantly cheaper compared to CVVH [37]. The RRT cost per day for SLED using high flux membrane was €63.2 compared to €209.3 for CVVH. In contrast to CVVH, PIRRT usually does not require a special circuit or fluid and neither does it require round-the-clock nursing support nor any add-on training for the nurses. In addition, initial set-up cost is also less, as PIRRT does not require ultrapure water and can often be done on the same HD machine being used for conventional HD. Obviously, addition of convection clearance increases the cost as one needs to ensure ultrapure water, as well as requiring more specialized machines.
Comparison with PD
In resource-constrained units, PD definitely offers a cost-effective viable option for children with AKI in the PICU. Although in the developed world the use of acute PD has waned following the report of premature termination of the RCT by Phu et al. [9] due to higher mortality among PD (47%) cohort in contrast to hemofiltration (15%), it remains an important (and often the only) option in the developing world [11, 13]. Recent studies primarily from Brazil have demonstrated that critically ill AKI patients can be successfully treated with PD using cycler therapy, flexible catheters and high volumes (HV) of fluid, and both adequate small solute clearances and ultrafiltration can be achieved [69,70,71]. In contrast to the various studies comparing PIRRT with IHD and CVVH, there are very few studies (even among adults) that have compared PIRRT with PD. Ponce et al. reported on a double-center RCT comparing extended HD (EHD), i.e., PIRRT, with high-volume PD (HVPD) for the treatment for AKI in the ICU. Four hundred and seven patients were randomized but only 143 patients were analyzed. Although no survival benefit or difference in hospital stay was demonstrated, EHD did show faster metabolic control, higher dialysis dose, and better ultrafiltration in comparison to HVPD [10].
Pediatric study
At the time of writing, of this review, only a single study had been published detailing pediatric experience on PIRRT [27]. Lee et al. reviewed their experience on SLED-f among 14 critically ill children totaling 60 sessions. The study concluded that in their cohort of sick children, SLED-f provided good hemodynamic tolerance and correction of fluid overload, pH, and electrolyte imbalance. In addition, they also showed a significant drop in inflammatory markers such as adiponectin, interleukin 17 A (IL-17A), and IL 16, post SLED-f session. Despite a relatively high PRISM score (16.8 ± 23.3), they reported an overall 28-day survival of 71.4%. In the absence of any comparator group in their study, they compared the outcomes with the prospective pediatric continuous renal replacement therapy (ppCRRT) registry cohort. Although the different nature of the ppCRRT cohort as well as different time frame makes direct comparison difficult, they did show a superior survival rate in comparison to the ppCRRT group (100% survival for PRISM III score < 10 in comparison to 55% in the ppCRRT registry and 55.6% for PRISM III score > 10 vis-à-vis 47%) [3]. This survival benefit to some extent is in accordance with the meta-analysis of Zhang et al. [21] who postulated that lower need for heparin, lower incidence of circuit clot, and decreased rate of bio-film formation in PIRRT compared to CVVH might contribute towards the lower mortality, although it was not statistically significant. Lastly, SLED-f was found to be significantly cheaper, i.e., US$77 per day, as opposed to CVVH with an average expenditure of US $305.
Though the study was unique in being the first to analyze SLED-f in children, the small study population, selective cohort (excluded children less than 20 kg) and retrospective nature of the study did leave a lot of unanswered questions regarding its viability in young critically ill children who are more prone to hemodynamic instability, as well as in a non-selected prospective cohort. Additionally, it has to be emphasized that the cohort of Lee et al. underwent filtration along with dialysis. Although SLED can be undertaken without much addition to a standard HD unit, filtration requires ultrapure water, which may increase the initial set-up cost, making it difficult for resource-constrained facilities where the utility of SLED is likely to be most important vis-à-vis CRRT. Another major pitfall is assessing the adequacy of dialysis dose prescribed, as even the adult literature does not have robust data and pediatric data is non-existent. None of the major adult studies, like the Brazil RCT or the Hannover Dialysis Outcome study showed any significant survival advantage of intensified HD and hence the optimum dose of dialysis remains debatable [51, 72].
Drug-dosing adjustments during SLED
Despite the increasing reports of feasibility and usefulness of PIRRT, drug dosing remains a major concern. A lack of studies and an absence of a standard definition for PIRRT has made it challenging for pharmacists and nephrologists when it comes to antibiotic dosing in the setting of SLED in critically ill septic patients. A recent electronic survey done to check pharmacists’ antibiotic dosing recommendations in SLED showed wide variations from 4- to 12-fold in dosing regimens across health facilities, and suggested monitoring of drug concentrations in blood and use of pharmacokinetic modeling techniques for appropriate dosing in SLED [73]. As pharmacokinetic studies for SLED in the pediatric population are lacking, we have to extrapolate from adult studies regarding any drug dosage adjustments. Unfortunately, even adult studies are few in number (Table 6), making robust recommendations difficult [74,75,76,77,78,79,80,81,82,83,84,85,86].
Conclusions
PIRRT provides a modality of RRT with excellent hemodynamic stability, acceptable biochemical clearance, and ease of use without the need for specialized equipment. It can be performed with a conventional dialysis machine used in a chronic maintenance dialysis program, and costs a small fraction of CVVH expenditure. Perhaps most importantly the flexible nature of this modality allows sufficient time for any ancillary procedures/treatments such as imaging or surgical intervention. Although we do not have very robust evidence supporting the superiority of PIRRT over CVVH, current evidence does support the outcomes of PIRRT being at least equivalent to CVVH. Similarly, while the use of cyclers and flexible catheters are likely to have made PD a more competitive option for children with AKI, effective fluid removal with PD remains an important concern, particularly in children with fluid overload. The availability of PIRRT in such a scenario is likely to be useful. Finally, it should be accepted that these therapeutic strategies may not necessarily be considered as competitors, but rather as alternatives, each of which might be applicable within the same unit and even the same patient, depending on the practical options at hand at a given time and on the metabolic or fluid balance needs of the patient. The definite advantage that PIRRT does have over CRRT is its cost-effectiveness, which is important in resource-constrained facilities, and its lesser requirement for anticoagulation. As initiating PIRRT in children poses challenges quite different to adults, one has to appreciate the current limitations, particularly adequacy, and dose modifications. In view of only a single pediatric study, further research is warranted to check for feasibility, tolerability, adequacy measurement, and drug-dose modifications in critically ill children on PIRRT.
References
Lameire NH, Bagga A, Cruz D, De Maeseneer J, Endre Z, Kellum JA, Liu KD, Mehta RL, Pannu N, Van Biesen W, Vanholder R (2013) Acute kidney injury: an increasing global concern. Lancet 382:170–179
Kidney Disease Improving Global Outcomes (2012) KDIGO Clinical Practice Guideline for Acute Kidney Injury. Available from http://kdigo.org/guidelines/acute-kidney-injury-2/ Accessed 13.04.17
Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, Hackbarth R, Somers MJ, Baum M, Symons JM, Flores FX, Benfield M, Askenazi D, Chand D, Fortenberry JD, Mahan JD, McBryde K, Blowey D, Goldstein SL (2010) Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis 55:316–325
Zarbock A, Kellum JA, Schmidt C, Van Aken H, Wempe C, Pavenstädt H, Boanta A, Gerß J, Meersch M (2016) Effect of early vs delayed initiation of renal replacement therapy on mortality in critically ill patients with acute kidney injury. JAMA 315:2190–2199
Bagshaw SM, George C, Bellomo R, Database Management Committee ANZICS (2008) Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care 12:R47
Honore PM, Jacobs R, Hendrickx I, Bagshaw SM, Joannes-Boyau O, Boer W, De Waele E, Van Gorp V, Spapen HD (2015) Prevention and treatment of sepsis-induced acute kidney injury: an update. Ann Intensive Care 5:51
Wu VC, Huang TM, Shiao CC, Lai CF, Tsai PR, Wang WJ, Huang HY, Wang KC, Ko WJ, Wu KD, NSARF Group (2013) The hemodynamic effects during sustained low-efficiency dialysis versus continuous veno-venous hemofiltration for uremic patients with brain hemorrhage: a crossover study. J Neurosurg 119:1288–1295
Ponce D, Buffarah MB, Goes C, Balbi A (2015) Peritoneal dialysis in acute kidney injury: trends in the outcome across time periods. PLoS One 10:e0126436
Phu NH, Hien TT, Mai NT, Chau TT, Chuong LV, Loc PP, Winearls C, Farrar J, White N, Day N (2002) Hemofiltration and peritoneal dialysis in infection-associated acute renal failure in Vietnam. N Engl J Med 347:895–902
Ponce D, Berbel MN, Abrão JM, Goes CR, Balbi AL (2013) A randomized clinical trial of high volume peritoneal dialysis versus extended daily hemodialysis for acute kidney injury patients. Int Urol Nephrol 45:869–878
Ponce D, Gobo-Oliveira M, Balbi AL (2017) Peritoneal dialysis treatment modality option in acute kidney injury. Blood Purif 43:173–178
Almeida CP, Ponce D, de Marchi AC, Balbi AL (2014) Effect of peritoneal dialysis on respiratory mechanics in acute kidney injury patients. Perit Dial Int 34:544–549
Bonilla-Félix M (2009) Peritoneal dialysis in the pediatric intensive care unit setting. Perit Dial Int 29(Suppl 2):S183–S185
Fortenberry JD, Paden ML, Goldstein SL (2013) Acute kidney injury in children: an update on diagnosis and treatment. Pediatr Clin N Am 60:669–688
Basu RK, Wheeler DS, Goldstein S, Doughty L (2011) Acute renal replacement therapy in pediatrics. Int J Nephrol 2011:785392
Sutherland SM, Alexander SR (2012) Continuous renal replacement therapy in children. Pediatr Nephrol 27:2007–2016
Legrand M, Darmon M, Joannidis M, Payen D (2013) Management of renal replacement therapy in ICU patients: an international survey. Intensive Care Med 39:101–108
Wu VC, Wang CH, Wang WJ, Lin YF, Hu FC, Chen YW, Chen YS, Wu MS, Lin YH, Kuo CC, Huang TM, Chen YM, Tsai PR, Ko WJ, Wu KD, NSARF Study Group (2010) Sustained low-efficiency dialysis versus continuous veno-venous hemofiltration for postsurgical acute renal failure. Am J Surg 199:466–476
Cheng J, Hu S, Lu H, Lei Q, Liu J, Yuan F, Chen R (2013) Comparison of the therapeutic effectiveness of sustained low-efficiency dialysis (SLED) with continuous blood purification (CBP) in critically ill patients. Cell Biochem Biophys 67:923–927
Caires RA, Abdulkader RC, Costa E Silva VT, Ferreira GS, Burdmann EA, Yu L, Macedo E (2016) Sustained low-efficiency extended dialysis (SLED) with single-pass batch system in critically-ill patients with acute kidney injury (AKI). J Nephrol 29:401–409
Zhang L, Yang J, Eastwood GM, Zhu G, Tanaka A, Bellomo R (2015) Extended daily dialysis versus continuous renal replacement therapy for acute kidney injury: a meta-analysis. Am J Kidney Dis 66:322–330
Abe M, Okada K, Suzuki M, Nagura C, Ishihara Y, Fujii Y, Ikeda K, Kaizu K, Matsumoto K (2010) Comparison of sustained hemodiafiltration with continuous venovenous hemodiafiltration for the treatment of critically ill patients with acute kidney injury. Artif Organs 34:331–338
Marshall MR, Golper TA, Shaver MJ, Alam MG, Chatoth DK (2001) Sustained low-efficiency dialysis for critically ill patients requiring renal replacement therapy. Kidney Int 60:777–785
Naka T, Baldwin I, Bellomo R, Fealy N, Wan L (2004) Prolonged daily intermittent renal replacement therapy in ICU patients by ICU nurses and ICU physicians. Int J Artif Organs 27:380–387
Fieghen HE, Friedrich JO, Burns KE, Nisenbaum R, Adhikari NK, Hladunewich MA, Lapinsky SE, Richardson RM, Wald R, University of Toronto Acute Kidney Injury Research Group (2010) The hemodynamic tolerability and feasibility of sustained low efficiency dialysis in the management of critically ill patients with acute kidney injury. BMC Nephrol 11:32
Kron J, Kron S, Wenkel R, Schuhmacher HU, Thieme U, Leimbach T, Kern H, Neumayer HH, Slowinski T (2012) Extended daily on-line high-volume haemodiafiltration in septic multiple organ failure: a well-tolerated and feasible procedure. Nephrol Dial Transplant 27:146
Lee CY, Yeh HC, Lin CY (2016) Treatment of critically ill children with kidney injury by sustained low-efficiency daily diafiltration. Pediatr Nephrol 27:2301–2309
Edrees F, Li T, Vijayan A (2016) Prolonged intermittent renal replacement therapy. Adv Chronic Kidney Dis 23:195–202
Kielstein JT, Schiffer M, Hafer C (2010) Back to the future: extended dialysis for treatment of acute kidney injury in the intensive care unit. J Nephrol 23:494–501
Himmelfarb J, Ikizler TA (2000) Quantitating urea removal in patients with acute renal failure: lost art or forgotten science? Semin Dial 13:147–149
Kudoh Y, Iimura O (1988) Slow continuous hemodialysis—new therapy for acute renal failure in critically ill patients–part 1. Theoretical consideration and new technique Jpn Circ J 52:1171–1182
Kudoh Y, Shiiki M, Sasa Y, Hotta D, Nozawa A, Iimura O (1988) Slow continuous hemodialysis—new therapy for acute renal failure in critically ill patients—part 2. Animal experiments and clinical implication. Jpn Circ J 52:1183–1190
Schlaeper C, Amerling R, Manns M, Levin NW (1999) High clearance continuous renal replacement therapy with a modified dialysis machine. Kidney Int Suppl 72:S20–S23
Berbece AN, Richardson RM (2006) Sustained low-efficiency dialysis in the ICU: cost, anticoagulation, and solute removal. Kidney Int 70:963–968
Clark JA, Schulman G, Golper TA (2008) Safety and efficacy of regional citrate anticoagulation during 8-hour sustained lowefficiency dialysis. Clin J Am Soc Nephrol 3:736–742
Fiaccadori E, Regolisti G, Cademartiri C, Cabassi A, Picetti E, Barbagallo M, Gherli T, Castellano G, Morabito S, Maggiore U (2013) Efficacy and safety of a citrate-based protocol for sustained low-efficiency dialysis in AKI using standard dialysis equipment. Clin J Am Soc Nephrol 8:1670–1678
Schwenger V, Weigand MA, Hoffmann O, Dikow R, Kihm LP, Seckinger J, Miftari N, Schaier M, Hofer S, Haar C, Nawroth PP, Zeier M, Martin E, Morath C (2012) Sustained low efficiency dialysis using a single-pass batch system in acute kidney injury—a randomized interventional trial: the REnal replacement therapy study in intensive care unit PatiEnts. Crit Care 16:R140
Kielstein JT, Kretschmer U, Ernst T, Hafer C, Bahr MJ, Haller H, Fliser D (2004) Efficacy and cardiovascular tolerability of extended dialysis in critically ill patients: a randomized controlled study. Am J Kidney Dis 43:342–349
Kumar VA, Craig M, Depner TA, Yeun JY (2000) Extended daily dialysis: a new approach to renal replacement for acute renal failure in the intensive care unit. Am J Kidney Dis 36:294–300
Lonnemann G, Floege J, Kliem V, Brunkhorst R, Koch KM (2000) Extended daily veno-venous high-flux haemodialysis in patients with acute renal failure and multiple organ dysfunction syndrome using a single path batch dialysis system. Nephrol Dial Transplant 15:1189–1193
Albino BB, Balbi AL, Abrao JM, Ponce D (2015) Dialysis complications in acute kidney injury patients treated with prolonged intermittent renal replacement therapy sessions lasting 10 versus 6 hours: results of a randomized clinical trial. Artif Organs 39:423–431
Marshall MR, Ma T, Galler D, Rankin AP, Williams AB (2004) Sustained low-efficiency daily diafiltration (SLEDD-f) for critically ill patients requiring renal replacement therapy: towards an adequate therapy. Nephrol Dial Transplant 19:877–884
Bunchman TE (2008) Treatment of acute kidney injury in children: from conservative management to renal replacement therapy. Nat Clin Pract Nephrol 4:510–514
Basu RK, Devarajan P, Wong H, Wheeler DS (2011) An update and review of acute kidney injury in pediatrics. Pediatr Crit Care Med 12:339–347
Fliser D, Kielstein JT (2006) Technology insight: treatment of renal failure in the intensive care unit with extended dialysis. Nat Clin Pract Nephrol 2:32–39
Overberger P, Pesacreta M, Palevsky PM, VA/NIH Acute Renal Failure Trial Network (2007) Management of renal replacement therapy in acute kidney injury: a survey of practitioner prescribing practices. Clin J Am Soc Nephrol 2:623–630
Basso F, Ricci Z, Cruz D, Ronco C (2010) International survey on the management of acute kidney injury in critically ill patients: year 2007. Blood Purif 30:214–220
Annigeri RA, Nandeesh V, Karuniya R, Rajalakshmi S, Venkataraman R, Ramakrishnan N (2016) Impact of dialysis practice patterns on outcomes in acute kidney injury in intensive care unit. Indian J Crit Care Med 20:14–20
Ledebo I (2002) On-line preparation of solutions for dialysis: practical aspects versus safety and regulations. J Am Soc Nephrol 13(Suppl 1):S78–S83
Vaslaki L, Karátson A, Vörös P, Major L, Pethö F, Ladányi E, Weber C, Mitteregger R, Falkenhagen D (2000) Can sterile and pyrogen-free on-line substitution fluid be routinely delivered? A multicentric study on the microbiological safety of on-line haemodiafiltration. Nephrol Dial Transplant 15(Suppl 1):74–78
Lima EQ, Silva RG, Donadi EL, Fernandes AB, Zanon JR, Pinto KR, Burdmann EA (2012) Prevention of intradialytic hypotension in patients with acute kidney injury submitted to sustained low-efficiency dialysis. Ren Fail 34:1238–1243
Tolwani AJ, Wheeler TS, Wille KM (2007) Sustained low-efficiency dialysis. Contrib Nephrol 156:320–324
Morabito S, Pistolesi V, Tritapepe L, Fiaccadori E (2014) Regional citrate anticoagulation for RRTs in critically ill patients with AKI. Clin J Am Soc Nephrol 9:2173–2188
Lahmer T, Messer M, Rasch S, Beitz A, Schnappauf C, Schmid RM, Huber W (2015) Sustained low-efficiency dialysis with regional citrate anticoagulation in medical intensive care unit patients with liver failure: a prospective study. J Crit Care 30:1096–1100
Kitchlu A, Adhikari N, Burns KE, Friedrich JO, Garg AX, Klein D, Richardson RM, Wald R (2015) Outcomes of sustained low efficiency dialysis versus continuous renal replacement therapy in critically ill adults with acute kidney injury: a cohort study. BMC Nephrol 16:127
Gashti CN, Salcedo S, Robinson V, Rodby RA (2008) Accelerated venovenous hemofiltration: early technical and clinical experience. Am J Kidney Dis 51:804–810
Madison J, Ilumin M, Chin A (2005) Citrate-containing dialysate is well tolerated during slow extended daily dialysis in the ICU. J Am Soc Nephrol 16:314A
Schetz M (1999) Non-renal indications for continuous renal replacement therapy. Kidney Int 56(Suppl 72):S88–S94
Tonelli M, Manns B, Feller-Kopman D (2002) Acute renal failure in the intensive care unit: a systematic review of the impact of dialytic modality on mortality and renal recovery. Am J Kidney Dis 40:875–885
Kellum JA, Angus DC, Johnson JP, Leblanc M, Griffin M, Ramakrishnan N, Linde-Zwirble WT (2002) Continuous versus intermittent renal replacement therapy: a meta-analysis. Intensive Care Med 28:29–37
Pannu N, Klarenbach S, Wiebe N, Manns B, Tonelli M, Network AKD (2008) Renal replacement therapy in patients with acute renal failure: a systematic review. JAMA 299:793–805
Liao Z, Zhang W, Hardy PA, Poh CK, Huang Z, Kraus MA, Clark WR, Gao D (2003) Kinetic comparison of different acute dialysis therapies. Artif Organs 27:802–807
Kumar VA, Yeun JY, Depner TA, Don BR (2004) Extended daily dialysis vs. continuous hemodialysis for ICU patients with acute renal failure: a two-year single center report. Int J Artif Organs 27:371–379
Walters S, Porter C, Brophy PD (2009) Dialysis and pediatric acute kidney injury: choice of renal support modality. Pediatr Nephrol 24:37–48
Ghahramani N, Shadrou S, Hollenbeak C (2008) A systematic review of continuous renal replacement therapy and intermittent haemodialysis in management of patients with acute renal failure. Nephrology (Carlton) 13:570–578
Rabindranath K, Adams J, Macleod AM, Muirhead N (2007) Intermittent versus continuous renal replacement therapy for acute renal failure in adults. Cochrane Database Syst Rev 3:CD003773
Schneider AG, Bellomo R, Bagshaw SM, Glassford NJ, Lo S, Jun M, Cass A, Gallagher M (2013) Choice of renal replacement therapy modality and dialysis dependence after acute kidney injury: a systematic review and meta-analysis. Intensive Care Med 39:987–997
Ponce D, Abrão JM, Albino BB, Balbi AL (2013) Extended daily dialysis in acute kidney injury patients: metabolic and fluid control and risk factors for death. PLoS One 8:e81697
Gabriel DP, Nascimento GV, Caramori JT, Martim LC, Barretti P, Balbi AL (2007) High volume peritoneal dialysis for acute renal failure. Perit Dial Int 27:277–282
Gabriel DP, Caramori JT, Martim LC, Barretti P, Balbi AL (2008) High volume peritoneal dialysis vs daily hemodialysis: a randomized, controlled trial in patients with acute kidney injury. Kidney Int Suppl 73:S87–S93
Ponce D, Berbel MN, Regina de Goes C, Almeida CT, Balbi AL (2012) High-volume peritoneal dialysis in acute kidney injury: indications and limitations. Clin J Am Soc Nephrol 7:887–894
Faulhaber-Walter R, Hafer C, Jahr N, Vahlbruch J, Hoy L, Haller H, Fliser D, Kielstein JT (2009) The Hannover dialysis outcome study: comparison of standard versus intensified extended dialysis for treatment of patients with acute kidney injury in the intensive care unit. Nephrol Dial Transplant 24:2179–2186
Mei JP, Ali-Moghaddam A, Mueller BA (2016) Survey of pharmacists’ antibiotic dosing recommendations for sustained low-efficiency dialysis. Int J Clin Pharm 38:127–134
Kielstein JT, Czock D, Schopke T, Hafer C, Bode-Böger SM, Kuse E, Keller F, Fliser D (2006) Pharmacokinetics and total elimination of meropenem and vancomycin in intensive care unit patients undergoing extended daily dialysis. Crit Care Med 34:51–56
Kielstein JT, Eugbers C, Bode-Boeger SM, Martens-Lobenhoffer J, Haller H, Joukhadar C, Traunmüller F, Knitsch W, Hafer C, Burkhardt O (2010) Dosing of daptomycin in intensive care unit patients with acute kidney injury undergoing extended dialysis—a pharmacokinetic study. Nephrol Dial Transplant 25:1537–1541
Lorenzen JM, Broll M, Kaever V, Burhenne H, Hafer C, Clajus C, Knitsch W, Burkhardt O, Kielstein JT (2012) Pharmacokinetics of ampicillin/ sulbactam in critically ill patients with acute kidney injury undergoing extended dialysis. Clin J Am Soc Nephrol 7:385–390
Fiaccadori E, Maggiore U, Rotelli C, Giacosa R, Parenti E, Picetti E, Sagripanti S, Manini P, Andreoli R, Cabassi A (2004) Removal of linezolid by conventional intermittent hemodialysis, sustained low-efficiency dialysis, or continuous venovenous hemofiltration in patients with acute renal failure. Crit Care Med 32:2437–2442
Golestaneh L, Gofran A, Mokrzycki MH, Chen JL (2009) Removal of vancomycin in sustained low-efficiency dialysis (SLED): a need for better surveillance and dosing. Clin Nephrol 72:286–291
Roberts JA, Field J, Visser A, Whitbread R, Tallot M, Lipman J, Kirkpatrick CM (2010) Using population pharmacokinetics to determine gentamicin dosing during extended daily diafiltration in critically ill patients with acute kidney injury. Antimicrob Agents Chemother 54:3635–3640
Manley HJ, Bailie GR, McClaran ML, Bender WL (2003) Gentamicin pharmacokinetics during slow daily home hemodialysis. Kidney Int 63:1072–1078
Bogard KN, Peterson NT, Plumb TJ, Erwin MW, Fuller PD, Olsen KM (2011) Antibiotic dosing during sustained low-efficiency dialysis: special considerations in adult critically ill patients. Crit Care Med 39:560–570
Burkhardt O, Hafer C, Langhoff A, Kaever V, Kumar V, Welte T, Haller H, Fliser D, Kielstein JT (2009) Pharmacokinetics of ertapenem in critically ill patients with acute renal failure undergoing extended daily dialysis. Nephrol Dial Transplant 24:267–271
Ahern JW, Lai C, Rebuck JA, Possidente CJ, Weidner M (2004) Experience with vancomycin in patients receiving slow low-efficiency dialysis. Hosp Pharm 39:138–143
Czock D, Hüsig-Linde C, Langhoff A, Schöpke T, Hafer C, de Groot K, Swoboda S, Kuse E, Haller H, Fliser D, Keller F, Kielstein JT (2006) Pharmacokinetics of moxifloxacin and levofloxacin in intensive care unit patients who have acute renal failure and undergo extended daily dialysis. Clin J Am Soc Nephrol 1:1263–1268
Clajus C, Kühn-Velten WN, Schmidt JJ, Lorenzen JM, Pietsch D, Beutel G, Kielstein JT (2013) Cotrimoxazole plasma levels, dialyzer clearance and total removal by extended dialysis in a patient with acute kidney injury: risk of under-dosing using current dosing recommendations. BMC Pharmacol Toxicol 14:19
Mueller BA, Scoville BA (2012) Adding to the armamentarium: antibiotic dosing in extended dialysis. Clin J Am Soc Nephrol 7:373–375
Acknowledgements
The authors wish to acknowledge Jennifer L. Clark, Grant/Medical Writer at Rebecca D. Considine Clinical Research Institute, Akron Children Hospital and Dr. Vinod Krishappa research fellow at Akron General Hospital, Cleveland Clinic Foundation, Akron, Ohio.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding/ support
None.
Competing interests
Dr. Timothy Bunchman has served as consultant to Baxter. The rest of the authors do not have any relevant competing interests to disclose.
Additional information
Both Rajiv Sinha and Sidharth Kumar Sethi are first authors of the manuscript.
Rights and permissions
About this article
Cite this article
Sinha, R., Sethi, S.K., Bunchman, T. et al. Prolonged intermittent renal replacement therapy in children. Pediatr Nephrol 33, 1283–1296 (2018). https://doi.org/10.1007/s00467-017-3732-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3732-2