Abstract
Introduction
While it is well established that antireflux surgery is effective in relieving typical gastroesophageal reflux disease (GERD) symptoms such as heartburn and regurgitation, it is currently unclear whether atypical symptoms (cough, hoarseness, wheeze) foreshadow a less satisfactory outcome following laparoscopic antireflux surgery (LARS). The purpose of this study is to critically analyze the clinical outcomes of atypical symptoms in patients undergoing LARS.
Methods
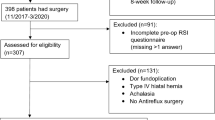
Patients scheduled for LARS for GERD were prospectively enrolled over a 7-year period; all subjects underwent preoperative high-resolution manometry (HRM) and had evidence of GERD on ambulatory pH study. Cough, wheeze, and hoarseness were considered atypical symptoms. During preoperative and postoperative examinations, patients completed detailed foregut symptomatology questionnaires, using both 5-point Likert and 10-point visual analog scales (VAS) to document typical as well as atypical symptoms. Atypical symptom burden was calculated as a sum of VAS for the three atypical symptoms, termed the atypical score (ATS). HRM patterns were grouped into normal, spastic, and hypomotile. Statistical significance (p < 0.05) was determined using paired t-test, and analysis of variance with post hoc least significant difference (LSD).
Results
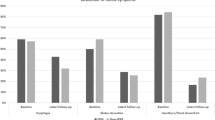
One hundred thirteen patients (age 49 ± 1.26 years, range 20–84 years, M:F 47:66) with mean follow-up of 28 ± 2.31 months (range 1–92 months) fulfilled inclusion criteria, having mean modified DeMeester score of 45.5 ± 2.78. Heartburn was noted in 84.1%, while atypical symptoms of some degree were reported by 92.0% (104 patients). Heartburn improved from a preoperative score of 7.1 ± 0.54 to 0.9 ± 0.24 after LARS, and ATS improved from 8.9 ± 0.71 to 2.2 ± 0.42. Significant improvements were noted for all atypical symptoms analyzed (p < 0.0001 for each). Improvement in atypical symptoms was least in the presence of hypomotility features on HRM (21.7% improvement), compared with normal motility (72.4%) and spastic features (83.9%). Preoperative atypical score (p < 0.0001) and esophageal hypomotility (p = 0.04) demonstrated a linear relationship with postoperative atypical score.
Conclusions
In an unselected cohort of patients undergoing LARS, atypical GERD symptoms improved as significantly as typical symptoms. Symptom improvement was significantly lower in the presence of esophageal hypomotility and with higher symptomatic state. Therefore, patients with severe atypical symptoms or hypomotile esophagus may not achieve the same clinical satisfaction from LARS.

Similar content being viewed by others
References
Spechler SJ et al (2001) Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: follow-up of a randomized controlled trial. JAMA 285(18):2331–2338
Peters JH et al (1998) The treatment of gastroesophageal reflux disease with laparoscopic Nissen fundoplication: prospective evaluation of 100 patients with “typical” symptoms. Ann Surg 228(1):40–50
Oelschlager BK et al (2008) Long-term outcomes after laparoscopic antireflux surgery. Am J Gastroenterol 103(2):280–287 (quiz 288)
Gee DW, Andreoli MT, Rattner DW (2008) Measuring the effectiveness of laparoscopic antireflux surgery: long-term results. Arch Surg 143(5):482–487
Fein M et al (2008) Ten-year outcome of laparoscopic antireflux surgery. J Gastrointest Surg 12(11):1893–1899
Power C, Maguire D, McAnena O (2004) Factors contributing to failure of laparoscopic Nissen fundoplication and the predictive value of preoperative assessment. Am J Surg 187(4):457–463
Chin KF et al (2008) Symptoms experienced during 24-h pH monitoring and their relationship to outcome after laparoscopic total fundoplication. Dis Esophagus 21(5):445–451
Velanovich V, Mahatme A (2004) Effects of manometrically discovered nonspecific motility disorders of the esophagus on the outcomes of antireflux surgery. J Gastrointest Surg 8(3):335–341
Laine S et al (1997) Laparoscopic vs conventional Nissen fundoplication. A prospective randomized study. Surg Endosc 11(5):441–444
Richardson WS, Trus TL, Hunter JG (1996) Laparoscopic antireflux surgery. Surg Clin North Am 76(3):437–450
Richter JE (2005) Review article: extraoesophageal manifestations of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 22 Suppl 1:70–80
Allen CJ, Anvari M (2004) Does laparoscopic fundoplication provide long-term control of gastroesophageal reflux related cough? Surg Endosc 18(4):633–637
Pauwels A et al (2009) Cough and gastroesophageal reflux: from the gastroenterologist end. Pulm Pharmacol Ther 22(2):135–138
Tutuian R et al (2006) Nonacid reflux in patients with chronic cough on acid-suppressive therapy. Chest 130(2):386–391
Patterson N et al (2009) Nonacid reflux episodes reaching the pharynx are important factors associated with cough. J Clin Gastroenterol 43(5):414–419
Kushnir VM, Sayuk GS, Gyawali CP (2010) Abnormal GERD parameters on ambulatory pH monitoring predict therapeutic success in noncardiac chest pain. Am J Gastroenterol 105(5):1032–1038
Hersh MJ, Sayuk GS, Gyawali CP (2010) Long-term therapeutic outcome of patients undergoing ambulatory pH monitoring for chronic unexplained cough. J Clin Gastroenterol 44(4):254–260
Banos JE et al (1989) Acceptability of visual analogue scales in the clinical setting: a comparison with verbal rating scales in postoperative pain. Methods Find Exp Clin Pharmacol 11(2):123–127
Ayazi S, Crookes PF (2009) High-resolution esophageal manometry: using technical advances for clinical advantages. J Gastrointest Surg
DeMeester TR et al (1990) Chronic respiratory symptoms and occult gastroesophageal reflux. A prospective clinical study and results of surgical therapy. Ann Surg 211(3):337–345
Chen RY, Thomas RJ (2000) Results of laparoscopic fundoplication where atypical symptoms coexist with oesophageal reflux. Aust N Z J Surg 70(12):840–842
Farrell TM et al (2001) Response of atypical symptoms of gastro-oesophageal reflux to antireflux surgery. Br J Surg 88(12):1649–1652
Horvath KD et al (1999) Laparoscopic Toupet fundoplication is an inadequate procedure for patients with severe reflux disease. J Gastrointest Surg 3(6):583–591
Winslow ER et al (2003) Influence of spastic motor disorders of the esophageal body on outcomes from laparoscopic antireflux surgery. Surg Endosc 17(5):738–745
Disclosures
Authors Brown, Gyawali, Melman, Jenkins, Bader, and Frisella have no conflicts of interest or financial ties to disclose relevant to this work. Author Eagon is a consultant for Ethicon Endosurgical. Author Brunt has received educational grants and research support from Ethicon Endosurgical, Karl Storz Endoscopy, Stryker Endoscopy, Lifecell, and an honorarium for speaking from Ethicon EndoSurgery. Author Matthews has received consulting fees from Atrium Medical, Ethicon EndoSurgery, and Muskuloskeletal Transplant Foundation, and an honorarium for speaking from W.L. Gore.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brown, S.R., Gyawali, C.P., Melman, L. et al. Clinical outcomes of atypical extra-esophageal reflux symptoms following laparoscopic antireflux surgery. Surg Endosc 25, 3852–3858 (2011). https://doi.org/10.1007/s00464-011-1806-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1806-y