Abstract
Background
Gastroesophageal reflux disease (GERD) is one of the most common diseases in North America and globally. The aim of this guideline is to provide evidence-based recommendations regarding the most utilized and available endoscopic and surgical treatments for GERD.
Methods
Systematic literature reviews were conducted for 4 key questions regarding the surgical and endoscopic treatments for GERD in adults: preoperative evaluation, endoscopic vs surgical or medical treatment, complete vs partial fundoplication, and treatment for obesity (body mass index [BMI] ≥ 35 kg/m2) and concomitant GERD. Evidence-based recommendations were formulated using the GRADE methodology by subject experts. Recommendations for future research were also proposed.
Results
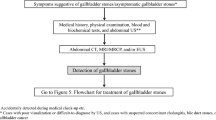
The consensus provided 13 recommendations. Through the development of these evidence-based recommendations, an algorithm was proposed for aid in the treatment of GERD. Patients with typical symptoms should undergo upper endoscopy, manometry, and pH-testing; additional testing may be required for patients with atypical or extra-esophageal symptoms. Patients with normal or abnormal findings on manometry should consider undergoing partial fundoplication. Magnetic sphincter augmentation or fundoplication are appropriate surgical procedures for adults with GERD. For patients who wish to avoid surgery, the Stretta procedure and transoral incisionless fundoplication (TIF 2.0) were found to have better outcomes than proton pump inhibitors alone. Patients with concomitant obesity were recommended to undergo either gastric bypass or fundoplication, although patients with severe comorbid disease or BMI > 50 should undergo Roux-en-Y gastric bypass for the additional benefits that follow weight loss.
Conclusion
Using the recommendations an algorithm was developed by this panel, so that physicians may better counsel their patients with GERD. There are certain patient factors that have been excluded from included studies/trials, and so these recommendations should not replace surgeon–patient decision making. Engaging in the identified research areas may improve future care for GERD patients.

Similar content being viewed by others
Abbreviations
- ARM:
-
Anti-reflux medication
- ARS:
-
Anti-reflux surgery
- CI:
-
Confidence interval
- EGD:
-
Esophagogastroduodenoscopy
- MSA:
-
Magnetic sphincter augmentation
- GERD:
-
Gastroesophageal reflux disease
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
- HREM:
-
High-resolution esophageal manometry
- KQ:
-
Key question
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QoL:
-
Quality of life
- PPI:
-
Proton pump inhibitor
- LES:
-
Lower esophageal sphincter
- LA:
-
Los Angeles
- Stretta procedure:
-
Radiofrequency treatment for GERD
- RCT:
-
Randomized clinical trial
- TIF:
-
Transoral incisionless fundoplication
- RYGB:
-
Roux-en-Y gastric bypass
- LNF:
-
Laparoscopic Nissen Fundoplication
References
Andrews JC, Schünemann HJ, Oxman AD, Pottie K, Meerpohl JJ, Coello PA, Rind D, Montori VM, Brito JP, Norris S, Elbarbary M, Post P, Nasser M, Shukla V, Jaeschke R, Brozek J, Djulbegovic B, Guyatt G (2013) GRADE guidelines: 15. Going from evidence to recommendation-determinants of a recommendation’s direction and strength. J Clin Epidemiol 66:726–735
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R, Global Consensus Group (2006) The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 101:1900–1920 (quiz 1943)
Sandhu DS, Fass R (2018) Current trends in the management of gastroesophageal reflux disease. Gut Liver 12:7–16
El-Serag HB, Sweet S, Winchester CC, Dent J (2014) Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 63:871–880
Thong BKS, Ima-Nirwana S, Chin KY (2019) Proton pump inhibitors and fracture risk: a review of current evidence and mechanisms involved. Int J Environ Res Public Health 16:1571
Chimukangara M, Jalilvand AD, Melvin WS, Perry KA (2019) Long-term reported outcomes of transoral incisionless fundoplication: an 8-year cohort study. Surg Endosc 33:1304–1309
Roks DJ, Broeders JA, Baigrie RJ (2017) Long-term symptom control of gastro-oesophageal reflux disease 12 years after laparoscopic Nissen or 180° anterior partial fundoplication in a randomized clinical trial. Br J Surg 104:852–856
Limpert PA, Naunheim KS (2005) Partial versus complete fundoplication: Is there a correct answer? Surg Clin North Am 85:399–410
Higgins RM, Gould JC (2020) The pros and cons of partial versus total fundoplication for gastroesophageal reflux disease. J Laparoendosc Adv Surg Tech A 30:117–120
Broeders J, Mauritz F, Ahmed AU, Draaisma W, Ruurda J, Gooszen H, Smout AJ, Broeders IA, Hazebroek EJ (2010) Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Br J Surg 97:1318–1330
Du X, Hu Z, Yan C, Zhang C, Wang Z, Wu JA (2016) A meta-analysis of long follow-up outcomes of laparoscopic Nissen (total) versus Toupet (270°) fundoplication for gastro-esophageal reflux disease based on randomized controlled trials in adults. BMC Gastroenterol 16:88
Corley DA, Kubo A (2006) Body mass index and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Gastroenterol 101:2619–2628
Delshad SD, Almario CV, Chey WD, Spiegel BMR (2020) Prevalence of gastroesophageal reflux disease and proton pump inhibitor-refractory symptoms. Gastroenterology 158(1250–1261):e2
Bou Daher H, Sharara AI (2019) Gastroesophageal reflux disease, obesity and laparoscopic sleeve gastrectomy: The burning questions. World J Gastroenterol 25:4805–4813
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD, GRADE Working Group (2016) GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ 353:1
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ, GRADE Working Group (2016) GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ 353:i2089
GRADEpro GDT (2021) GRADEpro Guideline Development Tool [Software]: McMaster University and Evidence Prime. Available from: http://www.gradepro.org
Chen Y, Yang K, Marusic A, Qaseem A, Meerpohl JJ, Flottorp S, Akl EA, Schünemann HJ, Chan ES, Falck-Ytter Y, Ahmed F, Barber S, Chen C, Zhang M, Xu B, Tian J, Song F, Shang H, Tang K, Wang Q, Norris SL, RIGHT (Reporting Items for Practice Guidelines in Healthcare) Working Group (2017) A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med 166:128–132
Rogers AT, Dirks R, Burt HA, Haggerty S, Kohn GP, Slater BJ, Walsh D, Stefanidis D, Pryor A (2021) Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines development: standard operating procedure. Surg Endosc 35:2417–2427
Schünemann H, Brożek J, Guyatt G, Oxman A (2013) GRADE handbook for grading quality of evidence and strength of recommendations. McMaster University and Evidence Prime. Available from: http://guidelinedevelopment.org/handbook.
World Health Organization (2014) Decision-making for guideline development at WHO. WHO handbook for guideline development –, 2nd edn. WHO Press, Geneva, pp 201–214
Andolfi C, Vigneswaran Y, Kavitt RT, Herbella FA, Patti MG (2017) Laparoscopic Antireflux Surgery: importance of patient’s selection and preoperative workup. J Laparoendosc Adv Surg Tech A 27:101–105
Bello B, Zoccali M, Gullo R, Allaix ME, Herbella FA, Gasparaitis A, Patti MG (2013) Gastroesophageal reflux disease and antireflux surgery-what is the proper preoperative work-up? J Gastrointest Surg 17:14–20
Benassai G, Mastrorilli M, Quarto G, Galloro G, Cantelmo A, Esposito T (2006) Laparoscopic antireflux surgery: indications, preoperative evaluation, techniques, and outcomes. Hepatogastroenterology 53:77–81
Blom D, Peters JH, DeMeester TR, Crookes PF, Hagan JA, DeMeester SR, Bremner C (2002) Physiologic mechanism and preoperative prediction of new-onset dysphagia after laparoscopic Nissen fundoplication. J Gastrointest Surg 6:22–27 (discussion 27-28)
Booth M, Stratford J, Dehn TC (2002) Preoperative esophageal body motility does not influence the outcome of laparoscopic Nissen fundoplication for gastroesophageal reflux disease. Dis Esophagus 15:57–60
Campos GM, Peters JH, DeMeester TR, Oberg S, Crookes PF, Tan S, DeMeester SR, Hagen JA, Bremner CG (1999) Multivariate analysis of factors predicting outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg 3:292–300
Chan WW, Haroian LR, Gyawali CP (2011) Value of preoperative esophageal function studies before laparoscopic antireflux surgery. Surg Endosc 25:2943–2949
Chin KF, Myers JC, Jamieson GG, Devitt PG (2008) Symptoms experienced during 24-h pH monitoring and their relationship to outcome after laparoscopic total fundoplication. Dis Esophagus 21:445–451
del Genio G, Tolone S, Rossetti G, Brusciano L, del Genio F, Pizza F, Russo F, Di Martino M, Napolitano V, del Genio A (2008) Total fundoplication does not obstruct the esophageal secondary peristalsis: investigation with pre- and postoperative 24-hour pH-multichannel intraluminal impedance. Eur Surg Res 40:230–234
Fanous MY, Jaehne AK, Lorenson D, Williams S (2021) Impact of participation of surgeons in diagnostic studies of gastroesophageal reflux disease on completion of workup and utilization of antireflux surgery. Surg Innov 28:58–61
Fein M, Bueter M, Thalheimer A, Pachmayr V, Heimbucher J, Freys SM, Fuchs KH (2008) Ten-year outcome of laparoscopic antireflux surgery. J Gastrointest Surg 12:1893–1899
Fuchs HF, Gutschow CA, Brinkmann S, Herbold T, Bludau M, Schröder W, Bollschweiler E, Hölscher AH, Leers JM (2014) Effect of laparoscopic antireflux surgery on esophageal motility. Dig Surg 31:354–358
Goss B, Shacham Y, Szold A (2003) Complete fundoplication has similar long-term results in patients with and without esophageal body dysmotility. Surg Endosc 17:567–570
Iwai N, Kaneda H, Tsuto T, Yanagihara J, Kojima O, Nishioka B, Fujita Y, Majima S (1984) Manometric study and prolonged pH monitoring of the esophagus in patients with hiatus hernia before and after operation. Gastroenterol Jpn 19:307–312
Kapadia S, Osler T, Lee A, Borrazzo E (2018) The role of preoperative high resolution manometry in predicting dysphagia after laparoscopic Nissen fundoplication. Surg Endosc 32:2365–2372
Khajanchee YS, Hong D, Hansen PD, Swanstrom LL (2004) Outcomes of antireflux surgery in patients with normal preoperative 24-hour pH test results. Am J Surg 187:599–603
Lugaresi M, Aramini B, Daddi N, Baldi F, Mattioli S (2015) Effectiveness of antireflux surgery for the cure of chronic cough associated with gastroesophageal reflux disease. World J Surg 39:208–215
Malhotra A, Freston JW, Aziz K (2008) Use of pH-impedance testing to evaluate patients with suspected extraesophageal manifestations of gastroesophageal reflux disease. J Clin Gastroenterol 42:271–278
Marjoux S, Roman S, Juget-Pietu F, Robert M, Poncet G, Boulez J, Mion F (2012) Impaired postoperative EGJ relaxation as a determinant of post laparoscopic fundoplication dysphagia: a study with high-resolution manometry before and after surgery. Surg Endosc 26:3642–3649
Morgenthal CB, Lin E, Shane MD, Hunter JG, Smith CD (2007) Who will fail laparoscopic Nissen fundoplication? Preoperative prediction of long-term outcomes. Surg Endosc 21:1978–1984
Mughal MM, Bancewicz J, Marples M (1990) Oesophageal manometry and pH recording does not predict the bad results of Nissen fundoplication. Br J Surg 77:43–45
O’Riordan JM, Byrne PJ, Ravi N, Keeling PW, Reynolds JV (2004) Long-term clinical and pathologic response of Barrett’s esophagus after antireflux surgery. Am J Surg 188:27–33
Riedl O, Gadenstätter M, Lechner W, Schwab G, Marker M, Ciovica R (2009) Preoperative lower esophageal sphincter manometry data neither impact manifestations of GERD nor outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg 137:1189–1197
Schneider JH, Kramer KM, Konigsrainer A, Granderath FA (2007) The lower esophageal sphincter strength in patients with gastroesophageal reflux before and after laparoscopic Nissen fundoplication. Dis Esophagus 20:58–62
So JB, Zeitels SM, Rattner DW (1998) Outcomes of atypical symptoms attributed to gastroesophageal reflux treated by laparoscopic fundoplication. Surgery 124:28–32
Staehelin A, Zingg U, Devitt PG, Esterman AJ, Smith L, Jamieson GG, Watson DI (2014) Preoperative factors predicting clinical outcome following laparoscopic fundoplication. World J Surg 38:1431–1443
Stoikes N, Drapekin J, Kushnir V, Shaker A, Brunt LM, Gyawali CP (2012) The value of multiple rapid swallows during preoperative esophageal manometry before laparoscopic antireflux surgery. Surg Endosc 26:3401–3407
Tarnowski W, Kiciak A, Borycka-Kiciak K, Ciesielski A, Binda A, Dib N (2011) Laparoscopic fundoplication improves oesophageal motility: a prospective study. Wideochirurgia Inne Tech Maloinwazyjne 6:73–83
Thoman DS, Hui TT, Spyrou M, Phillips EH (2002) Laparoscopic antireflux surgery and its effect on cough in patients with gastroesophageal reflux disease. J Gastrointest Surg 6:17–21
Watson A, Spychal RT, Brown MG, Peck N, Callander N (1995) Laparoscopic “physiological” antireflux procedure: preliminary results of a prospective symptomatic and objective study. Br J Surg 82:651–656
Watson DI, Foreman D, Devitt PG, Jamieson GG (1997) Preoperative endoscopic grading of esophagitis versus outcome after laparoscopic Nissen fundoplication. Am J Gastroenterol 92:222–225
Wayman J, Myers JC, Jamieson GG (2007) Preoperative gastric emptying and patterns of reflux as predictors of outcome after laparoscopic fundoplication. Br J Surg 94:592–598
Weber B, Portnoy JE, Castellanos A, Hawkshaw MJ, Lurie D, Katz PO, Sataloff RT (2014) Efficacy of anti-reflux surgery on refractory laryngopharyngeal reflux disease in professional voice users: a pilot study. J Voice 28:492–500
Winslow ER, Clouse RE, Desai KM, Frisella P, Gunsberger T, Soper NJ, Klingensmith ME (2003) Influence of spastic motor disorders of the esophageal body on outcomes from laparoscopic antireflux surgery. Surg Endosc 17:738–745
Del Genio G, Tolone S, Del Genio F, Rossetti G, Brusciano L, Pizza F, Fei L, del Genio A (2008) Total fundoplication controls acid and nonacid reflux: Evaluation by pre- and postoperative 24-h pH-multichannel intraluminal impedance. Surg Endosc 22:2518–2523
del Genio G, Tolone S, del Genio F, Aggarwal R, d’Alessandro A, Allaria A, Rossetti G, Brusciano L, del Genio A (2008) Prospective assessment of patient selection for antireflux surgery by combined multichannel intraluminal impedance pH monitoring. J Gastrointest Surg 12:1491–1496
Asti E, Bonitta G, Lovece A, Lazzari V, Bonavina L (2016) Longitudinal comparison of quality of life in patients undergoing laparoscopic Toupet fundoplication versus magnetic sphincter augmentation: observational cohort study with propensity score analysis. Medicine (Baltimore) 95:e4366
Bonavina L, Horbach T, Schoppmann SF, DeMarchi J (2021) Three-year clinical experience with magnetic sphincter augmentation and laparoscopic fundoplication. Surg Endosc 35:3449–3458
Louie BE, Farivar AS, Shultz D, Brennan C, Vallières E, Aye RW (2014) Short-term outcomes using magnetic sphincter augmentation versus Nissen fundoplication for medically resistant gastroesophageal reflux disease. Ann Thorac Surg 98:498–504 (discussion 504-505)
Reynolds JL, Zehetner J, Wu P, Shah S, Bildzukewicz N, Lipham JC (2015) Laparoscopic magnetic sphincter augmentation vs laparoscopic nissen fundoplication: a matched-pair analysis of 100 patients. J Am Coll Surg 221:123–128
Richards WO, McRae C (2018) Comparative analysis of laparoscopic fundoplication and magnetic sphincter augmentation for the treatment of medically refractory GERD. Am Surg 84:1762–1767
Riegler M, Schoppman SF, Bonavina L, Ashton D, Horbach T, Kemen M (2015) Magnetic sphincter augmentation and fundoplication for GERD in clinical practice: one-year results of a multicenter, prospective observational study. Surg Endosc 29:1123–1129
Warren HF, Reynolds JL, Lipham JC, Zehetner J, Bildzukewicz NA, Taiganides PA, Mickley J, Aye RW, Farivar AS, Louie BE (2016) Multi-institutional outcomes using magnetic sphincter augmentation versus Nissen fundoplication for chronic gastroesophageal reflux disease. Surg Endosc 30:3289–3296
Reynolds JL, Zehetner J, Nieh A, Bildzukewicz N, Sandhu K, Katkhouda N, Lipham JC (2016) Charges, outcomes, and complications: a comparison of magnetic sphincter augmentation versus laparoscopic Nissen fundoplication for the treatment of GERD. Surg Endosc 30:3225–3230
Sheu E, Nau P, Nath B, Kuo B, Rattner D (2015) A comparative trial of laparoscopic magnetic sphincter augmentation and Nissen fundoplication. Surg Endosc 29:505–509
Ayazi S, Zaidi AH, Zheng P, Chovanec K, Chowdhury N, Salvitti M, Newhams K, Levy J, Hoppo T, Jobe BA (2020) Comparison of surgical payer costs and implication on the healthcare expenses between laparoscopic magnetic sphincter augmentation (MSA) and laparoscopic Nissen fundoplication (LNF) in a large healthcare system. Surg Endosc 34:2279–2286
Bell R, Lipham J, Louie B, Williams V, Luketich J, Hill M, Richards W, Dunst C, Lister D, McDowell-Jacobs L, Reardon P, Woods K, Gould J, Buckley FP 3rd, Kothari S, Khaitan L, Smith CD, Park A, Smith C, Jacobsen G, Abbas G, Katz P (2019) Laparoscopic magnetic sphincter augmentation versus double-dose proton pump inhibitors for management of moderate-to-severe regurgitation in GERD: a randomized controlled trial. Gastrointest Endosc 89:14-22.e1
Toomey P, Teta A, Patel K, Ross S, Sukharamwala P, Rosemurgy AS (2014) Transoral incisionless fundoplication: is it as safe and efficacious as a Nissen or Toupet fundoplication? Am Surg 80:860–867
Bell RCW, Freeman K, Heidrick R, Ayazi S (2021) Transoral incisionless fundoplication demonstrates durability at up to 9 years. Therap Adv Gastroenterol 14:17562848211004828
Testoni S, Hassan C, Mazzoleni G, Antonelli G, Fanti L, Passaretti S, Correale L, Cavestro GM, Testoni PA (2021) Long-term outcomes of transoral incisionless fundoplication for gastro-esophageal reflux disease: systematic-review and meta-analysis. Endosc Int Open 9:E239–E246
Ramai D, Shapiro A, Barakat M, Facciorusso A, Dull A, Chandan S, Adler DG (2022) Adverse events associated with transoral incisionless fundoplication (TIF) for chronic gastroesophageal reflux disease: a MAUDE database analysis. Surg Endosc 36:4956–4959
Håkansson B, Montgomery M, Cadiere GB, Rajan A, Bruley des Varannes S, Lerhun M, Coron E, Tack J, Bischops R, Thorell A, Arnelo U, Lundell L, (2015) Randomised clinical trial: transoral incisionless fundoplication vs. sham intervention to control chronic GERD. Aliment Pharmacol Ther 42:1261–1270
Hunter JG, Kahrilas PJ, Bell RC, Wilson EB, Trad KS, Dolan JP, Perry KA, Oelschlager BK, Soper NJ, Snyder BE, Burch MA, Melvin WS, Reavis KM, Turgeon DG, Hungness ES, Diggs BS (2015) Efficacy of transoral fundoplication vs omeprazole for treatment of regurgitation in a randomized controlled trial. Gastroenterology 148:324-333.e5
Trrad KS, Simoni G, Barnes WE, Shughoury AB, Raza M, Heise JA, Turgeon DG, Fox MA, Mavrelis PG (2014) Efficacy of transoral fundoplication for treatment of chronic gastroesophageal reflux disease incompletely controlled with high-dose proton-pump inhibitors therapy: a randomized, multicenter, open label, crossover study. BMC Gastroenterol 14:174
Witteman BP, Conchillo JM, Rinsma NF, Betzel B, Peeters A, Koek GH, Stassen LP, Bouvy ND (2015) Randomized controlled trial of transoral incisionless fundoplication vs. proton pump inhibitors for treatment of gastroesophageal reflux disease. Am J Gastroenterol 110:531–542
Hu ZW, Wang ZG, Zhang Y, Wu JM, Liang WT, Yang Y, Tian SR, Wang AE (2014) A preliminary investigation of anti-reflux intervention for gastroesophageal reflux related childhood-to-adult persistent asthma. Ann Surg Innov Res 8:3
Ma L, Li T, Liu G, Wang J, Yin Z, Kang J (2020) Stretta radiofrequency treatment vs Toupet fundoplication for gastroesophageal reflux disease: a comparative study. BMC Gastroenterol 20:162
Liang W, Wu J, Hu Z, Wang Z, Zhu G, Zhang C (2014) Laparoscopic Nissen fundoplication is more effective intreating patients with GERD-related chronic cough than Stretta radiofrequency. Minerva Chir 69:121–127
Yan C, Liang WT, Wang ZG, Hu ZW, Wu JM, Zhang C, Chen MP (2015) Comparison of Stretta procedure and toupet fundoplication for gastroesophageal reflux disease-related extra-esophageal symptoms. World J Gastroenterol 21:12882–12887
Richards WO, Houston HL, Torquati A, Khaitan L, Holzman MD, Sharp KW (2003) Paradigm shift in the management of gastroesophageal reflux disease. Ann Surg 237:638–647 (discussion 648-649)
Liang WT, Yan C, Wang ZG, Wu JM, Hu ZW, Zhan XL, Wang F, Ma SS, Chen MP (2015) Early and midterm outcome after laparoscopic fundoplication and a minimally invasive endoscopic procedure in patients with gastroesophageal reflux disease: a prospective observational study. J Laparoendosc Adv Surg Tech A 25:657–661
Zhang C, Wu J, Hu Z, Yan C, Gao X, Liang W, Liu D, Li F, Wang Z (2016) Diagnosis and anti-reflux therapy for GERD with respiratory symptoms: a study using multichannel intraluminal impedance-pH monitoring. PLoS ONE 11:e0160139
Liang WT, Wu JN, Wang F, Hu ZW, Wang ZG, Ji T, Zhan XL, Zhang C (2014) Five-year follow-up of a prospective study comparing laparoscopic Nissen fundoplication with Stretta radiofrequency for gastroesophageal reflux disease. Minerva Chir 69:217–223
Arts J, Bisschops R, Blondeau K, Farré R, Vos R, Holvoet L, Caenepeel P, Lerut A, Tack J (2012) A double-blind sham-controlled study of the effect of radiofrequency energy on symptoms and distensibility of the gastro-esophageal junction in GERD. Am J Gastroent 107:222–230
Aziz AM, El-Khayat HR, Sadek A, Mattar SG, McNulty G, Kongkam P, Guda MF, Lehman GA (2010) A prospective randomized trial of sham, single-dose Stretta, and double-dose Stretta for the treatment of gastroesophageal reflux disease. Surg Endosc 24:818–825
Coron E, Sebille V, Cadiot G, Zerbib F, Ducrotte P, Ducrot F, Pouderoux P, Arts J, Le Rhun M, Piche T, Bruley des Varannes S, Galmiche JP, (2008) Clinical trial: Radiofrequency energy delivery in proton pump inhibitor-dependent gastro-oesophageal reflux disease patients. Aliment Pharmacol Ther 28:1147–1158
Zerbib F, Sacher-Huvelin S, Coron E, Coffin B, Melchior C, Ponchon T, Cholet F, Chabrun E, Vavasseur F, Gorbatchef C, Zalar A, Mion F, Robaszkiewicz M, Le Rhun M, Leroy M, Paul Galmiche J, Bruley des Varannes S, (2020) Randomised clinical trial: oesophageal radiofrequency energy delivery versus sham for PPI-refractory heartburn. Aliment Pharmacol Ther 52:637–645
Kalapala R, Shah H, Nabi Z, Darisetty S, Talukdar R, Nageshwar Reddy D (2017) Treatment of gastroesophageal reflux disease using radiofrequency ablation (Stretta procedure): an interim analysis of a randomized trial. Indian J Gastroenterol 36:337–342
Spence GM, Watson DI, Jamiesion GG, Lally CJ, Devitt PG (2006) Single center prospective randomized trial of laparoscopic Nissen versus anterior 90° fundoplication. J Gastroint Surg 10:698–705
Koch OO, Kaindlstorfer A, Antoniou SA, Luketina RR, Emmanuel K, Pointner R (2013) Comparison of results from a randomized trial 1 year after laparoscopic Nissen and Toupet fundoplications. Surg Endosc 27:2383–2390
Mickevicius A, Endzinas Z, Kiudelis M, Jonaitis L, Kupcinskas L, Maleckas A, Pundzius J (2008) Influence of wrap length on the effectiveness of Nissen and Toupet fundoplication: a prospective randomized study. Surg Endosc 22:2269–2276
Cai W, Qin MF, Zou FS, Li DY (2012) Five-year efficacy of laparoscopic Nissen fundoplication versus anterior 180° partial fundoplication in the management of reflux esophagitis: A randomized controlled trial. World Chin J Digestol 20:1234–1237
Cai W, Watson DI, Lally CJ, Devitt PG, Game PA, Jamieson GG (2008) Ten-year clinical outcome of a prospective randomized clinical trial of laparoscopic Nissen versus anterior 180 (degrees) partial fundoplication. Br J Surg 95:1501–1505
Zornig C, Strate U, Fibbe C, Emmermann A, Layer P (2002) Nissen vs Toupet laparoscopic fundoplication. Surg Endosc 16:758–766
Hopkins RJ, Irvine T, Jamieson GG, Devitt PG, Watson DI (2020) Long-term follow-up of two randomized trials comparing laparoscopic Nissen 360° with anterior 90° partial fundoplication. Br J Surg 107:56–63
Wang B, Zhang W, Liu S, Du Z, Shan C, Qiu M (2015) A Chinese randomized prospective trial of floppy Nissen and Toupet fundoplication for gastroesophageal disease. Int J Surg 23:35–40
Djerf P, Montgomery A, Hallerbäck B, Håkansson HO, Johnsson F (2016) One- and ten-year outcome of laparoscopic anterior 120° versus total fundoplication: a double-blind, randomized multicenter study. Surg Endosc 30:168–177
Rudolph-Stringer V, Bright T, Irvine T, Thompson SK, Devitt PG, Game PA, Jamieson GG, Watson DI (2020) Randomized trial of laparoscopic nissen vs. anterior 180 degree partial fundoplication - late clinical outcomes at 15–20 years. Ann Surg 275:39–44
Watson DI, Devitt PG, Smith L, Jamieson GG (2012) Anterior 90 degrees partial vs Nissen fundoplication–5 year follow-up of a single-centre randomised trial. J Gastrointest Surg 16:1653–1658
Baigrie RJ, Cullis SN, Ndhluni AJ, Cariem A (2005) Randomized double-blind trial of laparoscopic Nissen fundoplication versus anterior partial fundoplication. Br J Surg 92:819–823
Raue W, Ordemann J, Jacobi CA, Menenakos C, Buchholz A, Hartmann J (2011) Nissen versus Dor fundoplication for treatment of gastroesophageal reflux disease: a blinded randomized clinical trial. Dig Surg 28:80–86
Strate U, Emmermann A, Fibbe C, Layer P, Zornig C (2008) Laparoscopic fundoplication: Nissen versus Toupet two-year outcome of a prospective randomized study of 200 patients regarding preoperative esophageal motility. Surg Endosc 22:21–30
Booth MI, Stratford J, Jones L, Dehn TC (2008) Randomized clinical trial of laparoscopic total (Nissen) versus posterior partial (Toupet) fundoplication for gastro-oesophageal reflux disease based on preoperative oesophageal manometry. Br J Surg 95:57–63
Laws HL, Clements RH, Swillie CM (1997) A randomized, prospective comparison of the Nissen fundoplication versus the Toupet fundoplication for gastroesophageal reflux disease. Ann Surg 225:647–653 (discussion 654)
Khan MA, Smythe A, Globe J, Stoddard CJ, Ackroyd R (2009) Randomized controlled trial of laparoscopic Nissen versus Lind fundoplication for gastro-oesophageal reflux disease. Scand J Gastroenterol 44:269–275
Mardani J, Lundell L, Engstrom C (2011) Total or posterior partial fundoplication in the treatment of GERD: results of a randomized trial after 2 decades of follow-up. Ann Surg 253:875–878
Guérin E, Bétroune K, Closset J, Mehdi A, Lefèbvre JC, Houben JJ, Gelin M, Vaneukem P, El Nakadi I (2007) Nissen versus Toupet fundoplication: results of a randomized and multicenter trial. Surg Endosc 21:1985–1990
Nijjar RS, Watson DI, Jamieson GG, Archer S, Bessell JR, Booth M, Cade R, Cullingford GL, Devitt PG, Fletcher DR, Hurley J, Kiroff G, Martin IJ, Nathanson LK, Windsor JA; International Society for the Diseases of the Esophagus-Australasian Section (2010) Five-year follow-up of a multicenter, double-blind randomized clinical trial of laparoscopic Nissen vs anterior 90 degrees partial fundoplication. Arch Surg 145:552–557
Shaw JM, Bornman PC, Callanan MD, Beckingham IJ, Metz DC (2010) Long-term outcome of laparoscopic Nissen and laparoscopic Toupet fundoplication for gastroesophageal reflux disease: a prospective, randomized trial. Surg Endosc 24:924–932
Cao Z, Cai W, Qin M, Zhao H, Yue P, Li Y (2012) Randomized clinical trial of laparoscopic anterior 180 degrees partial versus 360 degrees Nissen fundoplication: 5-year results. Dis Esophagus 25:114–120
Mickevičius A, Endzinas Ž, Kiudelis M, Jonaitis L, Kupčinskas L, Pundzius J, Maleckas A (2013) Influence of wrap length on the effectiveness of Nissen and Toupet fundoplications: 5-year results of prospective, randomized study. Surg Endosc 27:986–991
Bell RC, Hanna P, Powers B, Sabel J, Hruza D (1996) Clinical and manometric results of laparoscopic partial (Toupet) and complete (Rosetti-Nissen) fundoplication. Surg Endosc 10:724–728
Broeders JA, Bredenoord AJ, Hazebroek EJ, Broeders IA, Gooszen HG, Smout AJ (2012) Reflux and belching after 270 degree versus 360 degree laparoscopic posterior fundoplication. Ann Surg 255:59–65
Dallemagne B, Weerts J, Markiewicz S, Dewandre JM, Wahlen C, Monami B, Jehaes C (2006) Clinical results of laparoscopic fundoplication at ten years after surgery. Surg Endosc 20:159–165
Erenoglu C, Miller A, Schirmer B (2003) Laparoscopic Toupet versus Nissen fundoplication for the treatment of gastroesophageal reflux disease. Int Surg 88:219–225
Farrell TM, Archer SB, Galloway KD, Branum GD, Smith CD, Hunter JG (2000) Heartburn is more likely to recur after Toupet fundoplication than Nissen fundoplication. Am Surg 66:229–236 (discussion 236-237)
Fernando HC, Luketich JD, Christie NA, Ikramuddin S, Schauer PR (2002) Outcomes of laparoscopic Toupet compared to laparoscopic Nissen fundoplication. Surg Endosc 16:905–908
Gunter RL, Shada AL, Funk LM, Wang X, Greenberg JA, Lidor AO (2017) Long-term quality of life outcomes following nissen versus toupet fundoplication in patients with gastroesophageal reflux disease. J Laparoendosc Adv Surg Tech A 27:931–936
Hafez J, Wrba F, Lenglinger J, Miholic J (2008) Fundoplication for gastroesophageal reflux and factors associated with the outcome 6 to 10 years after the operation: multivariate analysis of prognostic factors using the propensity score. Surg Endosc 22:1763–1768
Hoshino M, Omura N, Yano F, Tsuboi K, Yamamoto SR, Akimoto S, Mitsumori N, Kashiwagi H, Yanaga K (2017) Comparison of laparoscopic Nissen and Toupet fundoplication using a propensity score matching analysis. Surg Today 47:1195–1200
Karim SS, Panton ON, Finley RJ, Graham AJ, Dong S, Storseth C, Clifton J (1997) Comparison of total versus partial laparoscopic fundoplication in the management of gastroesophageal reflux disease. Am J Surg 173:375–378
Lal P, Shah SH, Leekha N, Puri AS (2017) Laparoscopic anterior partial fundoplication is comparable with nissen fundoplication for gastroesophageal reflux disease. Surg Laparosc Endosc Percutan Tech 27:24–29
Livingston CD, Jones HL Jr, Askew RE Jr, Victor BE, Askew RE Sr (2001) Laparoscopic hiatal hernia repair in patients with poor esophageal motility or paraesophageal herniation. Am Surg 67:987–991
McKernan JB (1994) Laparoscopic repair of gastroesophageal reflux disease. Toupet partial fundoplication versus Nissen fundoplication. Surg Endosc 8:851–856
Nicolau AE, Crăciun M, Zota R, Kitkani A (2013) Quality of life after laparoscopic fundoplication for gastroesophageal reflux disease. Preliminary Study Chirurgia (Bucur) 108:788–793
Papasavas PK, Keenan RJ, Yeaney WW, Caushaj PF, Gagné DJ, Landreneau RJ (2003) Effectiveness of laparoscopic fundoplication in relieving the symptoms of gastroesophageal reflux disease (GERD) and eliminating antireflux medical therapy. Surg Endosc 17:1200–1205
Patti MG, Arcerito M, Feo CV, De Pinto M, Tong J, Gantert W, Tyrrell D, Way LW (1998) An analysis of operations for gastroesophageal reflux disease: identifying the important technical elements. Arch Surg 133:600–606 (discussion 606-607)
Patti MG, De Pinto M, De Bellis M, Arcerito M, Tong J, Wang A, Mulvihill SJ, Way LW (1997) Comparison of laparoscopic total and partial fundoplication for gastroesophageal reflux. J Gastrointest Surg 1:309–315
Patti MG, Robinson T, Galvani C, Gorodner MV, Fisichella PM, Way LW (2004) Total fundoplication is superior to partial fundoplication even when esophageal peristalsis is weak. J Am Coll Surg 198:863–869 (discussion 869-870)
Pessaux P, Arnaud JP, Delattre JF, Meyer C, Baulieux J, Mosnier H (2005) Laparoscopic antireflux surgery: five-year results and beyond in 1340 patients. Arch Surg 140:946–951
Pessaux P, Arnaud JP, Ghavami B, Flament JB, Trebuchet G, Meyer C, Huten N, Champault G (2000) Laparoscopic antireflux surgery: comparative study of Nissen, Nissen-Rossetti, and Toupet fundoplication. Surg Endosc 14:1024–1027
Qin M, Ding G, Yang H (2013) A clinical comparison of laparoscopic nissen and toupet fundoplication for gastroesophageal reflux disease. J Laparoendosc Adv Surg Tech A 23:601–604
Radajewski R, Hazebroek EJ, Berry H, Leibman S, Smith GS (2009) Short-term symptom and quality-of-life comparison between laparoscopic Nissen and Toupet fundoplications. Dis Esophagus 22:84–88
Robertson AG, Patel RN, Couper GW, de Beaux AC, Paterson-Brown S, Lamb PJ (2017) Long-term outcomes following laparoscopic anterior and Nissen fundoplication. ANZ J Surg 87:300–304
Ruiz-Tovar J, Diez-Tabernilla M, Chames A, Morales V, Martinez-Molina E (2010) Clinical outcome at 10 years after laparoscopic versus open Nissen fundoplication. J Laparoendosc Adv Surg Tech A 20:21–23
Sgromo B, Irvine LA, Cuschieri A, Shimi SM (2008) Long-term comparative outcome between laparoscopic total Nissen and Toupet fundoplication: symptomatic relief, patient satisfaction and quality of life. Surg Endosc 22:1048–1053
Stewart GD, Watson AJ, Lamb PJ, Lee AJ, Krukowski ZH, Griffin SM, Paterson-Brown S (2004) Comparison of three different procedures for antireflux surgery. Br J Surg 91:724–749
Toydemir T, Tekin K, Yerdel MA (2011) Laparoscopic Nissen versus Toupet fundoplication: assessment of operative outcomes. J Laparoendosc Adv Surg Tech A 21:669–676
Walle KV, Funk LM, Xu Y, Davies KD, Greenberg J, Shada A, Lidor A (2019) Persistent dysphagia rate after antireflux surgery is similar for nissen fundoplication and partial fundoplication. J Surg Res 235:52–57
Wong AS, Myers JC, Jamieson GG (2008) Esophageal pH profile following laparoscopic total fundoplication compared to anterior fundoplication. J Gastrointest Surg 12:1341–1345
Wykypiel H, Gadenstaetter M, Klaus A, Klingler P, Wetscher GJ (2005) Nissen or partial posterior fundoplication: which antireflux procedure has a lower rate of side effects? Langenbecks Arch Surg 390:141–147
Zügel N, Jung C, Bruer C, Sommer P, Breitschaft K (2002) A comparison of laparoscopic Toupet versus Nissen fundoplication in gastroesophageal reflux disease. Langenbecks Arch Surg 386:494–498
Oleynikov D, Eubanks TR, Oelschlager BK, Pellegrini CA (2002) Total fundoplication is the operation of choice for patients with gastroesophageal reflux and defective peristalsis. Surg Endosc 16:909–913
Gyawali CP, Sifrim D, Carlson DA, Hawn M, Katzka DA, Pandolfino JE, Penagini R, Roman S, Savarino E, Tatum R, Vaezi M, Clarke JO, Triadafilopoulos G (2019) Ineffective esophageal motility: Concepts, future directions, and conclusions from the Stanford 2018 symposium. Neurogastroenterol Motil 31:e13584
Braghetto I, Korn O, Csendes A, Gutiérrez L, Valladares H, Chacon M (2012) Laparoscopic treatment of obese patients with gastroesophageal reflux disease and Barrett’s esophagus: a prospective study. Obes Surg 22:764–772
Patterson EJ, Davis DG, Khajanchee Y, Swanström LL (2003) Comparison of objective outcomes following laparoscopic Nissen fundoplication versus laparoscopic gastric bypass in the morbidly obese with heartburn. Surg Endosc 17:1561–1565
Anvari M, Bamehriz F (2006) Outcome of laparoscopic Nissen fundoplication in patients with body mass index > 35. Surg Endosc 20:230–234
Martin del Campo SE, Chaudhry UI, Kanji A, Suzo AJ, Perry KA (2017) Laparoscopic Nissen fundoplication controls reflux symptoms and improves disease-specific quality of life in patients with class I and II obesity. Surgery 162:1048–1054
Telem DA, Altieri M, Gracia G, Pryor AD (2014) Perioperative outcome of esophageal fundoplication for gastroesophageal reflux disease in obese and morbidly obese patients. Am J Surg 208:163–168
Clements RH, Gonzalez QH, Foster A, Richards WO, McDowell J, Bondora A, Laws HL (2003) Gastrointestinal symptoms are more intense in morbidly obese patients and are improved with laparoscopic Roux-en-Y gastric bypass. Obes Surg 13:610–614
Csendes A, Burgos AM, Smok G, Burdiles P, Henriquez A (2006) Effect of gastric bypass on Barrett’s esophagus and intestinal metaplasia of the cardia in patients with morbid obesity. J Gastrointest Surg 10:259–264
Holmberg D, Santoni G, Xie S, Lagergren J (2019) Gastric bypass surgery in the treatment of gastro-oesophageal reflux symptoms. Aliment Pharmacol Ther 50:159–166
Madalosso CA, Gurski RR, Callegari-Jacques SM, Navarini D, Mazzini G, Pereira Mda S (2016) The impact of gastric bypass on gastroesophageal reflux disease in morbidly obese patients. Ann Surg 263:110–116
Madalosso CA, Gurski RR, Callegari-Jacques SM, Navarini D, Thiesen V, Fornari F (2010) The impact of gastric bypass on gastroesophageal reflux disease in patients with morbid obesity: a prospective study based on the Montreal Consensus. Ann Surg 251:244–248
Mejía-Rivas MA, Herrera-López A, Hernández-Calleros J, Herrera MF, Valdovinos MA (2008) Gastroesophageal reflux disease in morbid obesity: the effect of Roux-en-Y gastric bypass. Obes Surg 18:1217–1224
Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J (2000) Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg 232:515–529
Luketina R-R, Koch OO, Köhler G, Antoniou SA, Emmanuel K, Pointner R (2015) Obesity does not affect the outcome of laparoscopic antireflux surgery. Surg Endosc 29:1327–1333
Sanford Z, Jayaraman S, Weltz AS, Reza Zahiri H, Park A (2020) The role of body mass index in determining clinical and quality of life outcomes after laparoscopic anti-reflux surgery. Surg Endosc 34:646–657
Borbély Y, Kröll D, Nett PC, Moreno P, Tutuian R, Lenglinger J (2016) Radiologic, endoscopic, and functional patterns in patients with symptomatic gastroesophageal reflux disease after Roux-en-Y gastric bypass. Surg Obes Relat Dis 14:764–768
Stefanidis D, Hope WW, Kohn GP, Reardon PR, Richardson WS, Fanelli RD, Guidelines Committee SAGES (2010) Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc 24:2647–2669
Perez AR, Moncure AC, Rattner DW (2001) Obesity adversely affects the outcome of antireflux operations. Surg Endosc 15:986–989
Ng VV, Booth MI, Stratford JJ, Jones L, Sohanpal J, Dehn TCB (2007) Laparoscopic anti-reflux surgery is effective in obese patients with gastro-oesophageal reflux disease. Ann R Coll Surg Engl 89:696–702
Iqbal A, Kakarlapudi GV, Awad ZT, Haynatzki G, Turaga KK, A, Fritz K, Haider M, Mittal SK, Filipi CJ, (2006) Assessment of diaphragmatic stressors as risk factors for symptomatic failure of laparoscopic nissen fundoplication. J Gastrointest Surg 10:12–21
Arman GA, Himpens J, Dhaenens J, Ballet T, Vilallonga R, Leman G (2016) Long-term (11+years) outcomes in weight, patient satisfaction, comorbidities, and gastroesophageal reflux treatment after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis 12:1778–1786
Chopra A, Chao E, Etkin Y, Merklinger L, Lieb J, Delany H (2012) Laparoscopic sleeve gastrectomy for obesity: can it be considered a definitive procedure? Surg Endosc 26:831–837
Daes J, Jimenez ME, Said N, Daza JC, Dennis R (2012) Laparoscopic sleeve gastrectomy: symptoms of gastroesophageal reflux can be reduced by changes in surgical technique. Obes Surg 22:1874–1879
Daes J, Jimenez ME, Said N, Dennis R (2014) Improvement of gastroesophageal reflux symptoms after standardized laparoscopic sleeve gastrectomy. Obes Surg 24:536–540
Dimbezel V, Nedelcu A, Danan M, Carandina S, Collet D, Gronnier C, Nedelcu M (2020) Endoscopic findings 5 years following sleeve gastrectomy. Obes Surg 30:3847–3851
Gorodner V, Buxhoeveden R, Clemente G, Solé L, Caro L, Grigaites A (2015) Does laparoscopic sleeve gastrectomy have any influence on gastroesophageal reflux disease? Preliminary results. Surg Endosc 29:1760–1768
Hendricks L, Alvarenga E, Dhanabalsamy N, Lo Menzo E, Szomstein S, Rosenthal R (2016) Impact of sleeve gastrectomy on gastroesophageal reflux disease in a morbidly obese population undergoing bariatric surgery. Surg Obes Relat Dis 12:511–517
Howard DD, Caban AM, Cendan JC, Ben-David K (2011) Gastroesophageal reflux after sleeve gastrectomy in morbidly obese patients. Surg Obes Relat Dis 7:709–713
Sucandy I, Chrestiana D, Bonanni F, Antanavicius G (2015) Gastroesophageal reflux symptoms after laparoscopic sleeve gastrectomy for morbid obesity. The importance of preoperative evaluation and selection. N Am J Med Sci 7:189–193
Felsenreich DM, Langer F, Kefurt R, Panhofer P, Schermann M, Beckerhinn P, Sperker C, Prager G (2016) Weight loss, weight regain, and conversions to Roux-en-Y gastric bypass: 10-year results of laparoscopic sleeve gastrectomy. Surg Obes Relat Dis 12:1655–1662
Mandeville Y, Van Looveren R, Vancoillie PJ, Verbeke X, Vandendriessche K, Vuylsteke P, Pattyn P, Smet B (2017) Moderating the enthusiasm of sleeve gastrectomy: up to fifty percent of reflux symptoms after ten years in a consecutive series of one hundred laparoscopic sleeve gastrectomies. Obes Surg 27:1797–1803
Carter PR, LeBlanc KA, Hausmann MG, Kleinpeter KP, deBarros SN, Jones SM (2011) Association between gastroesophageal reflux disease and laparoscopic sleeve gastrectomy. Surg Obes Relat Dis 7:569–572
Tai CM, Huang CK, Lee YC, Chang CY, Lee CT, Lin JT (2013) Increase in gastroesophageal reflux disease symptoms and erosive esophagitis 1 year after laparoscopic sleeve gastrectomy among obese adults. Surg Endosc 27:1260–1266
Althuwaini S, Bamehriz F, Aldohayan A, Alshammari W, Alhaidar S, Alotaibi M, Alanazi A, Alsahabi H, Almadi MA (2018) Prevalence and predictors of gastroesophageal reflux disease after laparoscopic sleeve gastrectomy. Obes Surg 28:916–922
Stenard F, Iannelli A (2015) Laparoscopic sleeve gastrectomy and gastroesophageal reflux. World J Gastroenterol 21:10348–10357
Sancho Moya C, Bruna Esteban M, Sempere García-Argüelles J, Ferrer Barceló L, Monzó Gallego A, Mirabet Sáez B, Mulas Fernández C, Albors Bagá P, Vázquez Prado A, Oviedo Bravo M, Montalvá Orón E (2022) The impact of sleeve gastrectomy on gastroesophageal reflux disease in patients with morbid obesity. Obes Surg 32:615–624
Laffin M, Chau J, Gill RS, Birch DW, Karmali S (2013) Sleeve gastrectomy and gastroesophageal reflux disease. J Obes 2013:741097
Antiporda M, Jackson C, Smith CD, Thomas M, Elli EF, Bowers SP (2019) Strategies for surgical remediation of the multi-fundoplication failure patient. Surg Endosc 33:1474–1481
Mittal SK, Légner A, Tsuboi K, Juhasz A, Bathla L, Lee TH (2013) Roux-en-Y reconstruction is superior to redo fundoplication in a subset of patients with failed antireflux surgery. Surg Endosc 27:927–935
Shao JM, Elhage SA, Prasad T, Gersin K, Augenstein VA, Colavita PD, Heniford BT (2021) Best reoperative strategy for failed fundoplication: redo fundoplication or conversion to Roux-en-Y gastric diversion? Surg Endosc 35:3865–3873
Weber CE, Kanani Z, Schumm M, Helm M, Gould JC (2019) Roux-en-Y gastric bypass as a salvage procedure in complicated patients with failed fundoplication(s). Surg Endosc 33:738–744
Yamamoto SR, Hoshino M, Nandipati KC, Lee TH, Mittal SK (2014) Long-term outcomes of reintervention for failed fundoplication: redo fundoplication versus Roux-en-Y reconstruction. Surg Endosc 28:42–48
Baretta G, Al-Mulla AE, Lopes MAG, Feistler RS, Cambi MPC, de Paula LM (2020) Laparoscopic Roux-en-Y gastric bypass after gastroesophageal reflux disease surgical procedure: analysis of 85 consecutive patients with pre- and post-operative endoscopy control. J Laparoendosc Adv Surg Tech A 30:40–43
Kellogg TA, Andrade R, Maddaus M, Slusarek B, Buchwald H, Ikramuddin S (2007) Anatomic findings and outcomes after antireflux procedures in morbidly obese patients undergoing laparoscopic conversion to Roux-en-Y gastric bypass. Surg Obes Relat Dis 3:52–57 (discussion 58-59)
Slater BJ, Dirks RC, McKinley SK, Ansari MT, Kohn GP, Thosani N, Qumseya B, Billmeier S, Daly S, Crawford C, Ehlers P, A, Hollands C, Palazzo F, Rodriguez N, Train A, Wassenaar E, Walsh D, Pryor AD, Stefanidis D, (2021) SAGES guidelines for the surgical treatment of gastroesophageal reflux (GERD). Surg Endosc 35:4903–4949
Acknowledgements
We would like to thank Jillian Kelly, the SAGES senior program coordinator, Holly Burt, the SAGES librarian, and the SAGES guideline committee members for their help with the creation of this guideline.
Funding
There was no funding for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
BS—Consultant for Hologic and Cook Medical, AC, APQ, MRR, SK, EC, SW, AAS, MTA, DIA, SD, FD, JH, KK, AL, MD, VL, DL, AP,CW,GPK, RV, AT—no conflicts of interest, RD—Personal stock in Johnson and Johnson, JCG—Preceptor for Ethicon/J + J, Speaker for BD, RJ—Speaker for Medtronic, Intuitive Surgical, and Aspire Medical, Consultant for Intuitive Surgical, Expert Review for BSPH Law, INH—Royalty for uptoDate. ISS—Proctor for Intuitive Surgical, NT—Consultant for Boston Scientific Corp, Pentax America, Ambu, Biotex Inc, Speaker for Abbvie, Royalty for UpToDate, Creatorship Rights for ROSEAID inc, VV—Advisory board and speaker for Integra Biosciences, Consultant for Innocoll Pharmaceuticals, Inc., and Proctor for Linx/Johnson & Johnson, JMM—Consultant for Boston Scientific, and US Endoscopy.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Slater, B.J., Collings, A., Dirks, R. et al. Multi-society consensus conference and guideline on the treatment of gastroesophageal reflux disease (GERD). Surg Endosc 37, 781–806 (2023). https://doi.org/10.1007/s00464-022-09817-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09817-3