Abstract
Background
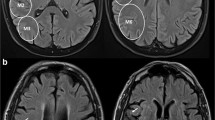
Distal medium vessel occlusions (DMVOs) contribute substantially to the incidence of acute ischemic strokes (AIS) and pose distinct challenges in clinical management and prognosis. Neuroimaging techniques, such as Fluid Attenuation Inversion Recovery (FLAIR) imaging and cerebral blood volume (CBV) index derived from perfusion imaging, have significantly improved our ability to assess the impact of strokes and predict their outcomes. The primary objective of this study was to investigate relationship between follow-up infarct volume (FIV) as assessed by FLAIR imaging in patients with DMVOs.
Methods
This prospectively collected, retrospective reviewed cohort study included patients from two comprehensive stroke centers within the Johns Hopkins Medical Enterprise, spanning August 2018–October 2022. The cohort consisted of adults with AIS attributable to DMVO. Detailed imaging analyses were conducted, encompassing non-contrast CT, CT angiography (CTA), CT perfusion (CTP), and FLAIR imaging. Univariable and multivariable linear regression models were employed to assess the association between different factors and FIV.
Results
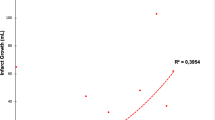
The study included 79 patients with DMVO stroke with a median age of 69 years (IQR, 62–77 years), and 57% (n = 45) were female. There was a negative correlation between the CBV index and FIV in a univariable linear regression analysis (Beta = – 16; 95% CI, – 23 to – 8.3; p < 0.001) and a multivariable linear regression model (Beta = – 9.1 per 0.1 change; 95% CI, – 15 to – 2.7; p = 0.006). Diabetes was independently associated with larger FIV (Beta = 46; 95% CI, 16 to 75; p = 0.003). Additionally, a higher baseline ASPECTS was associated with lower FIV (Beta = – 30; 95% CI, – 41 to – 20; p < 0.001).
Conclusion
Our findings underscore the CBV index as an independent association with FIV in DMVOs, which highlights the critical role of collateral circulation in determining stroke outcomes in this patient population. In addition, our study confirms a negative association of ASPECTS with FLAIR FIV and identifies diabetes as independent factor associated with larger FIV. These insights pave the way for further large-scale, prospective studies to corroborate these findings, thereby refining the strategies for stroke prognostication and management.


Similar content being viewed by others
References
Ospel JM, Goyal M (2021) A review of endovascular treatment for medium vessel occlusion stroke. J Neurointerv Surg 13(7):623–630. https://doi.org/10.1136/neurintsurg-2021-017321
Saver JL, Chapot R, Agid R et al (2020) Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke 51(9):2872–2884. https://doi.org/10.1161/STROKEAHA.120.028956
van Everdingen KJ, van der Grond J, Kappelle LJ, Ramos LM, Mali WP (1998) Diffusion-weighted magnetic resonance imaging in acute stroke. Stroke 29(9):1783–1790. https://doi.org/10.1161/01.str.29.9.1783
Van der Worp HP et al (2001) Reproducibility of measurements of cerebral infarct volume on CT scans. Stroke. https://doi.org/10.1161/01.str.32.2.424
Thijs VN, Lansberg MG, Beaulieu C, Marks MP, Moseley ME, Albers GW (2000) Is early ischemic lesion volume on diffusion-weighted imaging an independent predictor of stroke outcome? A multivariable analysis. Stroke 31(11):2597–2602. https://doi.org/10.1161/01.str.31.11.2597
Saunders DE, Clifton AG, Brown MM (1995) Measurement of infarct size using mri predicts prognosis in middle cerebral artery infarction. Stroke 26(12):2272–2276. https://doi.org/10.1161/01.STR.26.12.2272
Correlation of perfusion- and diffusion-weighted MRI with NIHSS score in acute (<6.5 hour) ischemic stroke - PubMed. Accessed 15 Jan 2024. https://pubmed.ncbi.nlm.nih.gov/9566364/
Farr TD, Wegener S (2010) Use of magnetic resonance imaging to predict outcome after stroke: a review of experimental and clinical evidence. J Cereb Blood Flow Metab 30(4):703–717. https://doi.org/10.1038/jcbfm.2010.5
Schiemanck SK, Kwakkel G, Post MWM, Prevo AJH (2006) Predictive value of ischemic lesion volume assessed with magnetic resonance imaging for neurological deficits and functional outcome poststroke: a critical review of the literature. Neurorehabil Neural Repair 20(4):492–502. https://doi.org/10.1177/1545968306289298
Ricci PE, Burdette JH, Elster AD, Reboussin DM (1999) A comparison of fast spin-echo, fluid-attenuated inversion-recovery, and diffusion-weighted MR imaging in the first 10 days after cerebral infarction. AJNR Am J Neuroradiol 20(8):1535–1542
Artzi M, Aizenstein O, Jonas-Kimchi T, Myers V, Hallevi H, Ben BD (2013) FLAIR lesion segmentation: application in patients with brain tumors and acute ischemic stroke. Eur J Radiol 82(9):1512–1518. https://doi.org/10.1016/j.ejrad.2013.05.029
Yedavalli V, Koneru M, Hamam O et al (2023) Pretreatment CTP collateral parameters predict good outcomes in successfully recanalized middle cerebral artery distal medium vessel occlusions. Clin Neuroradiol. https://doi.org/10.1007/s00062-023-01371-2
Arenillas JF, Cortijo E, García-Bermejo P et al (2018) Relative cerebral blood volume is associated with collateral status and infarct growth in stroke patients in SWIFT PRIME. J Cereb Blood Flow Metab 38(10):1839–1847. https://doi.org/10.1177/0271678X17740293
Imaoka Y, Shindo S, Miura M, Terasaki T, Mukasa A, Todaka T (2023) Hypoperfusion intensity ratio and CBV index as predictive parameters to identify underlying intracranial atherosclerotic stenosis in endovascular thrombectomy. J Neuroradiol 50(4):424–430. https://doi.org/10.1016/j.neurad.2022.10.005
Cheng-Ching E, Frontera JA, Man S et al (2015) Degree of collaterals and not time is the determining factor of core infarct volume within 6 hours of stroke onset. AJNR Am J Neuroradiol 36(7):1272–1276. https://doi.org/10.3174/ajnr.A4274
Hakimelahi R, Vachha BA, Copen WA et al (2014) Time and diffusion lesion size in major anterior circulation ischemic strokes. Stroke 45(10):2936–2941. https://doi.org/10.1161/STROKEAHA.114.005644
von Elm E, Altman DG, Egger M et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4(10):e296. https://doi.org/10.1371/journal.pmed.0040296
Cuschieri S (2019) The STROBE guidelines. Saudi J Anaesth 13(Suppl 1):S31–S34. https://doi.org/10.4103/sja.SJA_543_18
Koneru M, Hoseinyazdi M, Wang R et al (2023) Pretreatment parameters associated with hemorrhagic transformation among successfully recanalized medium vessel occlusions. J Neurol. https://doi.org/10.1007/s00415-023-12149-4
Souza LCS, Yoo AJ, Chaudhry ZA et al (2012) Malignant CTA collateral profile is highly specific for large admission DWI infarct core and poor outcome in acute stroke. AJNR Am J Neuroradiol 33(7):1331–1336. https://doi.org/10.3174/ajnr.A2985
Winkelmeier L et al (2023) Hypoperfusion intensity ratio is correlated with the risk of parenchymal hematoma after endovascular stroke treatment. Stroke. https://doi.org/10.1161/STROKEAHA.122.040540
Jiang Y, Han J, Spencer P et al (2021) Diabetes mellitus: a common comorbidity increasing hemorrhagic transformation after tPA thrombolytic therapy for ischemic stroke. Brain Hemorrhages 2(3):116–123. https://doi.org/10.1016/j.hest.2020.11.004
Broderick JP et al (1995) Hyperglycemia and hemorrhagic transformation of cerebral infarcts. Stroke. https://doi.org/10.1161/01.STR.26.3.484
Lau LH et al (2019) Prevalence of diabetes and its effects on stroke outcomes: a meta-analysis and literature review. J Diabetes Investig. https://doi.org/10.1111/jdi.12932
Hafez S et al (2016) Matrix metalloprotease 3 exacerbates hemorrhagic transformation and worsens functional outcomes in hyperglycemic stroke. Stroke. https://doi.org/10.1161/STROKEAHA.115.011258
Gliem M et al (2015) Hyperglycemia and PPARγ antagonistically influence macrophage polarization and infarct healing after ischemic stroke. Stroke. https://doi.org/10.1161/STROKEAHA.115.010557
Blood brain barrier disruption in diabetic stroke related to unfavorable outcome - PubMed. Accessed 15 Feb 2024. https://pubmed.ncbi.nlm.nih.gov/26986824/
Hoffmann A et al (2018) Early blood–brain barrier disruption in ischemic stroke initiates multifocally around capillaries/venules. Stroke. https://doi.org/10.1161/STROKEAHA.118.020927
Tasker RC, Acerini CL (2014) Cerebral edema in children with diabetic ketoacidosis: vasogenic rather than cellular? Pediatr Diabetes 15(4):261–270. https://doi.org/10.1111/pedi.12153
Venditti L, Chassin O, Ancelet C et al (2021) Pre-procedural predictive factors of symptomatic intracranial hemorrhage after thrombectomy in stroke. J Neurol 268(5):1867–1875. https://doi.org/10.1007/s00415-020-10364-x
Demeestere J, Garcia-Esperon C, Garcia-Bermejo P et al (2017) Evaluation of hyperacute infarct volume using ASPECTS and brain CT perfusion core volume. Neurology 88(24):2248–2253. https://doi.org/10.1212/WNL.0000000000004028
Olive-Gadea M, Martins N, Boned S et al (2019) Baseline ASPECTS and e-ASPECTS Correlation with infarct volume and functional outcome in patients undergoing mechanical thrombectomy. J Neuroimaging 29(2):198–202. https://doi.org/10.1111/jon.12564
Muir KW, Buchan A, von Kummer R, Rother J, Baron JC (2006) Imaging of acute stroke. Lancet Neurol 5(9):755–768. https://doi.org/10.1016/S1474-4422(06)70545-2
Broocks G, McDonough R, Meyer L et al (2021) Reversible ischemic lesion hypodensity in acute stroke CT following endovascular reperfusion. Neurology 97(11):e1075–e1084. https://doi.org/10.1212/WNL.0000000000012484
Jiang Q, Wang H, Ge J et al (2022) Mechanical thrombectomy versus medical care alone in large ischemic core: an up-to-date meta-analysis. Interv Neuroradiol 28(1):104–114. https://doi.org/10.1177/15910199211016258
Powers WJ, Rabinstein AA, Ackerson T et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke 50(12):e344–e418. https://doi.org/10.1161/STR.0000000000000211
Turc G, Bhogal P, Fischer U et al (2023) European stroke organisation (ESO) - European society for minimally invasive neurological therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg 15(8):e8. https://doi.org/10.1136/neurintsurg-2018-014569
Saber H, Narayanan S, Palla M et al (2018) Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: a meta-analysis. J Neurointerv Surg 10(7):620–624. https://doi.org/10.1136/neurintsurg-2017-013515
Nogueira RG, Zaidat OO, Castonguay AC et al (2016) Rescue thrombectomy in large vessel occlusion strokes leads to better outcomes than intravenous thrombolysis alone: a “Real World” applicability of the recent trials. Interv Neurol 5(3–4):101–110. https://doi.org/10.1159/000445809
Sarraj A, Hassan A, Savitz SI et al (2018) Endovascular thrombectomy for mild strokes: how low should we go? Stroke 49(10):2398–2405. https://doi.org/10.1161/STROKEAHA.118.022114
Strambo D, Bartolini B, Beaud V et al (2020) Thrombectomy and thrombolysis of isolated posterior cerebral artery occlusion: cognitive, visual, and disability outcomes. Stroke 51(1):254–261. https://doi.org/10.1161/STROKEAHA.119.026907
Tourdias T, Renou P, Sibon I et al (2011) Final cerebral infarct volume is predictable by MR imaging at 1 week. Am J Neuroradiol 32(2):352–358. https://doi.org/10.3174/ajnr.A2271
Thomalla G, Gerloff C (2010) We are on the clock: MRI as a surrogate marker of lesion age in acute ischemic stroke. Stroke 41(2):197–198. https://doi.org/10.1161/STROKEAHA.109.570085
FLAIR Vascular Hyperintensities as a Surrogate of Collaterals in Acute Stroke: DWI Matters - PubMed. Accessed 14 Feb 2024. https://pubmed.ncbi.nlm.nih.gov/36521962/
Wu O, Schwamm LH, Sorensen AG (2011) Imaging stroke patients with unclear onset times. Neuroimaging Clin N Am 21(2):327–344. https://doi.org/10.1016/j.nic.2011.02.008
Zhang X, Huang P, Zhang R (2022) Evaluation and prediction of post-stroke cerebral edema based on neuroimaging. Front Neurol 12:763018. https://doi.org/10.3389/fneur.2021.763018
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Salim, H., Lakhani, D.A., Balar, A. et al. Follow-up infarct volume on fluid attenuated inversion recovery (FLAIR) imaging in distal medium vessel occlusions: the role of cerebral blood volume index. J Neurol (2024). https://doi.org/10.1007/s00415-024-12279-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00415-024-12279-3