Abstract
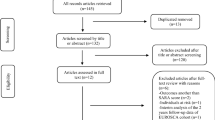
Spinocerebellar ataxias (SCA) comprise a rare, genetic subgroup within the degenerative ataxias and are dominantly inherited, with up to 48 recognized genetic subtypes. While an updated review on the management of degenerative ataxia is published recently, an evidence-based review focussed on the management of SCA is lacking. Here, we reviewed the pharmacological and non-pharmacological management of SCA by conducting a systematic review on Medline Ovid and Scopus. Of 29,284 studies identified, 47 studies (pharmacological: n = 25; non-pharmacological: n = 22) that predominantly involved SCA patients were included. Twenty studies had a high risk of bias based on the Cochrane’s Collaboration risk of bias tool. As per the European Federation of Neurological Societies 2004 guideline for therapeutic intervention, the remaining 27 studies were of Class I (n = 4) and Class II (n = 23) evidence. Only two therapies had Level A recommendations for the management of ataxia symptoms: riluzole and immediate in-patient neurorehabilitation. Ten therapies had Level B recommendations for managing ataxia symptoms and require further investigations with better study design. These include high dose valproate acid, branched-chain amino acid, intravenous trehalose; restorative rehabilitation using cycling regimen and videogame; and cerebellar stimulations using transcranial direct current stimulation and transcranial magnetic stimulation. Lithium and coaching on psychological adjustment received Level B recommendation for depressive symptoms and quality of life, respectively. Heterogeneous study designs, different genotypes, and non-standardized clinical measures alongside short duration and small sample sizes may hamper meaningful clinical translation. Therefore, rating of recommendations only serve as points of reference.

Similar content being viewed by others
Code availability
Not applicable.
References
Bodranghien F, Bastian A, Casali C, Hallett M, Louis ED, Manto M, Mariën P, Nowak DA, Schmahmann JD, Serrao M (2016) Consensus paper: revisiting the symptoms and signs of cerebellar syndrome. Cerebellum 15:369–391
Ruano L, Melo C, Silva MC, Coutinho P (2014) The global epidemiology of hereditary ataxia and spastic paraplegia: a systematic review of prevalence studies. Neuroepidemiology 42:174–183
Jacobi H, du Montcel ST, Bauer P, Giunti P, Cook A, Labrum R, Parkinson MH, Durr A, Brice A, Charles P (2015) Long-term disease progression in spinocerebellar ataxia types 1, 2, 3, and 6: a longitudinal cohort study. Lancet Neurol 14:1101–1108
Maschke M, Oehlert G, Xie TD, Perlman S, Subramony SH, Kumar N, Ptacek LJ, Gomez CM (2005) Clinical feature profile of spinocerebellar ataxia type 1–8 predicts genetically defined subtypes. Mov Disord 20:1405–1412
López-Bastida J, Perestelo-Pérez L, Montón-álvarez F, Serrano-Aguilar P (2008) Social economic costs and health-related quality of life in patients with degenerative cerebellar ataxia in Spain. Mov Disord 23:212–217
Diallo A, Jacobi H, Cook A, Labrum R, Durr A, Brice A, Charles P, Marelli C, Mariotti C, Nanetti L (2018) Survival in patients with spinocerebellar ataxia types 1, 2, 3, and 6 (EUROSCA): a longitudinal cohort study. Lancet Neurol 17:327–334
Bolton C, Lacy M (2019) Comparison of cognitive profiles in spinocerebellar ataxia subtypes: a case series. Cerebellum Ataxias 6:13–16
Klockgether T, Mariotti C, Paulson HL (2019) Spinocerebellar ataxia. Nat Rev Dis Primers 5:24
Stoodley CJ, Schmahmann JD (2010) Evidence for topographic organization in the cerebellum of motor control versus cognitive and affective processing. Cortex 46:831–844
Reeber SL, Otis TS, Sillitoe RV (2013) New roles for the cerebellum in health and disease. Front Syst Neurosci 7:1–11
Braga-Neto P, Pedroso JL, Alessi H, Dutra LA, Felício AC, Minett T, Weisman P, Santos-Galduroz RF, Bertolucci PHF, Gabbai AA (2012) Cerebellar cognitive affective syndrome in Machado Joseph disease: Core clinical features. Cerebellum 11:549–556
Coarelli G, Brice A, Durr A (2018) Recent advances in understanding dominant spinocerebellar ataxias from clinical and genetic points of view. F1000Research 7:1781–1790
Ashizawa T, Öz G, Paulson HL (2018) Spinocerebellar ataxias: prospects and challenges for therapy development. Nat Rev Neurol 14:590–605
Sarva H, Shanker VL (2014) Treatment options in degenerative cerebellar ataxia: a systematic review. Mov Disord Clin Pract 1:291–298
Page M, McKenzie JB, Boutron PMI, Hoffmann T, Mulrow CS, Tetzlaff JL, Akl E, Brennan S, Chou R, Glanville J, Grimshaw J, Hróbjartsson A, Lalu M, Li T, Loder E, Mayo-Wilson E, McDonald SM, Stewart LAL, Thomas J, Tricco A, Welch V, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA (2019) Assessing risk of bias in a randomized trial. In: Cochrane Handbook for Systematic Reviews of Interventions, pp 205–28
Brainin M, Barnes M, Baron JC, Gilhus N, Hughes R, Selmaj K, Waldemar G (2004) Guidance for the preparation of neurological management guidelines by EFNS scientific task forces–revised recommendations 2004. Eur J Neurol 11:577–581
Liu CS, Hsu HM, Cheng WL, Hsieh M (2005) Clinical and molecular events in patients with Machado-Joseph disease under lamotrigine therapy. Acta Neurol Scand 111:385–390
Sakai T, Matsuishi T, Yamada S, Komori H, Iwashita H (1995) Sulfamethoxazole-trimethoprim double-blind, placebo-controlled, crossover trial in Machado-Joseph disease: Sulfamethoxazole-trimethoprim increases cerebrospinal fluid level of biopterin. J Neural Transm/Gen Sect 102:159–172
Schulte T, Mattern R, Berger K, Szymanski S, Klotz P, Kraus PH, Przuntek H, Schöls L (2001) Double-blind crossover trial of trimethoprim-sulfamethoxazole in spinocerebellar ataxia type 3/Machado-Joseph disease. Arch Neurol 58:1451–1457
Sakai T, Antoku Y, Matsuishi T, Iwashita H (1996) Tetrahydrobiopterin double-blind, crossover trial in Machado-Joseph disease. J Neurol Sci 136:71–72
Wessel K, Langenberger K, Nitschke MF, Kömpf D (1997) Double-blind crossover study with physostigmine in patients with degenerative cerebellar diseases. Arch Neurol 54:397–400
Huang Y-Z, Chang Y-S, Hsu M-J, Wong AM, Chang Y-J (2015) Restoration of central programmed movement pattern by temporal electrical stimulation-assisted training in patients with spinal cerebellar atrophy. Neural Plast 2015:1–9
Hong JS, Kim JH, Yong SY, Lee YH, Kim SH, Park JY, Lee JK, Jang JY (2020) Preliminary clinical trial of balance compensation system for improvement of balance in patients with spinocerebellar ataxia. J Korean Acad Rehabil Med
Tsukahara A, Yoshida K, Matsushima A, Ajima K, Kuroda C, Mizukami N, Hashimoto M (2018) Effects of gait support in patients with spinocerebellar degeneration by a wearable robot based on synchronization control. J Neuroeng Rehabil 15:84
Romano S, Coarelli G, Marcotulli C, Leonardi L, Piccolo F, Spadaro M, Frontali M, Ferraldeschi M, Vulpiani MC, Ponzelli F (2015) Riluzole in patients with hereditary cerebellar ataxia: a randomised, double-blind, placebo-controlled trial. Lancet Neurol 14:985–991
Kobayashi K, Abe Y, Harada H, Oota E, Endo T, Takeda H (2019) Non-Clinical pharmacokinetic profiles of rovatirelin, an orally available thyrotropin-releasing hormone analogue. Xenobiotica 49:106–119
Saute JAM, de Castilhos RM, Monte TL, Schumacher-Schuh AF, Donis KC, D’Ávila R, Souza GN, Russo AD, Furtado GV, Gheno TC (2014) A randomized, phase 2 clinical trial of lithium carbonate in Machado-Joseph disease. Mov Disord 29:568–573
Lei L-F, Yang G-P, Wang J-L, Chuang D-M, Song W-H, Tang B-S, Jiang H (2016) Safety and efficacy of valproic acid treatment in SCA3/MJD patients. Parkinsonism Relat Disord 26:55–61
Zesiewicz TA, Greenstein P, Sullivan KL, Wecker L, Miller A, Jahan I, Chen R, Perlman S (2012) A randomized trial of varenicline (Chantix) for the treatment of spinocerebellar ataxia type 3. Neurology 78:545–550
Mori M, Adachi Y, Mori N, Kurihara S, Kashiwaya Y, Kusumi M, Takeshima T, Nakashima K (2002) Double-blind crossover study of branched-chain amino acid therapy in patients with spinocerebellar degeneration. J Neurol Sci 195:149–152
Zaltzman R, Elyoseph Z, Lev N, Gordon CR (2020) Trehalose in Machado-Joseph disease: safety, tolerability, and efficacy. Cerebellum 19:672–679
Velázquez-Pérez L, Rodríguez-Chanfrau J, García-Rodríguez JC, Sánchez-Cruz G, Aguilera-Rodríguez R, Rodríguez-Labrada R, Rodríguez-Díaz JC, Canales-Ochoa N, Gotay DA, Mederos LEA (2011) Oral zinc sulphate supplementation for six months in SCA2 patients: a randomized, double-blind, placebo-controlled trial. Neurochem Res 36:1793–1800
González C, Sánchez G, González Quevedo A, Delgado R, Velázquez L, García RJ (2005) Serum and cerebrospinal fluid levels of copper, iron and zinc in patiens with Ataxia type SCA-2 from the province of Holguin in Cuba. Ther Basic Dialogues Clin Neurosci 13:12–16
Bier JC, Dethy S, Hildebrand J, Jacquy J, Manto M, Martin J-J, Seeldrayers P (2003) Effects of the oral form of ondansetron on cerebellar dysfunction. J Neurol 250:693–697
Yabe I, Sasaki H, Yamashita I, Takei A, Tashiro K (2001) Clinical trial of acetazolamide in SCA6, with assessment using the Ataxia Rating Scale and body stabilometry. Acta Neurol Scand 104:44–47
Takei A, Fukazawa T, Hamada T, Sohma H, Yabe I, Sasaki H, Tashiro K (2004) Effects of tandospirone on “5-HT1A receptor-associated symptoms” in patients with Machado-Josephe disease: an open-label study. Clin Neuropharmacol 27:9–13
Takei A, Hamada S, Homma S, Hamada K, Tashiro K, Hamada T (2010) Difference in the effects of tandospirone on ataxia in various types of spinocerebellar degeneration: an open-label study. Cerebellum 9:567–570
Noorasyikin M, Elena A, Teh P, Waheeda TF, Hajar MS, Long K, Norlinah M (2020) Oral trehalose maybe helpful for patients with spinocerebellar ataxia 3 and should be better evaluated. Parkinsonism Relat Disord 70:42–44
Tan S, Wang R-H, Niu H-X, Shi C-H, Mao C-Y, Zhang R, Song B, Sun S-L, Liu X-J, Hou H-M (2015) Nerve growth factor for the treatment of spinocerebellar ataxia type 3: An open-label study. Chin Med J 128:291–294
Jin J-L, Liu Z, Lu Z-J, Guan D-N, Wang C, Chen Z-B, Zhang J, Zhang W-Y, Wu J-Y, Xu Y (2013) Safety and efficacy of umbilical cord mesenchymal stem cell therapy in hereditary spinocerebellar ataxia. Curr Neurovasc Res 10:11–20
Tsai Y-A, Liu R-S, Lirng J-F, Yang B-H, Chang C-H, Wang Y-C, Wu Y-S, Ho JH-C, Lee OK, Soong B-W (2017) Treatment of spinocerebellar ataxia with mesenchymal stem cells: a phase I/IIa clinical study. Cell Transpl 26:503–512
Miyai I, Ito M, Hattori N, Mihara M, Hatakenaka M, Yagura H, Sobue G, Nishizawa M (2012) Cerebellar ataxia rehabilitation trial in degenerative cerebellar diseases. Neurorehabil Neural Repair 26:515–522
Rodríguez-Díaz JC, Velázquez-Pérez L, Rodríguez Labrada R, Aguilera Rodríguez R, Laffita Pérez D, Canales Ochoa N, Medrano Montero J, Estupiñán Rodríguez A, Osorio Borjas M, Góngora MM (2018) Neurorehabilitation therapy in spinocerebellar ataxia type 2: a 24-week, rater-blinded, randomized, controlled trial. Mov Disord 33:1481–1487
Tercero-Pérez K, Cortés H, Torres-Ramos Y, Rodríguez-Labrada R, Cerecedo-Zapata CM, Hernández-Hernández O, Pérez-González N, González-Piña R, Leyva-García N, Cisneros B (2019) Effects of physical rehabilitation in patients with spinocerebellar ataxia type 7. Cerebellum 18:397–405
Wang R-Y, Huang F-Y, Soong B-W, Huang S-F, Yang Y-R (2018) A randomized controlled pilot trial of game-based training in individuals with spinocerebellar ataxia type 3. Sci Rep 8:1–7
Bunn LM, Marsden JF, Giunti P, Day BL (2015) Training balance with opto-kinetic stimuli in the home: a randomized controlled feasibility study in people with pure cerebellar disease. Clin Rehabil 29:143–153
Kaut O, Jacobi H, Coch C, Prochnicki A, Minnerop M, Klockgether T, Wüllner U (2014) A randomized pilot study of stochastic vibration therapy in spinocerebellar ataxia. Cerebellum 13:237–242
Chang Y-J, Chou C-C, Huang W-T, Lu C-S, Wong AM, Hsu M-J (2015) Cycling regimen induces spinal circuitry plasticity and improves leg muscle coordination in individuals with spinocerebellar ataxia. Arch Phys Med Rehabil 96:1006–1013
Manor B, Greenstein PE, Davila-Perez P, Wakefield S, Zhou J, Pascual-Leone A (2019) Repetitive transcranial magnetic stimulation in spinocerebellar ataxia: a pilot randomized controlled trial. Front Neurol 10:73
França C, de Andrade DC, Silva V, Galhardoni R, Barbosa ER, Teixeira MJ and Cury RG (2020) Effects of cerebellar transcranial magnetic stimulation on ataxias: a randomized trial. Parkinsonism Relat Disord
Benussi A, Dell’Era V, Cotelli MS, Turla M, Casali C, Padovani A, Borroni B (2017) Long term clinical and neurophysiological effects of cerebellar transcranial direct current stimulation in patients with neurodegenerative ataxia. Brain Stimul 10:242–250
Benussi A, Dell’Era V, Cantoni V, Bonetta E, Grasso R, Manenti R, Cotelli M, Padovani A, Borroni B (2018) Cerebello-spinal tDCS in ataxia: a randomized, double-blind, sham-controlled, crossover trial. Neurology 91:e1090–e1101
Burciu RG, Fritsche N, Granert O, Schmitz L, Spönemann N, Konczak J, Theysohn N, Gerwig M, van Eimeren T, Timmann D (2013) Brain changes associated with postural training in patients with cerebellar degeneration: a voxel-based morphometry study. J Neurosci 33:4594–4604
Keller JL, Bastian AJ (2014) A home balance exercise program improves walking in people with cerebellar ataxia. Neurorehabil Neural Repair 28:770–778
Santos G, Zeigelboim DBS, Severiano M, Teive H, Liberalesso P, Marques J, Cordeiro M (2017) Feasibility of virtual reality-based balance rehabilitation in adults with spinocerebellar ataxia: a prospective observational study. Hear Balance Commun 15:244–251
Zimmet AM, Cowan NJ, Bastian AJ (2019) Patients with cerebellar ataxia do not benefit from limb weights. Cerebellum 18:128–136
Horiuchi M, Maki F, Yanagisawa T, Sugihara H, Takahashi Y, Ohashi K, Sasaka K, Nakajima Y (2002) Therapeutic efficacy of transcranial magnetic stimulation for amyotrophic lateral sclerosis and spinocerebellar degeneration. In: International Congress Series. Elsevier, pp 525–32
Leonardi L, Aceto MG, Marcotulli C, Arcuria G, Serrao M, Pierelli F, Paone P, Filla A, Roca A, Casali C (2017) A wearable proprioceptive stabilizer for rehabilitation of limb and gait ataxia in hereditary cerebellar ataxias: a pilot open-labeled study. Neurol Sci 38:459–463
Nunes MB, Martinez ARM, Rezende TJR, Friedman JH, Lopes-Cendes I, D’Abreu A, França MC Jr (2015) Dystonia in Machado-Joseph disease: clinical profile, therapy and anatomical basis. Parkinsonism Relat Disord 21:1441–1447
Kanai K, Kuwabara S, Arai K, Sung JY, Ogawara K, Hattori T (2003) Muscle cramp in Machado-Joseph disease: altered motor axonal excitability properties and mexiletine treatment. Brain 126:965–973
Sacca F, Puorro G, Brunetti A, Capasso G, Cervo A, Cocozza S, de Leva M, Marsili A, Pane C, Quarantelli M (2015) A randomized controlled pilot trial of lithium in spinocerebellar ataxia type 2. J Neurol 262:149–153
Monte TL, Rieder C, Tort A, Rockenback I, Pereira M, Silveira I, Ferro A, Sequeiros J, Jardim LB (2003) Use of fluoxetine for treatment of Machado-Joseph disease: an open-label study. Acta Neurol Scand 107:207–210
Izumi S-I, Ando K, Ono M, Suzukamo Y, Michimata A, Fukuhara S (2007) Effect of coaching on psychological adjustment in patients with spinocerebellar degeneration: a pilot study. Clin Rehabil 21:987–996
Silva RCRd, Saute JAM, Silva ACFd, Coutinho ACdO, Saraiva-Pereira M, Jardim LB (2010) Occupational therapy in spinocerebellar ataxia type 3: an open-label trial. Braz J Med Biol Res 43:537–542
Nishizawa M, Onodera O, Hirakawa A, Shimizu Y, Yamada M (2020) Effect of rovatirelin in patients with cerebellar ataxia: two randomised double-blind placebo-controlled phase 3 trials. J Neurol Neurosurg Psychiatry 91:254–262
Kretschmer BD, Kratzer U, Schmidt WJ (1998) Riluzole, a glutamate release inhibitor, and motor behavior. Naunyn Schmiedebergs Arch Pharmacol 358:181–190
de Silva R, Greenfield J, Cook A, Bonney H, Vallortigara J, Hunt B, Giunti P (2019) Guidelines on the diagnosis and management of the progressive ataxias. Orphanet J Rare Dis 14:1–10
Olsson C, Jansson HN, Swenson J (2016) The role of trehalose for the stabilization of proteins. J Phys Chem B 120:4723–4731
Sarkar S, Davies JE, Huang Z, Tunnacliffe A, Rubinsztein DC (2007) Trehalose, a novel mTOR-independent autophagy enhancer, accelerates the clearance of mutant huntingtin and α-synuclein. J Biol Chem 282:5641–5652
Tanji K, Miki Y, Maruyama A, Mimura J, Matsumiya T, Mori F, Imaizumi T, Itoh K, Wakabayashi K (2015) Trehalose intake induces chaperone molecules along with autophagy in a mouse model of Lewy body disease. Biochem Biophys Res Commun 465:746–752
Felice VD, Quigley EM, Sullivan AM, O’Keeffe GW, O’Mahony SM (2016) Microbiota-gut-brain signalling in Parkinson’s disease: Implications for non-motor symptoms. Parkinsonism Relat Disord 27:1–8
Guillén-Rogel P, San Emeterio C, Marín PJ (2017) Associations between ankle dorsiflexion range of motion and foot and ankle strength in young adults. J Phys Ther Sci 29:1363–1367
Warburton DE, Bredin SS, Horita LT, Zbogar D, Scott JM, Esch BT, Rhodes RE (2007) The health benefits of interactive video game exercise. Appl Physiol Nutr Metab 32:655–663
Reetz K, Costa AS, Mirzazade S, Lehmann A, Juzek A, Rakowicz M, Boguslawska R, Schöls L, Linnemann C, Mariotti C (2013) Genotype-specific patterns of atrophy progression are more sensitive than clinical decline in SCA1, SCA3 and SCA6. Brain 136:905–917
Velázquez-Pérez L, Rodríguez-Diaz JC, Rodríguez-Labrada R, Medrano-Montero J, Aguilera Cruz AB, Reynaldo-Cejas L, Góngora-Marrero M, Estupiñán-Rodríguez A, Vázquez-Mojena Y, Torres-Vega R (2019) Neurorehabilitation improves the motor features in prodromal SCA2: a randomized, controlled trial. Mov Disord 34:1060–1068
Acknowledgements
This review was funded by Dana Impak Perdana Grant (DIP-2019-007) received by NMI from Universiti Kebangsaan Malaysia.
Funding
This review was funded by Dana Impak Perdana Grant (DIP-2019–007) received by NMI from Universiti Kebangsaan Malaysia.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Funding acquisition was performed by NMI and SA; Literature search was performed by KHY and SA. The first draft of this review was written by KHY, and all authors critically revised the work. All authors read and approved the final version of the review.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yap, K.H., Azmin, S., Che Hamzah, J. et al. Pharmacological and non-pharmacological management of spinocerebellar ataxia: A systematic review. J Neurol 269, 2315–2337 (2022). https://doi.org/10.1007/s00415-021-10874-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10874-2