Abstract
Objectives
Laboratory animal allergy is a highly prevalent occupational disease among exposed workers. The aim of the study was to validate the biomarkers of airway inflammation in laboratory animal (LA) care workers.
Methods
All of the participants in this observational study (63 LA care workers and 64 controls) were administered a clinical questionnaire, underwent spirometry and a skin prick or radioallergosorbent test for common and occupational aeroallergens, and the fraction of exhaled nitric oxide (FeNO50), exhaled breath condensate hydrogen peroxide (EBC H2O2) and serum pneumoprotein levels were measured. Multivariate analysis (ANCOVA) was used to assess the interactions of the variables.
Results
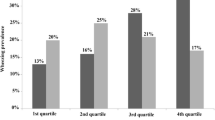
FeNO50 levels correlated with exposure (p = 0.002), sensitisation (p = 0.000) and age (p = 0.001), but there was no interaction between exposure and sensitisation when age was considered in the model (p = 0.146). EBC-H2O2 levels were higher in the sensitised workers than in the sensitised controls [0.14 (0.08–0.29) µM vs 0.07 (0.05–0.12) µM; p < 0.05]. Serum surfactant protein A (SP-A) levels were unaffected by exposure, sensitisation or age, although higher levels were observed in symptomatic workers; however, SP-D levels were influenced by exposure (p = 0.024) and age (p = 0.022), and club cell 16 levels were influenced by sensitisation (p = 0.027) and age (p = 0.019).
Conclusions
The presence of the clinical symptoms associated with LA exposure and high FeNO levels should prompt further medical assessments in LA workers. Although EBC-H2O2 levels do not seem to reflect eosinophilic inflammation, serum SP-A levels could be used to monitor progression from rhinitis to asthma.


Similar content being viewed by others
References
Adisesh LA, Kharitonov SA, Yates DH et al (1998) Exhaled and nasal nitric oxide is increased in laboratory animal allergy. Clin Exp Allergy 28(7):876–880
Alving K, Weitzberg E, Lundberg JM (1993) Increased amount of nitric oxide in exhaled air of asthmatics. Eur Respir J 6(9):1368–1370
American Thoracic Society, European Respiratory Society (2005) ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide, 2005. Am J Respir Crit Care Med 171:912–930
Antunes J, Borrego L, Romeira A et al (2009) Skin prick tests and allergy diagnosis. Allergol Immunopathol (Madr) 37(3):155–164
Aoyama K, Ueda A, Manda F et al (1992) Allergy to laboratory animals: an epidemiological study. Br J IndMed 49(1):41–47
Bauchau V, Durham SR (2004) Prevalence and rate of diagnosis of allergic rhinitis in Europe. Eur Respir J 24(5):758–764
Benson M, Fransson M, Martinsson T et al (2007) Inverse relation between nasal fluid Clara cell protein 16 levels and symptoms and signs of rhinitis in allergen-challenged patients with intermittent allergic rhinitis. Allergy 62(2):178–183
Broeckaert F, Arsalane K, Hermans C et al (2000) Serum clara cell protein: a sensitive biomarker of increased lung epithelium permeability caused by ambient ozone. Environ Health Perspect 108(6):533–537
Bush RK (2001a) Mechanism and epidemiology of laboratory animal allergy. ILAR J 42(1):4–11
Bush RK (2001b) Assessment and treatment of laboratory animal allergy. ILAR J 42(1):55–64
Carbonnelle S, Francaux M, Doyle I et al (2002) Changes in serum pneumoproteins caused by short-term exposures to nitrogen trichloride in indoor chlorinated swimming pools. Biomarkers 7(6):464–478
Chérot-Kornobis N, Hulo S, de Broucker V et al (2012) Induced sputum, exhaled NO, and breath condensate in occupational medicine. J Occup Environ Med 54(8):922–927
Chow S, Campbell C, Sandrini A, Thomas PS, Johnson AR, Yates DH (2009) Exhaled breath condensate biomarkers in asbestos-related lung disorders. Respir Med 103(8):1091–1097
Corradi M, Mutti A (2005) Exhaled breath analysis: from occupational to respiratory medicine. Acta Biomed 76(Suppl 2):20–29
Corradi M, Alinovi R, Goldoni M et al (2002) Biomarkers of oxidative stress after controlled human exposure to ozone. Toxicol Lett 134(1–3):219–225
Corradi M, Gergelova P, Mutti A (2010) Use of exhaled breath condensate to investigate occupational lung diseases. Curr Opin Allergy Clin Immunol 10(2):93–98
Corradi M, Romano C, Mutti A (2011) Laboratoryanimal; allergy; asthma. Med Lav 102(5):428–444
Corradi M, Gergelova P, Di Pilato E et al (2012) Effect of exposure to detergents and other chemicals on biomarkers of pulmonary response in exhaled breath from hospital cleaners: a pilot study. Int Arch Occup Environ Health 85(4):389–396
Corradi M, Goldoni M, Mutti A (2015) A review on airway biomarkers: exposure, effect and susceptibility. Expert Rev Respir Med 6:1–16
Crouch EC (1998) Collectins and pulmonary host defense. Am J Respir Cell Mol Biol 19:177–201
Cullinan P, Cook A, Nieuwenhuijsen MJ et al (2001) Allergen and dust exposure as determinants of work-related symptoms and sensitization in a cohort of flour-exposed workers; a case-control analysis. Ann Occup Hyg 45(2):97–103
Dweik RA, Boggs PB, Erzurum SC et al, American Thoracic Society Committee on Interpretation of Exhaled Nitric Oxide Levels (FENO) for Clinical Applications (2011) An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med 184(5):602–615
Erpenbeck VJ, Krug N, Hohlfeld JM (2009) Therapeutic use of surfactant components in allergic asthma. Naunyn Schmiedebergs Arch Pharmacol 379(3):217–224
Fireman E, Lerman Y, Stark M et al (2008) Detection of occult lung impairment in welders by induced sputum particles and breath oxidation. Am J Ind Med 51(7):503–511
Fisher AB, Dodia C, Ruckert P et al (2010) Pathway to lamellar bodies for surfactant protein A. Am J Physiol Lung Cell Mol Physiol 299(1):L51-8
Gautrin D, Infante-Rivard C, Ghezzo H,et al (2001) Incidence and host determinants of probable occupational asthma in apprentices exposed to laboratory animals. Am J Respir Crit Care Med 163:899–904
Greiner AN, Hellings PW, Rotiroti G et al (2011) Allergic rhinitis. Lancet 378(9809):2112–2122
Gube M, Ebel J, Brand P et al (2010) Biological effect markers in exhaled breath condensate and biomonitoring in welders: impact of smoking and protection equipment. Int Arch Occup Environ Health 83(7):803–811
Hermans C, Aly O, Nyberg BI et al (1998) Determinants of Clara cell protein (CC16) concentration in serum: a reassessment with two different immunoassays. Clin Chim Acta 272(2):101–110
Hermans C, Dong P, Robin M et al (2003) Determinants of serum levels of surfactant proteins A and B and Clara cell protein CC16. Biomarkers 8(6):461–471
Hollander A, Doekes G, Heederik D (1996) Cat and dog allergy and total IgE as risk factors of laboratory animal allergy. J Allergy Clin Immunol 98:545–554
Horváth I, Donnelly LE, Kiss A et al (1998) Combined use of exhaled hydrogen peroxide and nitric oxide in monitoring asthma. Am J Respir Crit Care Med 158(4):1042–1046
Horváth I, Hunt J, Barnes PJ et al (2005) ATS/ERS Task Force on Exhaled Breath Condensate. Exhaled breath condensate: methodological recommendations and unresolved questions. Eur Respir J 26(3):523–548
Johansson S, Keen C, Ståhl A et al (2005) Low levels of CC16 in nasal fluid of children with birch pollen-induced rhinitis. Allergy 60(5):638–642
Konradsen JR, Fujisawa T, van Hage M et al (2015) Allergy to furry animals: new insights, diagnostic approaches, and challenges. J Allergy Clin Immunol 135(3):616–625
Krakowiak A, Wiszniewska M, Krawczyk P et al (2007) Risk factors associated with airway allergic diseases from exposure to laboratory animal allergens among veterinarians. Int Arch Occup Environ Health 80(6):465–475
Kurowski M, Jurczyk J, Jarzębska M et al (2014) Association of serum Clara cell protein CC16 with respiratory infections and immune response to respiratory pathogens in elite athletes. Respir Res 15:45
Lakind JS, Holgate ST, Ownby DR et al (2007) A critical review of the use of Clara cell secretory protein (CC-16) as a biomarker of acute or chronic pulmonary effects. Biomarkers 12(5):445–467
LareseFilon F, Siracusa A, Rui F et al (2002) Prevalence of occupational allergy to laboratory animals in two towns of northern and central Italy. Med Lav 93(2):87–94
Laszlo G (2006) Standardisation of lung function testing: helpful guidance from the ATS/ERS Task Force. Thorax 61:744–746
Ledford JG, Pastva AM, Wright JR. Review (2010) Collectins link innate and adaptive immunity in allergic airway disease. Innate Immun 16(3):183–190
Ledford JG, Addison KJ, Foster MW et al (2014) Eosinophil-associated lung diseases. A cry for surfactant proteins A and D help? Am J Respir Cell Mol Biol 51(5):604–614
Liccardi G, Bilò MB, Manzi F et al (2015) What could be the role of molecular-based allergy diagnostics in detecting the risk of developing allergic sensitization to furry animals? Eur Ann Allergy Clin Immunol 47(5):163–167
Linhares D, Jacinto T, Pereira AM et al (2011) Effects of atopy and rhinitison exhaled nitric oxide values—a systematic review. Clin Transl Allergy 1(1):8
Madsen J, Tornoe I, Nielsen O et al (2003) Expression and localization of lung surfactant protein A in human tissues. Am J Respir Cell Mol Biol 29:591–597
Mutti A, Corradi M, Goldoni M et al (2006) Exhaled metallic elements and serum pneumoproteins in asymptomatic smokers and patients with COPD or asthma. Chest 129(5):1288–1297
National Institute for Occupational Safety and Health (NIOSH) (1998) NIOSH alert: preventing asthma in animal handlers. Publication no. 97-116
Olin AC, Alving K, Torén K (2004) Exhaled nitric oxide: relation to sensitization and respiratory symptoms. Clin Exp Allergy 34(2):221–226
Pacheco KA, McCammon C, Liu AH et al (2003) Airborne endotoxin predicts symptoms in non-mouse-sensitized technicians and research scientists exposed to laboratory mice. Am J Respir Crit Care Med 167(7):983–990
Palmberg L, Sundblad BM, Lindberg A et al (2015) Long term effect and allergic sensitization in newly employed workers in laboratory animal facilities. Respir Med 109(9):1164–1173
Pellegrino R, Viegi G, Brusasco V et al (2005) Interpretative strategies for lung function tests. Eur Respir J 26(5):948–968
Psathakis K, Mermigkis D, Papatheodorou G et al (2006) Exhaled markers of oxidative stress in idiopathic pulmonary fibrosis. Eur J Clin Investig 36(5):362–367
Qaseem AS, Sonar S, Mahajan L et al (2013) Linking surfactant protein SP-D and IL-13: implications in asthma and allergy. Mol Immunol 54(1):98–107
Quanjer PH, Stanojevic S, Cole TJ et al (2012) ERS Global Lung Function Initiative. Multi-ethnic reference values for spirometry for the 3–95-yr age range: theglobal lung function 2012 equations. Eur Respir J 40(6):1324–1343
Ricciardolo FL, Sterk PJ, Gaston B et al (2004) Nitric oxide in health and disease of the respiratory system. Physiol Rev 84(3):731–765
Ruoppi P, Koistinen T, Pennanen S (2005) Sensitisation to mites in laboratory animal workers with rhinitis. Occup Environ Med 62(9):612–615
Seward JP (1999) Occupational allergy to animals. Occup Med 14(2):285–304
Shijubo N, Kawabata I, Sato N et al (2003) Clinical aspects of Clara cell 10-kDa protein/uteroglobin (secretoglobin 1A1). Curr Pharm Des 9(14):1139–1149
Stolarek RA, Potargowicz E, Seklewska E et al (2010) Increased H2O2 level in exhaled breath condensate in primary breast cancer patients. J Cancer Res Clin Oncol 136(6):923–930
Suarthana E, Meijer E, Heederik D et al (2009) The Dutch diagnostic model for laboratory animal allergen sensitization was generalizable in Canadian apprentices. J Clin Epidemiol 62:542–549
Suresh V, Mih JD, George SC (2007) Measurement of IL-13-induced iNOS-derived gas phase nitric oxide in human bronchial epithelial cells. Am J Respir Cell Mol Biol 37(1):97–104
Tafuro F, Ridolo E, Goldoni M et al (2015) Work-related allergies to storage mites in Parma (Italy) ham workers. BMJ Open 5(5):e007502
Wolfle TL, Bush RK (2001) The science and pervasiveness of laboratory animal allergy. ILAR J 42(1):1–3
Wood RA (2001) Laboratory animal allergens. ILAR J 42(1):12–16
Ye Q, Fujita M, Ouchi H et al (2004) Serum CC-10 in inflammatory lung diseases. Respiration 71(5):505–510
Acknowledgements
The authors would like to thank Sonia Curioni, Marina Corti, Elisabetta Ferdenzi and Melissa Bonci for patient recruitment; Marcello Montagni and Valerie Melli for carrying out the skin prick tests; and Silvana Pinelli and Rossella Alinovi for their technical analyses.
Funding
This study received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Massimo Corradi: Scopus Author ID: 7005227313.
Rights and permissions
About this article
Cite this article
Tafuro, F., Selis, L., Goldoni, M. et al. Biomarkers of respiratory allergy in laboratory animal care workers: an observational study. Int Arch Occup Environ Health 91, 735–744 (2018). https://doi.org/10.1007/s00420-018-1321-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-018-1321-8