Abstract
Objective
This study aimed to correlate the symptoms and signs with the findings of laboratory vestibular function tests in patients with spinocerebellar ataxia (SCA).
Method
We retrospectively recruited 26 patients with SCA (9 men, median age: 52, age range: 21–67). Assessments included Dizziness Handicap Inventory, EuroQoL Five-Dimension, symptom questionnaires manifesting during walking in daily life, the Scale for the Assessment and Rating of Ataxia (SARA), and vestibular function tests including 3D video-oculography, video head impulse test, subjective visual vertical, and cervical and ocular vestibular evoked myogenic potentials (VEMP).
Results
Cross-analyses revealed that the patients with VEMP abnormalities showed higher SARA (p = 0.014) and prevalence of unpredictable falls (p = 0.046). The patients with SCA1 more frequently had unpredictable falls (75%, p = 0.038) and VEMP abnormalities (88%, p = 0.001) compared to SCA2 (29% falls, 17% VEMP abnormalities) and SCA6 (no falls or VEMP abnormalities).
Conclusion
Abnormal VEMPs are strongly associated with unpredicted falls in patients with SCA, particularly in those with SCA1. Impaired processing of otolithic information may contribute to falls in SCAs, and VEMP may help identifying the patients with a risk for unpredicted falls and preventing fall-related injuries in SCA. Limited number of patients with lower SARA scores warrant further confirmatory studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The autosomal dominant spinocerebellar ataxias (SCA) are neurogenerative disorders characterized by progressive cerebellar ataxia due to Purkinje cell degeneration. [1] The most common forms, SCA type 1, 2, 3, and 6, are caused by expansions of CAG repeats encoding the polyglutamine tracts within the several unrelated genes, ataxin1, ataxin2, ataxin3, and the gene encoding the alpha1 A subunit of voltage-gated calcium channel. [1,2,3] Even though SCAs are genetically and clinically heterogenous, cerebellar and brainstem ocular motor signs are common to SCAs. [4, 5] Evaluation of eye movements such as nystagmus, saccades, smooth pursuits, and the vestibulo-ocular reflex (VOR), each characterized by unique neural pathways, [6] may aid in specification of each SCA subtype. [7] Furthermore, since eye movements can be recorded and quantified, abnormal eye movements may serve as a marker for disease progression and therapeutic efficacy and guide genetic testing. [7]
Previous studies have mostly concentrated on associations among the CAG repeat numbers, ataxia scores, and neuroimaging abnormalities in SCA. [2, 8] However, the ataxia score alone cannot fully represent the quality of life (QoL), especially unpredicted falls that significantly affect the QoL. [9,10,11,12]
Despite the efforts to find out medication targeting the pathophysiological mechanisms of SCAs, a definitive cure remains elusive in these disorders. [13, 14] In this context, researches focusing on improving the QoL throughout a patient's life are essential. [15] Thus, it would be valuable to identify objective neurological signs that correlate with the subjective symptoms or QoL, potentially serving as the clinical markers for guidance of therapeutic intervention. The objective of this study is to illuminate any correlation between the objective findings of ocular motor and vestibular function tests and the symptoms and QoL in patients with SCAs.
Methods
Patients
Two authors retrospectively reviewed the medical records of 37 patients with genetically confirmed autosomal dominant SCA at the dizziness clinic of Pusan National University Hospital from January 2019 to March 2022. We finally recruited 26 (9 men, median age: 52, age range: 21–67) for analyses after excluding 11 patients with incomplete evaluation due to a bed-ridden state (n = 4), a follow-up loss (n = 4), refusal of the testing (n = 2), and a previous history of vestibular neuritis (n = 1). The subtypes of SCA included SCA1 in eight from four families, SCA2 in 14 from eight families, and SCA6 in four from three families. There were no differences in age, sex, and disease duration among the subtypes (Table 2).
Standard protocol approvals, registration, and patient contents
This study followed the tenets of the Declaration of Helsinki and was performed according to the guidelines of the Institutional Review Board of Pusan National University Hospital (2108–001-105).
Evaluation of ataxia and scoring for symptoms and quality of life
The assessments for cerebellar ataxia were based on the Scale for the Rating and Assessment of Ataxia (SARA) that was scored by the sum of the gait, stance, sitting, speech disturbance, finger-chase, nose-finger test, fast alternating hand and heel-shin movements. [5] Self-administered questionnaires for evaluation of dizziness and health-related QoL included the dizziness handicap inventory (DHI) [16, 17] and the five-level EuroQoL five-Dimension (EQ-5D-5L). [18] To assess the symptoms during walking in daily life, the following yes or no questions were also added; "Q1: Have you had unpredictable falls?" "Q2: Do you feel more dizzy in moving conditions, such as in a moving elevator or escalator?" "Q3: Do you feel a pulling sensation to one side while walking (lateropulsion)?".
Oculography and video head impulse tests
Eye movements were recorded at a sampling rate of 60 Hz using 3D-video-oculography (VOG, SLMED, Seoul, Korea). Spontaneous nystagmus (SN) with or without visual fixation, gaze-evoked nystagmus (GEN), and horizontal saccades and smooth pursuit were pursued following the methods described previously in detail. [19] Head and eye movements were also recorded during head impulses using a video-based equipment (vHIT, SLMED, Seoul, South Korea). The detailed methods and normative data on gain of the vestibulo-ocular reflex (VOR) for six semicircular canals (SCCs) were described previously. [20]
Cervical and ocular vestibular evoked myogenic potentials, and subjective visual vertical
The detailed methods for recording cervical and ocular vestibular evoked myogenic potentials (VEMPs) and the subjective visual vertical (SVV) were described previously. [20, 21] VEMPs were recorded using a Nicolet Viking Select unit (Nicolet Biomedical, Madison, WI, USA) on the same day. Cervical VEMP (cVEMP) was recorded from the ipsilateral sternocleidomastoid muscle (SCM) that was activated by elevating and turning the head contralaterally in the supine position. Electromyographic activities of the SCM were simultaneously recorded using a surface electrode from the upper half of the SCM with a ground electrode on the forehead and a reference electrode over the upper sternum. A short alternating tone burst (110 dB nHL; 121.5 dB SPL; 500 Hz; ramp = 2 ms; plateau = 3 ms) was given at 2.1 Hz monoaurally using a headphone. During the recording, the EMG activities of the SCM were also monitored and digitized at 1 kHz using an analog-to-digital converter (NI PCI-4461, National Instruments, Austin, TX, USA). The LabVIEW program (National Instruments) was used to analyse the peak-to-peak amplitudes and calculate the mean tonic activation during the recording. The absolute cVEMP amplitude was then normalized against the mean tonic activation of the SCM during the recording. [21] We confirmed that none of the patients had the conditions leading to conductive hearing loss, such as middle ear infections, and no patients reported subjective hearing impairments. To record ocular VEMP (oVEMP), patients sat with their head upright while fixating on a target that was displaced on the wall, more than 2 m away from the eyes, with an angle of gaze more than 20° upward. Electromyographic activities were recorded using a surface electrode placed on the infra-orbital ridge 1 cm below the center of the lower eyelid. The reference electrode was attached 2 cm below the active electrode, and the ground electrode on the forehead. Bilateral oVEMPs were induced tapping the hairline at AFz up to 60 times using an electric reflex hammer (VIASYS Healthcare, CA, USA). The latency of cVEMP was measured as the time when the positive wave (p13) at around 13 ms and the negative wave (n23) at around 23 ms appeared, and the amplitude between these two waves was normalized to the SCM contraction. For oVEMP, the latency of the negative wave at around 10 ms (n10) and the amplitude between n10 and the subsequent positive wave were measured. We compared the VEMPs of the patient group with those of 26 age-matched control (Median age = 53, IQR 40–58, p = 0.096). Abnormal VEMPs were defined as no responses to stimulation or asymmetry of the amplitudes > 20%. [20, 21]
The SVV tilt was measured while seating the patient in a darkroom. The patients were instructed to align a randomly tilted rod (80 cm long and 0.3 cm wide) vertically using a joystick at least five times per each session. The normal value of SVV is ± 3° during binocular viewing (a negative value indicates a counterclockwise rotation). [20, 21]
Statistical analysis
Statistical analyses were performed using SPSS (version 23.0; SPSS, Chicago, IL). Quantitative values are presented as the median (IQR, first—third quartile) or mean ± standard deviation (SD), and the qualitative values as the frequency (%, percent). The Kruskal–Wallis or Mann–Whitney test was used for the continuous variables and Chi-square or Fisher’s exact tests for the nominal ones. When comparing the continuous variables among the groups, we employed either the student t or Mann–Whitney test. The significance level was set at p < 0.05.
Results
Thirteen (50%) Patients reported moderate dizziness with the median DHI score at 32 (IQR, 11–63) and the median EQ-5D-5L score at 10 (IQL, 8–14) (Table 1). Almost all the patients (25/26, 96%) showed gait abnormalities with the score more than 2 on the gait subdomain of SARA, which indicates that the patients could not complete more than 10 tandem steps. The SARA, DHI, and QoL did not differ among the subtypes of SCA.
About one third of patients (10/26, 38%) also reported unpredicted falls or gait unsteadiness. Of interest, patients with SCA1 showed a higher prevalence of unpredicted falls (6/8, 75%, p = 0.038, Table 2). In contrast, only two patients (8%) reported dizziness in a moving elevator or escalator (Table 1).
Ocular motor and vestibular function tests
Detailed description of the ocular motor findings is provided in Table 1. No patients exhibited SN with or without fixation. However, all patients showed cerebellar ocular motor dysfunction that included GEN, impaired smooth pursuit, or hypermetric saccades. GEN was observed in all patients with SCA6 (p = 0.040). Slowing of horizontal saccades was observed in 15 (58%) patients and was more prevalent in patients with SCA2 (13/14, 93%, p < 0.0001, Table 2).
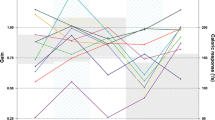
The head impulse gain of the VOR was decreased for the horizontal semicircular canal (HC, 0.89 ± 0.10 vs. 0.94 ± 0.05, p = 0.004, t-test), but was normal for the vertical semicircular canals (0.95 ± 0.11 vs. 0.96 ± 0.04, p = 0.427, t-test). Overall, 14 patients (54%) showed a subnormal gain for at least one of the semicircular canals, 38% (10/26) for the HC and 27% (7/26) for the vertical canals. The reduced gain for the HC was less commonly observed in patients with SCA2 (2/12, p = 0.022).
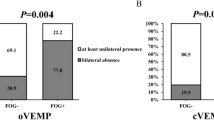
Nine patients (35%) exhibited abnormal oVEMP (n = 6, 23%) or cVEMP (n = 7, 27%) (Table 1). Of them, bilateral absence of responses was observed in seven, oVEMP in five and cVEMP in five. Two other patients with abnormal cVEMP were marked by a unilateral absence of wave formation, one (SCA1) of them with an asymmetry oVEMP at 36%.
Most patients with SCA1 (7/8, 88%) demonstrated various patterns of abnormal VEMPs [abnormal cVEMP in 6 (75%, median age 54, range 43–65), abnormal oVEMP in 5 (63%, median age 56, range 43–65)] while only two patients (14%) with SCA2 and none of the patients with SCA6 showed abnormal VEMP (Table 2).
Correlation between the symptoms and ocular motor/vestibular dysfunction
In the cross-analyses of the variables (Fisher's Exact Test), the patients with abnormal cVEMP or oVEMP showed a higher SARA score (p = 0.014) and a history of unpredicted falls (p = 0.046). Especially, the patients with abnormal oVEMP showed elevated SARA scores (p = 0.017) (Fig. 1B).
The frequency (A) and statistical significance (B) of ocular motor/vestibular dysfunction in patients with increased (median or higher) scores during each survey. The numbers in the small squares represent the proportion (A) and p-value obtained with Fisher’s exact test for cross-analysis (B). Darker shades in each square indicate higher proportion and lower p-values. DHI dizziness handicap inventory, EQ-5D-5L EuroQoL Five-Dimension, GEN gaze evoked nystagmus, HC horizontal semicircular canal, SARA Scale for the Assessment and Rating of Ataxia, SCA spinocerebellar ataxia, SVV subjective visual vertical, VC vertical semicircular canal, VEMP vestibular evoked myogenic potential, vHIT video head impulse test, VOR vestibulo-ocular reflex)
Discussion
We found a significant correlation between the VEMP abnormalities and unpredicted falls in patients with SCA, especially SCA1 Fig. 2.
Representative ocular motor and vestibular dysfunction in each patient with spinocerebellar ataxia type 1 and 2 (A–D). A 54-year-old woman with spinocerebellar ataxia (SCA) type 1 shows hypermetric horizontal saccades (A) and impaired smooth pursuit (B). Video head impulse tests (vHIT) show decreased gain of the vestibulo-ocular reflex (VOR) for left horizontal semicircular canal (C). Cervical and ocular vestibular evoked myogenic potentials (VEMPs) show no responses bilaterally (D). E–H A 40-year-old woman with SCA2 shows slow horizontal saccades (E) and impaired smooth pursuit (F). In contrast, the findings of vHIT (G), and ocular and cervical VEMPs are normal (H)
Previous studies have found falls as a critical detrimental factor for the QoL in patients with SCA. [10, 11] A retrospective analysis reported falls in nearly 70% of 228 patients with SCA, having resulted in significant trauma in approximately 70% of them. [11] The factors associated with a higher likelihood of falls included elevated SARA scores, longer disease duration, presence of pyramidal and extrapyramidal signs, and SCA3. [11] The authors suggested that the leg dystonia, which is more prevalent in SCA3, could have contributed to falls. [11] In our study, the prevalence of falls was rather low (38%) compared to that of the previous study. This may be attributed to the unpredicted nature of falls defined in our study. Otherwise, exclusion of the patients in more advanced stage may explain the low prevalence.
While falls may occur due to diverse causes, otolithic dysfunction is an independent predictor. [22] VEMPs can evaluate central as well as peripheral otolithic function. [21,22,23,24] Even though the relationship between falls and VEMP abnormalities in SCA requires further elucidation, it has been the subject of studies in patients with parkinsonism. [14, 25, 26] Vestibular dysfunction, especially delayed responses or reduced amplitude of oVEMP or cVEMP, is associated with frequent falling in patients with idiopathic Parkinson's disease and atypical parkinsonism. [14, 25] Since central otolithic projections ascend via the medial longitudinal fasciculus and descend via the medial vestibulospinal tract in the brainstem, abnormal VEMPs indicate altered processing of the otolithic information in the brainstem due to neurodegeneration in these disorders. [25] Thus, in conjunction with bradykinesia and rigidity, impaired otolithic information may lead to frequent falls in patients with Parkinson's disease. [25] Furthermore, the patients with progressive supranuclear palsy also show a decreased gain of the linear VOR and reduced amplitude of cVEMP, which may contribute to the postural instability and falls frequently observed in this disorder. [26]
A few studies on otolithic dysfunction have shown controversial results in SCA3. [27, 28] A study of 18 patients with SCA3 did not show any difference in the latency and amplitude of cVEMP between the patients and controls, but found a decrease in the VOR gain for six SCCs during vHIT. [27] On the contrary, another study found abnormalities of either oVEMP or cVEMP in 93% (13/14) of patients with SCA3, [28] which may be explained by involvement of the vestibular nuclei in SCA3. [27] These differences could be attributed to individual variation or dissimilar disease severity of the patients participated in those studies. [27]
In our study, we observed characteristic ocular motor findings for each subtype of SCAs as previously reported, such as slow saccades for SCA2 [7] and GEN with impaired VOR gain for SCA6. [29] Prior studies have shown that the ocular motor findings are more variable in SCA1. [4, 30] Our study could not identify distinctive ocular motor findings specific for SCA1, either.
However, we found significantly higher prevalence of unpredicted falls and VEMP abnormalities in SCA1 than in other subtypes. Previous pathologic studies also documented distinct involvements of the vestibular nuclei, vestibulocerebellum, and dentate nuclei in SCA1 while those were spared in SCA2. [31] The lateral and superior vestibular nuclei are more severely affected than the medial vestibular nuclei in the advanced stages. [32] These findings may explain the frequent falls and VEMP abnormalities observed in SCA1 compared to SCA2 even though the disease duration was similar between the groups. Likewise, the VOR gains were also subnormal during the rotatory chair and caloric tests [4] and vHIT in SCA1. [33] In contrast, the VOR and VEMPs are mostly preserved in SCA2 while saccadic slowing was most prominent. [7, 33, 34] These findings also indicate a relative sparing of the vestibular structures and a predilection of the premotor structures for horizontal saccades, which was also confirmed in pathologic studies in SCA2. [31, 32] The preserved VEMPs in SCA6 are consistent with pure cerebellar involvement and sparing of the brainstem in this disorder while GEN and impaired high-frequency VOR are mostly due to neurodegeneration involving the flocculus. [29, 35]
Our study has several limitations. First, due to the relatively small number of patients included, particularly in SCA6, the differences in scores observed across the subtypes may have been underestimated. Moreover, we enrolled the patients with relatively lower SARA scores, who were capable of completing all the vestibular function tests. This implies that individuals with higher SARA scores, not represented in this study, may have a greater propensity for falls. The lack of SCA3 patients in our study is also a limitation. This absence precludes a comparison with the previous studies on the prevalence of falls in SCAs, underscoring the need for future researches that involve SCA3 patients with a large scale cohort or focuses on each subtype of SCAs for more comprehensive analyses.
Conclusion
The unpredicted falls in SCA may be related to impaired processing of otolithic information, especially in type 1. The higher prevalence of unpredicted falls and abnormal VEMPs in SCA1 suggests potential involvements of the vestibular structures in the brainstem in this disorder. VEMP may assist in identifying the SCA patients with a risk of unpredicted falls and preventing fall-related injuries. Since the correlation does not necessarily imply causation, additional large-scale studies are required for further elucidation of this association.
Data Availability
Anonymized data will be shared by request from any qualified investigator.
References
Durr A (2010) Autosomal dominant cerebellar ataxias: polyglutamine expansions and beyond. Lancet Neurol 9:885–894
Jacobi H, du Montcel ST, Romanzetti S, Harmuth F, Mariotti C, Nanetti L, Rakowicz M, Makowicz G, Durr A, Monin ML, Filla A, Roca A, Schols L, Hengel H, Infante J, Kang JS, Timmann D, Casali C, Masciullo M, Baliko L, Melegh B, Nachbauer W, Burk-Gergs K, Schulz JB, Riess O, Reetz K, Klockgether T (2020) Conversion of individuals at risk for spinocerebellar ataxia types 1, 2, 3, and 6 to manifest ataxia (RISCA): a longitudinal cohort study. Lancet Neurol 19:738–747
Hekman KE, Gomez CM (2015) The autosomal dominant spinocerebellar ataxias: emerging mechanistic themes suggest pervasive Purkinje cell vulnerability. J Neurol Neurosurg Psychiatry 86:554–561
Burk K, Fetter M, Abele M, Laccone F, Brice A, Dichgans J, Klockgether T (1999) Autosomal dominant cerebellar ataxia type I: oculomotor abnormalities in families with SCA1, SCA2, and SCA3. J Neurol 246:789–797
Schmitz-Hubsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, Giunti P, Globas C, Infante J, Kang JS, Kremer B, Mariotti C, Melegh B, Pandolfo M, Rakowicz M, Ribai P, Rola R, Schols L, Szymanski S, van de Warrenburg BP, Durr A, Klockgether T, Fancellu R (2006) Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology 66:1717–1720
Leigh RJ, Zee DS (2015) The neurology of eye movements. Oxford University Press, Oxford; New York
Buttner N, Geschwind D, Jen JC, Perlman S, Pulst SM, Baloh RW (1998) Oculomotor phenotypes in autosomal dominant ataxias. Arch Neurol 55:1353–1357
Jacobi H, Schaprian T, Beyersmann J, Tezenas Montcel S, Schmid M, Klockgether T, Eurosca and Groups RS (2022) Evolution of disability in spinocerebellar ataxias type 1, 2, 3, and 6. Ann Clin Transl Neurol 9:286–295
Homann CN, Homann B, Ivanic G (2022) Accidental falls in patients with hyperkinetic movement disorders: a systematic review. Tremor Other Hyperkinet Mov (N Y) 12:30
Fonteyn EM, Schmitz-Hubsch T, Verstappen CC, Baliko L, Bloem BR, Boesch S, Bunn L, Charles P, Durr A, Filla A, Giunti P, Globas C, Klockgether T, Melegh B, Pandolfo M, De Rosa A, Schols L, Timmann D, Munneke M, Kremer BP, van de Warrenburg BP (2010) Falls in spinocerebellar ataxias: results of the EuroSCA Fall Study. Cerebellum 9:232–239
Fonteyn EM, Schmitz-Hubsch T, Verstappen CC, Baliko L, Bloem BR, Boesch S, Bunn L, Giunti P, Globas C, Klockgether T, Melegh B, Pandolfo M, Schols L, Timmann D, van de Warrenburg BP (2013) Prospective analysis of falls in dominant ataxias. Eur Neurol 69:53–57
Ozcan A, Donat H, Gelecek N, Ozdirenc M, Karadibak D (2005) The relationship between risk factors for falling and the quality of life in older adults. BMC Public Health 2005(5):90
Moreira-Gomes T, Nobrega C (2023) From the disruption of RNA metabolism to the targeting of RNA-binding proteins: the case of polyglutamine spinocerebellar ataxias. J Neurochem. https://doi.org/10.1111/jnc.16010
Venhovens J, Meulstee J, Bloem BR, Verhagen WIM (2020) Neurovestibular dysfunction and falls in parkinson’s disease and atypical parkinsonism: a prospective 1 year follow-up study. Front Neurol 11:580285
Yap KH, Azmin S, Che Hamzah J, Ahmad N, van de Warrenburg B, Mohamed Ibrahim N (2022) Pharmacological and non-pharmacological management of spinocerebellar ataxia: A systematic review. J Neurol 269:2315–2337
Jacobson GP, Newman CW (1990) The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg 116:424–427
Han GC, Lee EJ, Lee JH, Park SN, Lee HY, Jeon EJ, Lee H, Cheon BC, Kim JI, Gon EK, Koo JW, Ban JH, Sung KB (2004) The study of standardization for a Korean adaptation of self-report measures of dizziness. J Korean Bal Soc 3:307–325
Oppe M, Devlin NJ, van Hout B, Krabbe PF, de Charro F (2014) A program of methodological research to arrive at the new international EQ-5D-5L valuation protocol. Value Health 17:445–453
Lee SU, Kim HJ, Choi JY, Kim JS (2020) Ictal downbeat nystagmus in Meniere disease: A cross-sectional study. Neurology 95:e2409–e2417
Choi JH, Oh EH, Choi SY, Kim HJ, Lee SK, Choi JY, Kim JS, Choi KD (2022) Vestibular impairments in episodic ataxia type 2. J Neurol 269:2687–2695
Choi SY, Lee SH, Kim HJ, Kim JS (2014) Impaired modulation of the otolithic function in acute unilateral cerebellar infarction. Cerebellum 13:362–3711
Menant JC, St George RJ, Fitzpatrick RC, Lord SR (2012) Perception of the postural vertical and falls in older people. Gerontology 58:497–503
Venhovens J, Meulstee J, Verhagen WIM (2016) Vestibular evoked myogenic potentials (VEMPs) in central neurological disorders. Clin Neurophysiol 127:40–49
Wagner AR, Kobel MJ, Merfeld DM (2023) Increased roll tilt thresholds are associated with subclinical postural instability in asymptomatic adults aged 21 to 84 years. Front Aging Neurosci 15:1207711
Venhovens J, Meulstee J, Bloem BR, Verhagen WI (2016) Neurovestibular analysis and falls in Parkinson’s disease and atypical parkinsonism. Eur J Neurosci 43:1636–1646
Liao K, Wagner J, Joshi A, Estrovich I, Walker MF, Strupp M, Leigh RJ (2008) Why do patients with PSP fall? Evidence for abnormal otolith responses. Neurology 70:802–809
Geisinger D, Elyoseph Z, Zaltzman R, Mintz M, Gordon CR (2021) Angular vestibuloocular reflex loss with preserved saccular function in Machado-Joseph disease. J Neurol Sci 424:117393
Ribeiro RS, Pereira MM, Pedroso JL, Braga-Neto P, Barsottini OG, Manzano GM (2015) Cervical and ocular vestibular evoked potentials in Machado-Joseph disease: Functional involvement of otolith pathways. J Neurol Sci 358:294–298
Gomez CM, Thompson RM, Gammack JT, Perlman SL, Dobyns WB, Truwit CL, Zee DS, Clark HB, Anderson JH (1997) Spinocerebellar ataxia type 6: gaze-evoked and vertical nystagmus, Purkinje cell degeneration, and variable age of onset. Ann Neurol 42:933–950
Burk K, Abele M, Fetter M, Dichgans J, Skalej M, Laccone F, Didierjean O, Brice A, Klockgether T (1996) Autosomal dominant cerebellar ataxia type I clinical features and MRI in families with SCA1, SCA2 and SCA3. Brain 119(Pt 5):1497–1505
Iwabuchi K, Tsuchiya K, Uchihara T, Yagishita S (1999) Autosomal dominant spinocerebellar degenerations clinical, pathological, and genetic correlations. Rev Neurol 155:255–270
Rub U, Burk K, Timmann D, den Dunnen W, Seidel K, Farrag K, Brunt E, Heinsen H, Egensperger R, Bornemann A, Schwarzacher S, Korf HW, Schols L, Bohl J, Deller T (2012) Spinocerebellar ataxia type 1 (SCA1): new pathoanatomical and clinico-pathological insights. Neuropathol Appl Neurobiol 38:665–680
Luis L, Costa J, Munoz E, de Carvalho M, Carmona S, Schneider E, Gordon CR, Valls-Sole J (2016) Vestibulo-ocular reflex dynamics with head-impulses discriminates spinocerebellar ataxias types 1, 2 and 3 and Friedreich ataxia. J Vestib Res 26:327–334
Geiner S, Horn AK, Wadia NH, Sakai H, Buttner-Ennever JA (2008) The neuroanatomical basis of slow saccades in spinocerebellar ataxia type 2 (Wadia-subtype). Prog Brain Res 171:575–581
Lee SU, Kim JS, Kim HJ, Choi JY, Park JY, Kim JM, Yang X (2020) Evolution of the vestibular function during head impulses in spinocerebellar ataxia type 6. J Neurol 267:1672–1678
Funding
Open Access funding enabled and organized by Seoul National University. This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2021R1F1A1051464).
Author information
Authors and Affiliations
Contributions
CSY conducted the experiments, analyzed and interpreted the data, and wrote the manuscript. CKD and CJH conducted the experiments and analyzed and interpreted the data. KJS conducted the design and conceptualization of the study, interpretation of the data, and revised the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Drs. Choi SY, Choi JH, and Choi KD report no disclosure. Dr. Kim JS serves as an associate editor of Frontiers in Neuro-otology and on the editorial boards of the Journal of Clinical Neurology, Frontiers in Neuro-ophthalmology, Journal of Neuro-ophthalmology, Journal of Vestibular Research, and Clinical and Translational Neurology.
Ethical approval
This study followed the tenets of the Declaration of Helsinki and was performed according to the guidelines of Institutional Review Board of Pusan National University Hospital (2108–001-105).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Choi, SY., Choi, KD., Choi, JH. et al. Abnormal vestibular-evoked myogenic potentials as a risk factor for unpredicted falls in spinocerebellar ataxia: a preliminary study. J Neurol 271, 2539–2546 (2024). https://doi.org/10.1007/s00415-024-12195-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-024-12195-6