Abstract
Background/Purpose
Distal medium vessel occlusions (DMVOs) account for a large percentage of vessel occlusions resulting in acute ischemic stroke (AIS) with disabling symptoms. We aim to assess whether pretreatment quantitative CTP collateral status (CS) parameters can serve as imaging biomarkers for good clinical outcomes prediction in successfully recanalized middle cerebral artery (MCA) DMVOs.
Methods
We performed a retrospective analysis of consecutive patients with AIS secondary to primary MCA-DMVOs who were successfully recanalized by mechanical thrombectomy (MT) defined as modified thrombolysis in cerebral infarction (mTICI) 2b, 2c, or 3. We evaluated the association between the CBV index and HIR independently with good clinical outcomes (modified Rankin score 0–2) using Spearman rank correlation, logistic regression, and ROC analyses.
Results
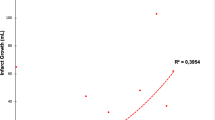
From 22 August 2018 to 18 October 2022 8/22/2018 to 10/18/2022, 60 consecutive patients met our inclusion criteria (mean age 71.2 ± 13.9 years old [mean ± SD], 35 female). The CBV index (r = −0.693, p < 0.001) and HIR (0.687, p < 0.001) strongly correlated with 90-day mRS.
A CBV index ≥ 0.7 (odds ratio, OR, 2.27, range 6.94–21.23 [OR] 2.27 [6.94–21.23], p = 0.001)) and lower likelihood of prior stroke (0.13 [0.33–0.86]), p = 0.024)) were independently associated with good outcomes.
The ROC analysis demonstrated good performance of the CBV index in predicting good 90-day mRS (AUC 0.73, p = 0.003) with a threshold of 0.7 for optimal sensitivity (71% [52.0–85.8%]) and specificity (76% [54.9–90.6%]). The HIR also demonstrated adequate performance in predicting good 90-day mRS (AUC 0.77, p = 0.001) with a threshold of 0.3 for optimal sensitivity (64.5% [45.4–80.8%]) and specificity (76.0% [54.9–90.6%]).
Conclusion
A CBV index ≥ 0.7 may be independently associated with good clinical outcomes in our cohort of AIS caused by MCA-DMVOs that were successfully treated with MT. Furthermore, a HIR < 0.3 is also associated with good clinical outcomes. This is the first study of which we are aware to identify a CBV index threshold for MCA-DMVOs.

Similar content being viewed by others
References
Saver JL, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke. 2020;51:2872–84.
Guenego A, et al. Thrombectomy for distal medium vessel occlusion with a new generation of Stentretriever (Tigertriever 13). Interv Neuroradiol. 2021;15910199211039926.
Kauw F, et al. Collateral status in Ischemic stroke: a comparison of computed tomography angiography, computed tomography perfusion, and digital subtraction Angiography. J Comput Assist Tomogr. 2020;44:984–92.
Wolff L, et al. Inter-rater reliability for assessing intracranial collaterals in patients with acute ischemic stroke: comparing 29 raters and an artificial intelligence-based software. Neuroradiology. 2022;64:2277–84.
Arenillas JF, et al. Relative cerebral blood volume is associated with collateral status and infarct growth in stroke patients in SWIFT PRIME. J Cereb Blood Flow Metab. 2018;38:1839–47.
Guenego A, et al. Hypoperfusion intensity ratio correlates with angiographic collaterals in acute ischaemic stroke with M1 occlusion. Eur J Neurol. 2020;27:864–70.
Olivot JM, et al. Hypoperfusion intensity ratio predicts infarct progression and functional outcome in the DEFUSE 2 Cohort. Stroke. 2014;45:1018–23.
Guenego A, et al. Hypoperfusion intensity ratio is correlated with patient eligibility for thrombectomy. Stroke. 2019;50:917–22.
Rao VL, et al. Collateral status contributes to differences between observed and predicted 24‑h infarct volumes in DEFUSE 3. J Cereb Blood Flow Metab. 2020;40:1966–74.
Guenego A, et al. Hypoperfusion intensity ratio predicts infarct growth after successful thrombectomy for distal medium vessel occlusion. Clin Neuroradiol. 2022;32:849–56.
Simera I, Moher D, Hoey J, Schulz KF, Altman DG. A catalogue of reporting guidelines for health research. Eur J Clin Invest. 2010;40:35–53.
Menon BK, et al. Efficacy of endovascular thrombectomy in patients with M2 segment middle cerebral artery occlusions: meta-analysis of data from the HERMES Collaboration. J Neurointerv Surg. 2019;11:1065–9.
Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second european-australasian acute stroke study investigators. Lancet. 1998;352:1245–1251.
Liu L, et al. Guidelines for evaluation and management of cerebral collateral circulation in ischaemic stroke 2017. Stroke Vasc Neurol. 2018;3:117–30.
Saber H, et al. Endovascular therapy vs medical management for patients with acute stroke with medium vessel occlusion in the anterior circulation. JAMA Netw Open. 2022;5:e2238154.
Farouki Y, et al. First-pass effect predicts clinical outcome and infarct growth after thrombectomy for distal medium vessel occlusions. Neurosurgery. 2022;91:913–9.
MacLellan A, et al. Perfusion imaging collateral scores predict infarct growth in non-Reperfused DEFUSE 3 patients. J Stroke Cerebrovasc Dis. 2022;31:106208.
Lu W‑Z, Lin H‑A, Hou S‑K, Bai C‑H, Lin S‑F. Diagnostic test accuracy of pretreatment collateral score in predicting stroke outcomes after intra-arterial endovascular thrombectomy: a meta-analysis in DSA and CTA. Eur Radiol. 2022;32:6097–107.
van den Wijngaard IR, et al. Impact of collateral status evaluated by dynamic computed tomographic angiography on clinical outcome in patients with Ischemic stroke. Stroke. 2015;46:3398–404.
Lyndon D, et al. Hypoperfusion intensity ratio correlates with CTA collateral status in large-vessel occlusion acute ischemic stroke. AJNR Am J Neuroradiol. 2021;42:1380–6.
Winkelmeier L, et al. Hypoperfusion intensity ratio is correlated with the risk of parenchymal hematoma after endovascular stroke treatment. Stroke. 2023;54:135–43.
Ospel JM, et al. Prevalence and outcomes of medium vessel occlusions with discrepant infarct patterns. Stroke. 2020;51:2817–24.
Flach C, Muruet W, Wolfe CDA, Bhalla A, Douiri A. Risk and secondary prevention of stroke recurrence: a population-base cohort study. Stroke. 2020;51:2435–44.
Burn J, et al. Long-term risk of recurrent stroke after a first-ever stroke. The Oxfordshire community stroke project. Stroke. 1994;25:333–7.
Kolmos M, Christoffersen L, Kruuse C. Recurrent Ischemic stroke—A systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2021;30:105935.
Kargiotis O, et al. Computed tomography perfusion imaging in acute ischemic stroke: accurate interpretation matters. Stroke. 2023;54:e104–8.
Faizy TD, et al. Distinct intra-arterial clot localization affects tissue-level collaterals and venous outflow profiles. Eur J Neurol. 2021;28:4109–16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
V. Yedavalli, M. Koneru, O. Hamam, M. Hoseinyazdi, E.B. Marsh, R. Llinas, V. Urrutia, R. Leigh, F. Gonzalez, R. Xu, J. Caplan, J. Huang, H. Lu, M. Wintermark, J. Heit, A. Guenego, G. Albers, K. Nael and A. Hillis declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yedavalli, V., Koneru, M., Hamam, O. et al. Pretreatment CTP Collateral Parameters Predict Good Outcomes in Successfully Recanalized Middle Cerebral Artery Distal Medium Vessel Occlusions. Clin Neuroradiol 34, 341–349 (2024). https://doi.org/10.1007/s00062-023-01371-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-023-01371-2