Abstract
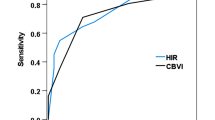
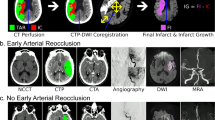
Although pretreatment radiographic biomarkers are well established for hemorrhagic transformation (HT) following successful mechanical thrombectomy (MT) in large vessel occlusion (LVO) strokes, they are yet to be explored for medium vessel occlusion (MeVO) acute ischemic strokes. We aim to investigate pretreatment imaging biomarkers representative of collateral status, namely the hypoperfusion intensity ratio (HIR) and cerebral blood volume (CBV) index, and their association with HT in successfully recanalized MeVOs. A prospectively collected registry of acute ischemic stroke patients with MeVOs successfully recanalized with MT between 2019 and 2023 was retrospectively reviewed. A multivariate logistic regression for HT of any subtype was derived by combining significant univariate predictors into a forward stepwise regression with minimization of Akaike information criterion. Of 60 MeVO patients successfully recanalized with MT, HT occurred in 28.3% of patients. Independent factors for HT included: diabetes mellitus history (p = 0.0005), CBV index (p = 0.0071), and proximal versus distal occlusion location (p = 0.0062). A multivariate model with these factors had strong diagnostic performance for predicting HT (area under curve [AUC] 0.93, p < 0.001). Lower CBV indexes, distal occlusion location, and diabetes history are significantly associated with HT in MeVOs successfully recanalized with MT. Of note, HIR was not found to be significantly associated with HT.


Similar content being viewed by others
Data availability
De-identified data will be made available upon reasonable request to the corresponding author.
References
Saver JL, Chapot R, Agid R et al (2020) Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke 51:2872–2884. https://doi.org/10.1161/STROKEAHA.120.028956
Menon BK, Hill MD, Davalos A et al (2019) Efficacy of endovascular thrombectomy in patients with M2 segment middle cerebral artery occlusions: meta-analysis of data from the HERMES Collaboration. J Neurointerv Surg 11:1065–1069. https://doi.org/10.1136/neurintsurg-2018-014678
Sepp D, Hernandez Petzsche MR, Zarth T et al (2023) Mechanical thrombectomy of distal cerebral vessel occlusions of the anterior circulation. Sci Rep 13:5730. https://doi.org/10.1038/s41598-023-32634-0
Cartmell SCD, Ball RL, Kaimal R et al (2018) Early cerebral vein after endovascular ischemic stroke treatment predicts symptomatic reperfusion hemorrhage. Stroke 49:1741–1746. https://doi.org/10.1161/STROKEAHA.118.021402
Heit JJ, Mlynash M, Christensen S et al (2021) What predicts poor outcome after successful thrombectomy in late time windows? J Neurointerv Surg 13:421–425. https://doi.org/10.1136/neurintsurg-2020-016125
Seners P, Wouters A, Maïer B et al (2023) Role of brain imaging in the prediction of intracerebral hemorrhage following endovascular therapy for acute stroke. Stroke. https://doi.org/10.1161/STROKEAHA.123.040806
Guenego A, Marcellus DG, Martin BW et al (2019) Hypoperfusion intensity ratio is correlated with patient eligibility for thrombectomy. Stroke 50:917–922. https://doi.org/10.1161/STROKEAHA.118.024134
Winkelmeier L, Heit JJ, Adusumilli G et al (2023) Hypoperfusion intensity ratio is correlated with the risk of parenchymal hematoma after endovascular stroke treatment. Stroke 54:135–143. https://doi.org/10.1161/STROKEAHA.122.040540
Arenillas JF, Cortijo E, García-Bermejo P et al (2018) Relative cerebral blood volume is associated with collateral status and infarct growth in stroke patients in SWIFT PRIME. J Cereb Blood Flow Metab 38:1839–1847. https://doi.org/10.1177/0271678X17740293
Cortijo E, Calleja AI, García-Bermejo P et al (2014) Relative cerebral blood volume as a marker of durable tissue-at-risk viability in hyperacute ischemic stroke. Stroke 45:113–118. https://doi.org/10.1161/STROKEAHA.113.003340
Simera I, Moher D, Hoey J et al (2010) A catalogue of reporting guidelines for health research. Eur J Clin Investig 40:35–53. https://doi.org/10.1111/j.1365-2362.2009.02234.x
Adams HP Jr, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41. https://doi.org/10.1161/01.str.24.1.35
Yedavalli V, Kihira S, Shahrouki P et al (2023) CTP-based estimated ischemic core: a comparative multicenter study between Olea and RAPID software. J Stroke Cerebrovasc Dis 32:107297. https://doi.org/10.1016/j.jstrokecerebrovasdis.2023.107297
Yedavalli V, Hamam O, Mohseni A et al (2023) Pretreatment brain CT perfusion thresholds for predicting final infarct volume in distal medium vessel occlusions. J Neuroimaging. https://doi.org/10.1111/jon.13142
Yedavalli V, Koneru M, Hoseinyazdi M et al (2023) Excellent recanalization and small core volumes are associated with favorable AM-PAC score in patients with acute ischemic stroke secondary to large vessel occlusion. Arch Rehabil Res Clin Transl. https://doi.org/10.1016/j.arrct.2023.100306
Demeestere J, Wouters A, Christensen S et al (2020) Review of perfusion imaging in acute ischemic stroke: from time to tissue. Stroke 51:1017–1024. https://doi.org/10.1161/STROKEAHA.119.028337
Nael K, Tadayon E, Wheelwright D et al (2019) Defining ischemic core in acute ischemic stroke using CT perfusion: a multiparametric Bayesian-based model. AJNR Am J Neuroradiol 40:1491–1497. https://doi.org/10.3174/ajnr.A6170
Yoshie T, Yu Y, Jiang H et al (2020) Perfusion parameter thresholds that discriminate ischemic core vary with time from onset in acute ischemic stroke. AJNR Am J Neuroradiol 41:1809–1815. https://doi.org/10.3174/ajnr.A6744
Potreck A, Scheidecker E, Weyland CS et al (2022) RAPID CT perfusion-based relative CBF identifies good collateral status better than hypoperfusion intensity ratio, CBV-index, and time-to-maximum in anterior circulation stroke. AJNR Am J Neuroradiol 43:960–965. https://doi.org/10.3174/ajnr.A7542
Rao V, Christensen S, Yennu A et al (2019) Ischemic core and hypoperfusion volumes correlate with infarct size 24 hours after randomization in DEFUSE 3. Stroke 50:626–631. https://doi.org/10.1161/STROKEAHA.118.023177
Rao VL, Mlynash M, Christensen S et al (2020) Collateral status contributes to differences between observed and predicted 24-h infarct volumes in DEFUSE 3. J Cereb Blood Flow Metab 40:1966–1974. https://doi.org/10.1177/0271678X20918816
Chen C, Parsons MW, Levi CR et al (2021) What is the “optimal” target mismatch criteria for acute ischemic stroke? Front Neurol. https://doi.org/10.3389/fneur.2020.590766
Larrue V, von Kummer RR, Müller A, Bluhmki E (2001) Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke 32:438–441. https://doi.org/10.1161/01.str.32.2.438
Boisseau W, Fahed R, Lapergue B et al (2019) Predictors of parenchymal hematoma after mechanical thrombectomy: a multicenter study. Stroke 50:2364–2370. https://doi.org/10.1161/STROKEAHA.118.024512
Guenego A, Farouki Y, Mine B et al (2022) Hypoperfusion intensity ratio predicts infarct growth after successful thrombectomy for distal medium vessel occlusion. Clin Neuroradiol 32:849–856. https://doi.org/10.1007/s00062-022-01141-6
Jiang Y, Han J, Spencer P et al (2021) Diabetes mellitus: a common comorbidity increasing hemorrhagic transformation after tPA thrombolytic therapy for ischemic stroke. Brain Hemorrhages 2:116–123. https://doi.org/10.1016/j.hest.2020.11.004
Broderick JP, Hagen T, Brott T, Tomsick T (1995) Hyperglycemia and hemorrhagic transformation of cerebral infarcts. Stroke 26:484–487. https://doi.org/10.1161/01.str.26.3.484
Lau L-H, Lew J, Borschmann K et al (2019) Prevalence of diabetes and its effects on stroke outcomes: a meta-analysis and literature review. J Diabetes Investig 10:780–792. https://doi.org/10.1111/jdi.12932
Hafez S, Abdelsaid M, El-Shafey S et al (2016) Matrix metalloprotease 3 exacerbates hemorrhagic transformation and worsens functional outcomes in hyperglycemic stroke. Stroke 47:843–851. https://doi.org/10.1161/STROKEAHA.115.011258
Gliem M, Klotz L, van Rooijen N et al (2015) Hyperglycemia and PPARγ antagonistically influence macrophage polarization and infarct healing after ischemic stroke. Stroke 46:2935–2942. https://doi.org/10.1161/STROKEAHA.115.010557
Chalouhi N, Tjoumakaris S, Starke RM et al (2014) Endovascular stroke intervention in young patients with large vessel occlusions. Neurosurg Focus 36:E6. https://doi.org/10.3171/2013.9.FOCUS13398
Marsh EB, Llinas RH, Schneider ALC et al (2016) Predicting hemorrhagic transformation of acute ischemic stroke: prospective validation of the HeRS score. Medicine 95:e2430. https://doi.org/10.1097/MD.0000000000002430
Marsh EB, Llinas RH, Hillis AE, Gottesman RF (2013) Hemorrhagic transformation in patients with acute ischaemic stroke and an indication for anticoagulation. Eur J Neurol 20:962–967. https://doi.org/10.1111/ene.12126
Sun J, Lam C, Christie L et al (2023) Risk factors of hemorrhagic transformation in acute ischaemic stroke: a systematic review and meta-analysis. Front Neurol 14:1079205. https://doi.org/10.3389/fneur.2023.1079205
Bala F, Singh N, Menon BK et al (2022) Poor cortical venous opacification on baseline computed tomography angiography predicts parenchymal hemorrhage after thrombectomy. Stroke Vasc Interv Neurol 2:e000299. https://doi.org/10.1161/SVIN.121.000299
Nogueira RG, Gupta R, Jovin TG et al (2015) Predictors and clinical relevance of hemorrhagic transformation after endovascular therapy for anterior circulation large vessel occlusion strokes: a multicenter retrospective analysis of 1122 patients. J Neurointerv Surg 7:16–21
Faizy TD, Kabiri R, Christensen S et al (2021) Distinct intra-arterial clot localization affects tissue-level collaterals and venous outflow profiles. Eur J Neurol 28:4109–4116. https://doi.org/10.1111/ene.15079
Funding
This study is supported by the Johns Hopkins University School of Medicine Department of Radiology Physician Scientist Incubator Program (RAD-PSI) in addition to the following grants: R01 N106711 and P41 EB031771.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by VY. The analysis was performed by MK. The first draft of the manuscript was written by MK and VY, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Drs. Vivek Yedavalli, Jeremy Heit, and Gregory Albers are consultants for iSchemaView (Menlo Park, CA, USA), not related to submitted work.
Ethical approval
This study was approved by the institutional review board of the Johns Hopkins School of Medicine.
Informed consent
This retrospective study was approved by the IRB with waiver of informed consent.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koneru, M., Hoseinyazdi, M., Wang, R. et al. Pretreatment parameters associated with hemorrhagic transformation among successfully recanalized medium vessel occlusions. J Neurol 271, 1901–1909 (2024). https://doi.org/10.1007/s00415-023-12149-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-12149-4