Abstract
Frontotemporal lobar degeneration (FTLD) with TDP-43-immunoreactive inclusions (FTLD–TDP) is a neurodegenerative disease associated with clinical, genetic, and neuropathological heterogeneity. An association between TDP-43, FTLD and amyotrophic lateral sclerosis (ALS) was first described in 2006. However, a century before immunohistochemistry existed, atypical dementias displaying behavioral, language and/or pyramidal symptoms and showing non-specific FTLD with superficial cortical neuronal loss, gliosis and spongiosis were often confused with Alzheimer’s or Pick’s disease. Initially this pathology was termed dementia lacking distinctive histopathology (DLDH), but this was later renamed when ubiquitinated inclusions originally found in ALS were also discovered in (DLDH), thus warranting a recategorization as FTLD-U (ubiquitin). Finally, the ubiquitinated protein was identified as TDP-43, which aggregates in cortical, subcortical, limbic and brainstem neurons and glial cells. The topography and morphology of TDP-43 inclusions associate with specific clinical syndromes and genetic mutations which implies different pathomechanisms that are yet to be discovered; hence, the TDP-43 journey has actually just begun. In this review, we describe how FTLD–TDP was established and defined clinically and neuropathologically throughout the past century.



Similar content being viewed by others
References
Onari K, Spatz H (1926) Anatomische Beiträge zur Lehre von der Pickschen umschriebenen Großhirnrinden-Atrophie (“Picksche Krankheit”) [Anatomical contributions to the theory of Pick’s circumscribed cerebral cortex atrophy (Pick’s disease]. Z Ges Neurol Psychiat 101:470–511
McKhann GM, Albert MS, Grossman M, Miller B, Dickson D, Trojanowski JQ (2001) Clinical and pathological diagnosis of frontotemporal dementia: report of the Work Group on Frontotemporal Dementia and Pick’s Disease. Arch Neurol 58:1803–1809
Josephs KA, Hodges JR, Snowden JS, Mackenzie IR, Neumann M, Mann DM, Dickson DW (2011) Neuropathological background of phenotypical variability in frontotemporal dementia. Acta Neuropathol 122:137–153
Hutton M, Lendon CL, Rizzu P, Baker M, Froelich S, Houlden H, Pickering-Brown S, Chakraverty S, Isaacs A, Grover A, Hackett J, Adamson J, Lincoln S, Dickson D, Davies P, Petersen RC, Stevens M, de Graaff E, Wauters E, van Baren J, Hillebrand M, Joosse M, Kwon JM, Nowotny P, Che LK, Norton J, Morris JC, Reed LA, Trojanowski J, Basun H, Lannfelt L, Neystat M, Fahn S, Dark F, Tannenberg T, Dodd PR, Hayward N, Kwok JB, Schofield PR, Andreadis A, Snowden J, Craufurd D, Neary D, Owen F, Oostra BA, Hardy J, Goate A, van Swieten J, Mann D, Lynch T, Heutink P (1998) Association of missense and 5’-splice-site mutations in tau with the inherited dementia FTDP-17. Nature 393:702–705
Arai T, Hasegawa M, Akiyama H, Ikeda K, Nonaka T, Mori H, Mann D, Tsuchiya K, Yoshida M, Hashizume Y, Oda T (2006) TDP-43 is a component of ubiquitin-positive tau-negative inclusions in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Biochem Biophys Res Commun 351:602–611
Neumann M, Sampathu DM, Kwong LK, Truax AC, Micsenyi MC, Chou TT, Bruce J, Schuck T, Grossman M, Clark CM, McCluskey LF, Miller BL, Masliah E, Mackenzie IR, Feldman H, Feiden W, Kretzschmar HA, Trojanowski JQ, Lee VM (2006) Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science 314:130–133
Kwiatkowski TJ Jr, Bosco DA, Leclerc AL, Tamrazian E, Vanderburg CR, Russ C, Davis A, Gilchrist J, Kasarskis EJ, Munsat T, Valdmanis P, Rouleau GA, Hosler BA, Cortelli P, de Jong PJ, Yoshinaga Y, Haines JL, Pericak-Vance MA, Yan J, Ticozzi N, Siddique T, McKenna-Yasek D, Sapp PC, Horvitz HR, Landers JE, Brown RH Jr (2009) Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science 323:1205–1208
Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, Freedman M, Kertesz A, Robert PH, Albert M, Boone K, Miller BL, Cummings J, Benson DF (1998) Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology 51:1546–1554
Snowden J, Neary D, Mann D (2007) Frontotemporal lobar degeneration: clinical and pathological relationships. Acta Neuropathol 114:31–38
Pick A (1892) Über die Beziehungen der senilen Hirnatrophie zur Aphasie [The relation between senile brain atrophy and aphasia]. Prag Med Wochenschr 17:165–167
Pick A (1901) Senile Hirnatrophie als Grundlage von Herderscheinungen [Senile brain atrophy as the basis of focal symptoms]. Wien Klin Wochenschr 14:403–404
Pick A (1904) Zur Symptomatologie der linksseitigen Schläfenlappenatrophie [On the symptomatology of left-sided temporal lobe atrophy]. Monatsschr Psychiatr Neurol 16:378–388
Pick A (1904) Über primäre progressive Demenz bei Erwachsenen [On primary progressive dementia of adults]. Prag Med Wochenschr 29:417–420
Pick A (1906) Über einen weiteren symptomencomplex in Rahmen des Dementia senilis, bedingt durch umschriebene sträkere Hirnatrophie (gemischte Apraxie) [About another complex of symptoms in the context of dementia senilis, caused by circumscribed severe cerebral atrophy (mixed apraxia)]. Monatsschr Psychiatr Neurol 19:97–108
Pick A, Girling DM, Berrios GE (1994) On the relationship between senile cerebral atrophy and aphasia. Hist Psychiatry 5:542–547
Pick A, Girling DM, Markova IS (1995) Senile Hirnatrophie als Grundlage von Herderscheinungen: (Senile cerebral atrophy as the origin of focal symptoms. Hist Psychiatry 6:533–537
Pick A, Girling DM, Berrios GE (1997) On the symptomatology of left-sided temporal lobe atrophy. Hist Psychiatry 8:149–159
Brion S, Plas J, Jeanneau A (1991) Pick’s disease. anatomo-clinical point of view. Rev Neurol 147:693–704
Mesulam MM (1982) Slowly progressive aphasia without generalized dementia. Ann Neurol 11:592–598
Poeck K, Luzzatti C (1988) Slowly progressive aphasia in three patients. The problem of accompanying neuropsychological deficit. Brain 111(1):151–168
Kertesz A, Davidson W, McCabe P (1998) Primary progressive semantic aphasia: a case study. J Int Neuropsychol Soc 4:388–398
Hodges JR, Patterson K, Oxbury S, Funnell E (1992) Semantic dementia. Progressive fluent aphasia with temporal lobe atrophy. Brain 115(6):1783–1806
Spatt J (2003) Arnold Pick’s concept of dementia. Cortex 39:525–531
Derouesne C (2014) From Arnold Pick’s original descriptions to frontotemporal dementia: the present enlightened by the past an historical approach. Geriatr Psychol Neuropsychiatr Vieil 12:74–84
Kertesz A (2004) Frontotemporal dementia/Pick’s disease. Arch Neurol 61:969–971
Gans A (1923) Betrachtungen über Art und Ausbreitung des krankhaften Prozesses in einem Fall von Pickscher Atrophie des Stirnhirns [Reflections on the nature and spread of the disease process in a case of Pick’s atrophy of the frontal lobe]. Z Ges Neurol Psychiat 80:10–28
Alzheimer A (1911) Über eigenartige Krankheitsfälle des späteren Alters [On certain peculiar diseases of old age]. Z Ges Neurol Psychiat 4:356–385
Alzheimer A (1991) Über eigenartige Krankheitsfälle des späteren Alters: (On certain peculiar diseases of old age). Hist Psychiatry 2:74–101
Dickson DW (2001) Neuropathology of Pick’s disease. Neurology 56:S16-20
Schneider C (1927) Üeber Picksche Krankheit. [Pick’s disease]. Monatsschr Psychiatr Neurol 65:230–275
Schneider C (1929) Weitere Beiträge zur Lehre von der Pickschen Krankheit [Further contributions to the theory of Pick’s disease]. Z Ges Neurol Psychiat 120:340–384
Grünthal E (1930) Über ein Brüderpaar mit Pickscher Krankheit: Eine vergleichende Untersuchung, zugleich ein Beitrag zur Kenntnis der Verursachung und des Verlaufs der Erkrankung. [Two brothers with Pick’s disease: a comparative study and contribution to the knowledge of the cause and the course of the disease.]. Z Ges Neurol Psychiat 129:350–375
Braunmühl V A, Leonhard K (1934) Über ein Schwesternpaar mit Pickscher Krankheit [On a pair of sisters with Pick’s disease]. Z Ges Neurol Psychiat 150:209–241
Verhaart WJC (1930) Over de ziekte van Pick [About Pick’s disease]. Nederl Tijdschr Geneesk 74:5586–5598
Malamud N, Waggoner RW (1943) Genealogic and clinicopathologic study of Pick’s disease. Arch Neurol Psychiat 50:288–303
Keddie KM (1967) Presenile dementia, clinically of the Pick’s disease variety, occurring in a mother and daughter. Int J Neuropsychiatry 3:182–187
Ferraro A, Jervis A (1936) Pick’s disease: clinicopathologic study with report of two cases. Arch NeurPsych 36:739–767
Delay J, Brion S, Escourolle R (1957) Limites et conception actuelle de la maladie de Pick : son diagnostic différentiel [Limits & current concept of Pick’s disease; its differential diagnosis]. Ann Med Psychol (Paris) 115:609–634
Thibodeau MP, Miller BL (2013) ‘Limits and current knowledge of Pick’s disease: its differential diagnosis’. A translation of the 1957 Delay, Brion. Escourolle article. Neurocase 19:417–422
Neumann MA (1949) Pick’s disease. J Neuropathol Exp Neurol 8:255–282
Hassin GB, Levitin D (1941) Pick’s disease: clinicopathologic study and report of a case. Arch NeurPsych 45:814–833
Löwenberg K (1936) Pick’s disease: a clinicopathologic contribution. Arch Neurol Psychiatry 36:768–789
Kahn E, Thompson LJ (1934) Concerning Pick’s disease. Am J Psychiatry 90:937–946
Stern K, Reed GE (1945) Presenile dementia (Alzheimer’s disease). Am J Psychiatry 102:191–197
Marchand L, Anglade R, Fretet J, Rougean M, Roan P (1938) La maladie de Pick, la maladie d’Alzheimer, et la démence sénile sans athérome cérébral sont-elles les trois modalités d’un même processus dégénératif [Are Pick’s disease, Alzheimer’s disease and senile dementia without atherosclerosis all the same degenerative process]. Ann Med Psychol 96:249–255
Marchand L (1937) La démence sénile sans atherome cérébral. Ses rapports avec la maladie d’Alzheimer et la maladie de Pick. Considerations sur les encephaloses [Senile dementia without atherosclerosis; Its relation with Alzheimer’s and Pick’s disease. Considerations on encephalosis]. Ann Med Psychol 95:680–735
Delay J, Brion S, Badaracco JC (1955) Le diagnostic différentiel des maladies de Pick et d’Alzhiemer (A propos de 12 observations anatomo-cliniques) [Differential diagnosis of Pick’s disease from Alzheimer’s disease; anatomical and clinical observations on 12 cases]. Encephale 44:454–499
Spatz H (1952) La maladie de Pick les atrophies systématisées progressives et la sénescence cérébrale prématurée localisée. 1er congres international d’histopathologie du système nerveux [Pick’s disease, progressive atrophy and premature localized cerebral senescence. 1st international conference on nervous system histopathology]. 2:375–406
Escourolle R (1956) La maladie de Pick. Etude d’ensemble et synthèse anatomo-clinique [Pick’s disease: critical study and anatomo-clinical summary]. In:Dissertation, Paris
Rewcastle NB, Ball MJ (1968) Electron microscopic structure of the “inclusion bodies” in Pick’s disease. Neurology 18:1205–1213
Brion S, Mikol J (1971) Ultrastructural study of Pick’s disease. Apropos of 3 cases. Rev Neurol 125:273–286
Brion S, Mikol J, Psimaras A (1973) Recent findings in Pick’s disease. In: Zimmerman HM (ed) Progress in neuropathology. Grune and Stratton, New York, pp 421–452
Constantinidis J, Richard J, Tissot R (1974) Pick’s disease. Histological and clinical correlations. Eur Neurol 11:208–217
Papageorgiou SG, Beratis IN, Horvath J, Herrmann FR, Bouras C, Kövari E (2016) Amnesia in frontotemporal dementia: shedding light on the Geneva historical data. J Neurol 263:657–664
Brion S (1977) Les demences preseniles [Presenile dementias]. In: Encycl. Med. Chir. 37 545, A10, Paris, pp 1–16
Masse G, Mikol J, Brion S (1981) Atypical presenile dementia: Report of an anatomo-clinical case and review of the literature. J Neurol Sci 52:245–267
Brun A, Gustafson L (1978) Limbic lobe involvement in presenile dementia. Arch Psychiatr Nervenkr (1970) 226:79–93
Brun A, Gustafson L (1976) Distribution of cerebral degeneration in Alzheimer’s disease. A clinico-pathological study. Arch Psychiatr Nervenkr (1970) 223:15–33
Neumann MA, Cohn R (1967) Progressive subcortical gliosis, a rare form of presenile dementia. Brain 90:405–418
Akelaitis AJ (1944) Atrophy of basal ganglia in Pick’s disease Clinicopathologic Study. Arch Neurol Psychiatr 51:27–34
Kim RC, Collins GH, Parisi JE, Wright AW, Chu YB (1981) Familial dementia of adult onset with pathological findings of a “non-specific” nature. Brain 104:61–78
Schaumburg HH, Suzuki K (1968) Non-specific familial presenile dementia. J Neurol Neurosurg Psychiatr 31:479–486
Clark AW, White CL, Manz HJ, Parhad IM, Curry B, Whitehouse PJ, Lehmann J, Coyle JT (1986) Primary degenerative dementia without Alzheimer pathology. Can J Neurol Sci 13:462–470
Hughes CP, Myers FK, Smith K, Torack RM (1973) Nosologic problems in dementia. A clinical and pathologic study of 11 cases. Neurology 23:344–351
Morris JC, Cole M, Banker BQ, Wright D (1984) Hereditary dysphasic dementia and the Pick-Alzheimer spectrum. Ann Neurol 16:455–466
Cole M, Wright D, Banker BQ (1979) Familial aphasia due to Pick’s disease. Ann Neurol 6:158
Cole M, Wright D, Banker BQ (1979) Familial aphasia: the Pick-Alzheimer spectrum. Trans Am Neurol Assoc 104:175–179
Lendon CL, Lynch T, Norton J, McKeel DW Jr, Busfield F, Craddock N, Chakraverty S, Gopalakrishnan G, Shears SD, Grimmett W, Wilhelmsen KC, Hansen L, Morris JC, Goate AM (1998) Hereditary dysphasic disinhibition dementia: a frontotemporal dementia linked to 17q21-22. Neurology 50:1546–1555
Behrens MI, Mukherjee O, Tu PH, Liscic RM, Grinberg LT, Carter D, Paulsmeyer K, Taylor-Reinwald L, Gitcho M, Norton JB, Chakraverty S, Goate AM, Morris JC, Cairns NJ (2007) Neuropathologic heterogeneity in HDDD1: a familial frontotemporal lobar degeneration with ubiquitin-positive inclusions and progranulin mutation. Alzheimer Dis Assoc Disord 21:1–7
Mehler MF, Horoupian DS, Davies P, Dickson DW (1987) Reduced somatostatin-like immunoreactivity in cerebral cortex in nonfamilial dysphasic dementia. Neurology 37:1448–1453
Dejerine J, Serieux P (1897) Un cas de surdité verbale pure, terminée par aphasie sensorielle, suivi d’autopsie [A case of pure word deafness terminating in sensory aphasia, followed by autopsy]. C R Soc Biol 49:1074–1077
Heath PD, Kennedy P, Kapur N (1983) Slowly progressive aphasia without generalized dementia. Ann Neurol 13:687–688
Chawluk JB, Mesulam MM, Hurtig H, Kushner M, Weintraub S, Saykin A, Rubin N, Alavi A, Reivich M (1986) Slowly progressive aphasia without generalized dementia: studies with positron emission tomography. Ann Neurol 19:68–74
Kirshner HS, Webb WG, Kelly MP, Wells CE (1984) Language disturbance. An initial symptom of cortical degenerations and dementia. Arch Neurol 41:491–496
Mesulam MM, Weintraub S (1992) Spectrum of primary progressive aphasia. Baillieres Clin Neurol 1:583–609
Mesulam MM (2001) Primary progressive aphasia. Ann Neurol 49:425–432
Mesulam MM (1987) Primary progressive aphasia–differentiation from Alzheimer’s disease. Ann Neurol 22:533–534
Snowden JS, Neary D, Mann DM, Goulding PJ, Testa HJ (1992) Progressive language disorder due to lobar atrophy. Ann Neurol 31:174–183
Kirshner HS, Tanridag O, Thurman L, Whetsell WO Jr (1987) Progressive aphasia without dementia: two cases with focal spongiform degeneration. Ann Neurol 22:527–532
Green J, Morris JC, Sandson J, McKeel DW Jr, Miller JW (1990) Progressive aphasia: a precursor of global dementia? Neurology 40:423–429
Warrington EK (1975) The selective impairment of semantic memory. Q J Exp Psychol 27:635–657
Snowden J, Goulding P, Neary D (1989) Semantic Dementia: a form of circumscribed cerebral atrophy. Behav Neurol 2:167–182
Neary D, Snowden JS, Northen B, Goulding P (1988) Dementia of frontal lobe type. J Neurol Neurosurg Psychiatr 51:353–361
Rowland LP (2001) How amyotrophic lateral sclerosis got its name: the clinical-pathologic genius of jean-martin charcot. Arch Neurol 58:512–515
Androp S (1940) Amyotrophic lateral sclerosis with psychosis. Psychiatr Q 14:818–825
Ziegler LH (1930) Psychotic and emotional phenomena associated with amyotrophic lateral sclerosis. Arch Neurol Psychiatry 24:930–936
Westphal A (1925) Schizophrene Krankheitsprozesse und amyotrophische Lateralsklerose [Schizophrenic disease processes and amyotrophic lateral sclerosis]. Arch Psychiat Nervenkr 74:310–325
Wechsler IS, Davison C (1932) Amyotrophic lateral sclerosis with mental symptoms. Arch Neurol Psychiatr 27:859–880
Meyer A (1929) Über eine der amyotrophischen Lateralsklerose nahestehende Erkrankung mit psychischen Störungen [About a disease related to amyotrophic lateral sclerosis with mental disorders]. Z Ges Neurol Psychiat 121:107–138
v. Bagh K, (1941) Über anatomische Befunde bei 30 Fällen von systematischer Atrophie der Großhirnrinde (Pickscher Krankheit) mit besonderer Berücksichtigung der Stammganglien und der langen absteigenden Leitungsbahnen. Eine vorläufige Mitteilung [Anatomic findings in 30 cases of systemic atrophy of the cerebral cortex (Pick’s disease) with particular attention to the basal ganglia and the long descending pathways. A preliminary communication]. Arch Psychiat Nervenkr 114:68–70
Hirano A, Kurland LT, Krooth RS, Lessell S (1961) Parkinsonism-dementia complex, an endemic disease on the island of Guam I clinical features. Brain 84:642–661
Bonduelle M, Bouygues P, Escourolle R, Lormeau G (1968) Simultaneous development of amyotrophic lateral sclerosis, Parkinson’s syndrome and progressive dementia. Apropos of 2 anatomoclinical cases. Attempted interpretation. J Neurol Sci 6:315–332
Mitsuyama Y, Takamiya S (1979) Presenile dementia with motor neuron disease in Japan. A new entity? Arch Neurol 36:592–593
Horoupian DS, Thal L, Katzman R, Terry RD, Davies P, Hirano A, DeTeresa R, Fuld PA, Petito C, Blass J et al (1984) Dementia and motor neuron disease: morphometric, biochemical, and Golgi studies. Ann Neurol 16:305–313
Neary D, Snowden JS, Mann DM, Northen B, Goulding PJ, Macdermott N (1990) Frontal lobe dementia and motor neuron disease. J Neurol Neurosurg Psychiatry 53:23–32
Neary D, Snowden J, Mann D (2005) Frontotemporal dementia. Lancet Neurol 4:771–780
Morita K, Kaiya H, Ikeda T, Namba M (1987) Presenile dementia combined with amyotrophy: a review of 34 Japanese cases. Arch Gerontol Geriatr 6:263–277
Salazar AM, Masters CL, Gajdusek DC, Gibbs CJ Jr (1983) Syndromes of amyotrophic lateral sclerosis and dementia: relation to transmissible Creutzfeldt-Jakob disease. Ann Neurol 14:17–26
Brun A (2007) Identification and characterization of frontal lobe degeneration: historical perspective on the development of FTD. Alzheimer Dis Assoc Disord 21:S3-4
Neary D, Snowden JS, Bowen DM, Sims NR, Mann DM, Benton JS, Northen B, Yates PO, Davison AN (1986) Neuropsychological syndromes in presenile dementia due to cerebral atrophy. J Neurol Neurosurg Psychiatry 49:163–174
Gustafson L (1987) Frontal lobe degeneration of non-Alzheimer type. II. Clinical picture and differential diagnosis. Arch Gerontol Geriatr 6:209–223
Brun A (1987) Frontal lobe degeneration of non-Alzheimer type I Neuropathology. Arch Gerontol Geriatr 6:193–208
Risberg J (1987) Frontal lobe degeneration of non-Alzheimer type. III. Regional cerebral blood flow. Arch Gerontol Geriatr 6:225–233
Englund E, Brun A (1987) Frontal lobe degeneration of non-Alzheimer type. IV White Matter Changes. Arch Gerontol Geriatr 6:235–243
Gustafson L, Brun A, Passant U (1992) Frontal lobe degeneration of non-Alzheimer type Baillieres. Clin Neurol 1:559–582
Brun A, Gustafson L (2011) The birth and early evolution of the frontotemporal dementia (FTD) concept. J Mol Neurosci 45:324–329
Johanson A, Hagberg B (1989) Psychometric characteristics in patients with frontal lobe degeneration of non-Alzheimer type. Arch Gerontol Geriatr 8:129–137
Förstl H, Hentschel F, Besthorn C, Geiger-Kabisch C, Sattel H, Schreiter-Gasser U, Bayerl JR, Schmitz F, Schmitt HP (1994) Frontal and temporal onset of brain atrophy. Clinical and instrumental findings]. Nervenarzt 65:611–618
Filley CM, Kleinschmidt-De Masters BK, Gross KF (1994) Non-Alzheimer fronto-temporal degenerative dementia. A neurobehavioral and pathologic study. Clin Neuropathol 13:109–116
Knopman DS, Mastri AR, Frey WH 2nd, Sung JH, Rustan T (1990) Dementia lacking distinctive histologic features: a common non-Alzheimer degenerative dementia. Neurology 40:251–256
Knopman DS (1993) Overview of dementia lacking distinctive histology: pathological designation of a progressive dementia. Dementia 4:132–136
Miller BL, Cummings JL, Villanueva-Meyer J, Boone K, Mehringer CM, Lesser IM, Mena I (1991) Frontal lobe degeneration: clinical, neuropsychological, and SPECT characteristics. Neurology 41:1374–1382
Benson DF (1993) Progressive frontal dysfunction. Dementia 4:149–153
Risberg J, Passant U, Warkentin S, Gustafson L (1993) Regional cerebral blood flow in frontal lobe dementia of non-Alzheimer type. Dementia 4:186–187
Miller BL, Chang L, Mena I, Boone K, Lesser IM (1993) Progressive right frontotemporal degeneration: clinical, neuropsychological and SPECT characteristics. Dementia 4:204–213
Friedland RP, Koss E, Lerner A, Hedera P, Ellis W, Dronkers N, Ober BA, Jagust WJ (1993) Functional imaging, the frontal lobes, and dementia. Dementia 4:192–203
Brown J, Gydesen S, Sorensen SA, Brun A, Duff K, Houlden H, Fidani L, Kullkarni S, Cummings J, Goate A et al (1993) Exclusion mapping in familial non-specific dementia. Dementia 4:163–166
Edvinsson L, Minthon L, Ekman R, Gustafson L (1993) Neuropeptides in cerebrospinal fluid of patients with Alzheimer’s disease and dementia with frontotemporal lobe degeneration. Dementia 4:167–171
Francis PT, Holmes C, Webster MT, Stratmann GC, Procter AW, Bowen DM (1993) Preliminary neurochemical findings in non-Alzheimer dementia due to lobar atrophy. Dementia 4:172–177
Brun A (1993) Frontal lobe degeneration of non-Alzheimer type revisited. Dementia 4:126–131
Mann DM, South PW, Snowden JS, Neary D (1993) Dementia of frontal lobe type: neuropathology and immunohistochemistry. J Neurol Neurosurg Psychiatry 56:605–614
Liu X, Brun A (1996) Regional and laminar synaptic pathology in frontal lobe degeneration of non-alzheimer type. Int J Geriatr Psychiatry 11:47–55
Liu X, Erikson C, Brun A (1996) Cortical synaptic changes and gliosis in normal aging, Alzheimer’s disease and frontal lobe degeneration. Dementia 7:128–134
Cooper PN, Jackson M, Lennox G, Lowe J, Mann DM (1995) Tau, ubiquitin, and alpha B-crystallin immunohistochemistry define the principal causes of degenerative frontotemporal dementia. Arch Neurol 52:1011–1015
Groups TLaM (1994) Clinical and neuropathological criteria for frontotemporal dementia. J Neurol Neurosurg Psychiatry 57:416–418
Dickson DW, Kouri N, Murray ME, Josephs KA (2011) Neuropathology of frontotemporal lobar degeneration-tau (FTLD-tau). J Mol Neurosci 45:384–389
Cairns NJ, Bigio EH, Mackenzie IRA, Neumann M, Lee VMY, Hatanpaa KJ, White CL, Schneider JA, Grinberg LT, Halliday G, Duyckaerts C, Lowe JS, Holm IE, Tolnay M, Okamoto K, Yokoo H, Murayama S, Woulfe J, Munoz DG, Dickson DW, Ince PG, Trojanowski JQ, Mann DMA (2007) Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: consensus of the Consortium for frontotemporal lobar degeneration. Acta Neuropathol 114:5–22
Forman MS, Farmer J, Johnson JK, Clark CM, Arnold SE, Coslett HB, Chatterjee A, Hurtig HI, Karlawish JH, Rosen HJ, Van Deerlin V, Lee VM, Miller BL, Trojanowski JQ, Grossman M (2006) Frontotemporal dementia: clinicopathological correlations. Ann Neurol 59:952–962
Leigh PN, Anderton BH, Dodson A, Gallo JM, Swash M, Power DM (1988) Ubiquitin deposits in anterior horn cells in motor neurone disease. Neurosci Lett 93:197–203
Lowe J, Lennox G, Jefferson D, Morrell K, McQuire D, Gray T, Landon M, Doherty FJ, Mayer RJ (1988) A filamentous inclusion body within anterior horn neurones in motor neurone disease defined by immunocytochemical localisation of ubiquitin. Neurosci Lett 94:203–210
Wightman G, Anderson VE, Martin J, Swash M, Anderton BH, Neary D, Mann D, Luthert P, Leigh PN (1992) Hippocampal and neocortical ubiquitin-immunoreactive inclusions in amyotrophic lateral sclerosis with dementia. Neurosci Lett 139:269–274
Okamoto K, Murakami N, Kusaka H, Yoshida M, Hashizume Y, Nakazato Y, Matsubara E, Hirai S (1992) Ubiquitin-positive intraneuronal inclusions in the extramotor cortices of presenile dementia patients with motor neuron disease. J Neurol 239:426–430
Jackson M, Lennox G, Lowe J (1996) Motor neurone disease-inclusion dementia. Neurodegeneration 5:339–350
Tolnay M, Probst A (1995) Frontal lobe degeneration: novel ubiquitin-immunoreactive neurites within frontotemporal cortex. Neuropathol Appl Neurobiol 21:492–497
Lipton AM, White CL 3rd, Bigio EH (2004) Frontotemporal lobar degeneration with motor neuron disease-type inclusions predominates in 76 cases of frontotemporal degeneration. Acta Neuropathol 108:379–385
Johnson JK, Diehl J, Mendez MF, Neuhaus J, Shapira JS, Forman M, Chute DJ, Roberson ED, Pace-Savitsky C, Neumann M, Chow TW, Rosen HJ, Forstl H, Kurz A, Miller BL (2005) Frontotemporal lobar degeneration: demographic characteristics of 353 patients. Arch Neurol 62:925–930
Hodges JR, Davies RR, Xuereb JH, Casey B, Broe M, Bak TH, Kril JJ, Halliday GM (2004) Clinicopathological correlates in frontotemporal dementia. Ann Neurol 56:399–406
Josephs KA, Holton JL, Rossor MN, Godbolt AK, Ozawa T, Strand K, Khan N, Al-Sarraj S, Revesz T (2004) Frontotemporal lobar degeneration and ubiquitin immunohistochemistry. Neuropathol Appl Neurobiol 30:369–373
Shi J, Shaw CL, Du Plessis D, Richardson AMT, Bailey KL, Julien C, Stopford C, Thompson J, Varma A, Craufurd D, Tian J, Pickering-Brown S, Neary D, Snowden JS, Mann DMA (2005) Histopathological changes underlying frontotemporal lobar degeneration with clinicopathological correlation. Acta Neuropathol 110:501–512
Neary D, Snowden JS, Mann DM (2000) Classification and description of frontotemporal dementias. Ann N Y Acad Sci 920:46–51
Mackenzie IR, Shi J, Shaw CL, Duplessis D, Neary D, Snowden JS, Mann DM (2006) Dementia lacking distinctive histology (DLDH) revisited. Acta Neuropathol 112:551–559
Josephs KA, Jones AG, Dickson DW (2004) Hippocampal sclerosis and ubiquitin-positive inclusions in dementia lacking distinctive histopathology. Dement Geriatr Cogn Disord 17:342–345
Nakano I (2000) Frontotemporal dementia with motor neuron disease (amyotrophic lateral sclerosis with dementia). Neuropathology 20:68–75
Mackenzie IR, Feldman H (2003) The relationship between extramotor ubiquitin-immunoreactive neuronal inclusions and dementia in motor neuron disease. Acta Neuropathol 105:98–102
Josephs KA, Knopman DS, Whitwell JL, Boeve BF, Parisi JE, Petersen RC, Dickson DW (2005) Survival in two variants of tau-negative frontotemporal lobar degeneration: FTLD-U vs FTLD-MND. Neurology 65:645–647
Mackenzie IR, Baborie A, Pickering-Brown S, Du Plessis D, Jaros E, Perry RH, Neary D, Snowden JS, Mann DM (2006) Heterogeneity of ubiquitin pathology in frontotemporal lobar degeneration: classification and relation to clinical phenotype. Acta Neuropathol 112:539–549
Sampathu DM, Neumann M, Kwong LK, Chou TT, Micsenyi M, Truax A, Bruce J, Grossman M, Trojanowski JQ, Lee VM (2006) Pathological heterogeneity of frontotemporal lobar degeneration with ubiquitin-positive inclusions delineated by ubiquitin immunohistochemistry and novel monoclonal antibodies. Am J Pathol 169:1343–1352
Baker M, Mackenzie IR, Pickering-Brown SM, Gass J, Rademakers R, Lindholm C, Snowden J, Adamson J, Sadovnick AD, Rollinson S, Cannon A, Dwosh E, Neary D, Melquist S, Richardson A, Dickson D, Berger Z, Eriksen J, Robinson T, Zehr C, Dickey CA, Crook R, McGowan E, Mann D, Boeve B, Feldman H, Hutton M (2006) Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17. Nature 442:916–919
Josephs KA, Ahmed Z, Katsuse O, Parisi JF, Boeve BF, Knopman DS, Petersen RC, Davies P, Duara R, Graff-Radford NR, Uitti RJ, Rademakers R, Adamson J, Baker M, Hutton ML, Dickson DW (2007) Neuropathologic features of frontotemporal lobar degeneration with ubiquitin-positive inclusions with progranulin gene (PGRN) mutations. J Neuropathol Exp Neurol 66:142–151
Mackenzie IR, Baker M, Pickering-Brown S, Hsiung GY, Lindholm C, Dwosh E, Gass J, Cannon A, Rademakers R, Hutton M, Feldman HH (2006) The neuropathology of frontotemporal lobar degeneration caused by mutations in the progranulin gene. Brain 129:3081–3090
Morita M, Al-Chalabi A, Andersen PM, Hosler B, Sapp P, Englund E, Mitchell JE, Habgood JJ, de Belleroche J, Xi J, Jongjaroenprasert W, Horvitz HR, Gunnarsson LG, Brown RH Jr (2006) A locus on chromosome 9p confers susceptibility to ALS and frontotemporal dementia. Neurology 66:839–844
Vance C, Al-Chalabi A, Ruddy D, Smith BN, Hu X, Sreedharan J, Siddique T, Schelhaas HJ, Kusters B, Troost D, Baas F, de Jong V, Shaw CE (2006) Familial amyotrophic lateral sclerosis with frontotemporal dementia is linked to a locus on chromosome 9p13.2-21.3. Brain 129:868–876
Forman MS, Mackenzie IR, Cairns NJ, Swanson E, Boyer PJ, Drachman DA, Jhaveri BS, Karlawish JH, Pestronk A, Smith TW, Tu PH, Watts GD, Markesbery WR, Smith CD, Kimonis VE (2006) Novel ubiquitin neuropathology in frontotemporal dementia with valosin-containing protein gene mutations. J Neuropathol Exp Neurol 65:571–581
Cairns NJ, Neumann M, Bigio EH, Holm IE, Troost D, Hatanpaa KJ, Foong C, White CL 3rd, Schneider JA, Kretzschmar HA, Carter D, Taylor-Reinwald L, Paulsmeyer K, Strider J, Gitcho M, Goate AM, Morris JC, Mishra M, Kwong LK, Stieber A, Xu Y, Forman MS, Trojanowski JQ, Lee VM, Mackenzie IR (2007) TDP-43 in familial and sporadic frontotemporal lobar degeneration with ubiquitin inclusions. Am J Pathol 171:227–240
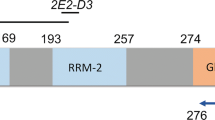
Kawakami I, Arai T, Hasegawa M (2019) The basis of clinicopathological heterogeneity in TDP-43 proteinopathy. Acta Neuropathol 138:751–770
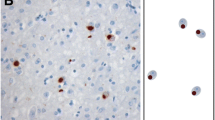
Davidson Y, Kelley T, Mackenzie IR, Pickering-Brown S, Du Plessis D, Neary D, Snowden JS, Mann DM (2007) Ubiquitinated pathological lesions in frontotemporal lobar degeneration contain the TAR DNA-binding protein, TDP-43. Acta Neuropathol 113:521–533
Neumann M, Kwong LK, Truax AC, Vanmassenhove B, Kretzschmar HA, Van Deerlin VM, Clark CM, Grossman M, Miller BL, Trojanowski JQ, Lee VM (2007) TDP-43-positive white matter pathology in frontotemporal lobar degeneration with ubiquitin-positive inclusions. J Neuropathol Exp Neurol 66:177–183
Neumann M, Mackenzie IR, Cairns NJ, Boyer PJ, Markesbery WR, Smith CD, Taylor JP, Kretzschmar HA, Kimonis VE, Forman MS (2007) TDP-43 in the ubiquitin pathology of frontotemporal dementia with VCP gene mutations. J Neuropathol Exp Neurol 66:152–157
Hatanpaa KJ, Bigio EH, Cairns NJ, Womack KB, Weintraub S, Morris JC, Foong C, Xiao G, Hladik C, Mantanona TY, White CL 3rd (2008) TAR DNA-binding protein 43 immunohistochemistry reveals extensive neuritic pathology in FTLD-U: a midwest-southwest consortium for FTLD study. J Neuropathol Exp Neurol 67:271–279
Josephs KA, Stroh A, Dugger B, Dickson DW (2009) Evaluation of subcortical pathology and clinical correlations in FTLD-U subtypes. Acta Neuropathol 118:349–358
Mackenzie IR, Neumann M (2017) Reappraisal of TDP-43 pathology in FTLD-U subtypes. Acta Neuropathol 134:79–96
Mackenzie IR, Neumann M (2020) Subcortical TDP-43 pathology patterns validate cortical FTLD-TDP subtypes and demonstrate unique aspects of C9orf72 mutation cases. Acta Neuropathol 139:83–98
Thorpe JR, Tang H, Atherton J, Cairns NJ (2008) Fine structural analysis of the neuronal inclusions of frontotemporal lobar degeneration with TDP-43 proteinopathy. J Neural Transm 115:1661–1671
Josephs KA, Zhang YJ, Baker M, Rademakers R, Petrucelli L, Dickson DW (2019) C-terminal and full length TDP-43 specie differ according to FTLD-TDP lesion type but not genetic mutation. Acta Neuropathol Commun 7:100
Kametani F, Obi T, Shishido T, Akatsu H, Murayama S, Saito Y, Yoshida M, Hasegawa M (2016) Mass spectrometric analysis of accumulated TDP-43 in amyotrophic lateral sclerosis brains. Sci Rep 6:23281
Igaz LM, Kwong LK, Xu Y, Truax AC, Uryu K, Neumann M, Clark CM, Elman LB, Miller BL, Grossman M, McCluskey LF, Trojanowski JQ, Lee VM (2008) Enrichment of C-terminal fragments in TAR DNA-binding protein-43 cytoplasmic inclusions in brain but not in spinal cord of frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Am J Pathol 173:182–194
Lee EB, Lee VM, Trojanowski JQ (2011) Gains or losses: molecular mechanisms of TDP43-mediated neurodegeneration. Nat Rev Neurosci 13:38–50
Winton MJ, Igaz LM, Wong MM, Kwong LK, Trojanowski JQ, Lee VM (2008) Disturbance of nuclear and cytoplasmic TAR DNA-binding protein (TDP-43) induces disease-like redistribution, sequestration, and aggregate formation. J Biol Chem 283:13302–13309
Jung Y, Duffy JR, Josephs KA (2013) Primary progressive aphasia and apraxia of speech. Semin Neurol 33:342–347
Whitwell JL, Josephs KA (2012) Recent advances in the imaging of frontotemporal dementia. Curr Neurol Neurosci Rep 12:715–723
Whitwell JL (2019) FTD spectrum: neuroimaging across the FTD spectrum. Prog Mol Biol Transl Sci 165:187–223
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, Ogar JM, Rohrer JD, Black S, Boeve BF, Manes F, Dronkers NF, Vandenberghe R, Rascovsky K, Patterson K, Miller BL, Knopman DS, Hodges JR, Mesulam MM, Grossman M (2011) Classification of primary progressive aphasia and its variants. Neurology 76:1006–1014
Gorno-Tempini ML, Dronkers NF, Rankin KP, Ogar JM, Phengrasamy L, Rosen HJ, Johnson JK, Weiner MW, Miller BL (2004) Cognition and anatomy in three variants of primary progressive aphasia. Ann Neurol 55:335–346
DeJesus-Hernandez M, Mackenzie IR, Boeve BF, Boxer AL, Baker M, Rutherford NJ, Nicholson AM, Finch NA, Flynn H, Adamson J, Kouri N, Wojtas A, Sengdy P, Hsiung GY, Karydas A, Seeley WW, Josephs KA, Coppola G, Geschwind DH, Wszolek ZK, Feldman H, Knopman DS, Petersen RC, Miller BL, Dickson DW, Boylan KB, Graff-Radford NR, Rademakers R (2011) Expanded GGGGCC hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron 72:245–256
Renton AE, Majounie E, Waite A, Simón-Sánchez J, Rollinson S, Gibbs JR, Schymick JC, Laaksovirta H, van Swieten JC, Myllykangas L, Kalimo H, Paetau A, Abramzon Y, Remes AM, Kaganovich A, Scholz SW, Duckworth J, Ding J, Harmer DW, Hernandez DG, Johnson JO, Mok K, Ryten M, Trabzuni D, Guerreiro RJ, Orrell RW, Neal J, Murray A, Pearson J, Jansen IE, Sondervan D, Seelaar H, Blake D, Young K, Halliwell N, Callister JB, Toulson G, Richardson A, Gerhard A, Snowden J, Mann D, Neary D, Nalls MA, Peuralinna T, Jansson L, Isoviita VM, Kaivorinne AL, Hölttä-Vuori M, Ikonen E, Sulkava R, Benatar M, Wuu J, Chiò A, Restagno G, Borghero G, Sabatelli M, Heckerman D, Rogaeva E, Zinman L, Rothstein JD, Sendtner M, Drepper C, Eichler EE, Alkan C, Abdullaev Z, Pack SD, Dutra A, Pak E, Hardy J, Singleton A, Williams NM, Heutink P, Pickering-Brown S, Morris HR, Tienari PJ, Traynor BJ (2011) A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron 72:257–268
Mackenzie IR, Neumann M, Baborie A, Sampathu DM, Du Plessis D, Jaros E, Perry RH, Trojanowski JQ, Mann DM, Lee VM (2011) A harmonized classification system for FTLD-TDP pathology. Acta Neuropathol 122:111–113
Lee EB, Porta S, Michael Baer G, Xu Y, Suh E, Kwong LK, Elman L, Grossman M, Lee VM, Irwin DJ, Van Deerlin VM, Trojanowski JQ (2017) Expansion of the classification of FTLD-TDP: distinct pathology associated with rapidly progressive frontotemporal degeneration. Acta Neuropathol 134:65–78
Takeuchi R, Tada M, Shiga A, Toyoshima Y, Konno T, Sato T, Nozaki H, Kato T, Horie M, Shimizu H, Takebayashi H, Onodera O, Nishizawa M, Kakita A, Takahashi H (2016) Heterogeneity of cerebral TDP-43 pathology in sporadic amyotrophic lateral sclerosis: evidence for clinico-pathologic subtypes. Acta Neuropathol Commun 4:61
Tan RH, Guennewig B, Dobson-Stone C, Kwok JBJ, Kril JJ, Kiernan MC, Hodges JR, Piguet O, Halliday GM (2019) The underacknowledged PPA-ALS: a unique clinicopathologic subtype with strong heritability. Neurology 92:e1354–e1366
Nishihira Y, Gefen T, Mao Q, Appin C, Kohler M, Walker J, Rademakers R, Rademaker A, Rogalski E, Weintraub S, Geula C, Mesulam MM, Bigio EH (2019) Revisiting the utility of TDP-43 immunoreactive (TDP-43-ir) pathology to classify FTLD-TDP subtypes. Acta Neuropathol 138:167–169
Neumann M, Lee EB, Mackenzie IR (2021) Frontotemporal lobar degeneration TDP-43-Immunoreactive pathological subtypes: clinical and mechanistic significance. Adv Exp Med Biol 1281:201–217
Sommer W (1880) Erkrankung des Ammonshornes als aetiologisches Moment der Epilepsie [Disease of the Ammon’s horn as an etiological element of epilepsy]. Arch Psychiatr Nervenkr 10:361–375
Thom M (2009) Hippocampal sclerosis: progress since Sommer. Brain Pathol 19:565–572
Crystal HA, Dickson DW, Sliwinski MJ, Lipton RB, Grober E, Marks-Nelson H, Antis P (1993) Pathological markers associated with normal aging and dementia in the elderly. Ann Neurol 34:566–573
Dickson DW, Davies P, Bevona C, Van Hoeven KH, Factor SM, Grober E, Aronson MK, Crystal HA (1994) Hippocampal sclerosis: a common pathological feature of dementia in very old (> or = 80 years of age) humans. Acta Neuropathol 88:212–221
Jellinger KA (1994) Hippocampal sclerosis: a common pathological feature of dementia in very old humans. Acta Neuropathol 88:599
Ala TA, Beh GO, Frey WH 2nd (2000) Pure hippocampal sclerosis: a rare cause of dementia mimicking Alzheimer’s disease. Neurology 54:843–848
Jellinger K (2000) Pure hippocampal sclerosis: a rare cause of dementia mimicking Alzheimer’s disease. Neurology 55:739–740
Leverenz JB, Agustin CM, Tsuang D, Peskind ER, Edland SD, Nochlin D, DiGiacomo L, Bowen JD, McCormick WC, Teri L, Raskind MA, Kukull WA, Larson EB (2002) Clinical and neuropathological characteristics of hippocampal sclerosis: a community-based study. Arch Neurol 59:1099–1106
Corey-Bloom J, Sabbagh MN, Bondi MW, Hansen L, Alford MF, Masliah E, Thal LJ (1997) Hippocampal sclerosis contributes to dementia in the elderly. Neurology 48:154–160
Rasmusson DX, Brandt J, Steele C, Hedreen JC, Troncoso JC, Folstein MF (1996) Accuracy of clinical diagnosis of Alzheimer disease and clinical features of patients with non-Alzheimer disease neuropathology. Alzheimer Dis Assoc Disord 10:180–188
Blass DM, Hatanpaa KJ, Brandt J, Rao V, Steinberg M, Troncoso JC, Rabins PV (2004) Dementia in hippocampal sclerosis resembles frontotemporal dementia more than Alzheimer disease. Neurology 63:492–497
Toyoshima Y, Piao YS, Tan CF, Morita M, Tanaka M, Oyanagi K, Okamoto K, Takahashi H (2003) Pathological involvement of the motor neuron system and hippocampal formation in motor neuron disease-inclusion dementia. Acta Neuropathol 106:50–56
Hatanpaa KJ, Blass DM, Pletnikova O, Crain BJ, Bigio EH, Hedreen JC, White CL 3rd, Troncoso JC (2004) Most cases of dementia with hippocampal sclerosis may represent frontotemporal dementia. Neurology 63:538–542
Barker WW, Luis CA, Kashuba A, Luis M, Harwood DG, Loewenstein D, Waters C, Jimison P, Shepherd E, Sevush S, Graff-Radford N, Newland D, Todd M, Miller B, Gold M, Heilman K, Doty L, Goodman I, Robinson B, Pearl G, Dickson D, Duara R (2002) Relative frequencies of Alzheimer disease, lewy body, vascular and frontotemporal dementia, and hippocampal sclerosis in the state of Florida brain bank. Alzheimer Dis Assoc Disord 16:203–212
Josephs KA, Parisi JE, Knopman DS, Boeve BF, Petersen RC, Dickson DW (2006) Clinically undetected motor neuron disease in pathologically proven frontotemporal lobar degeneration with motor neuron disease. Arch Neurol 63:506–512
Josephs KA, Dickson DW (2007) Hippocampal sclerosis in tau-negative frontotemporal lobar degeneration. Neurobiol Aging 28:1718–1722
Josephs KA, Whitwell JL, Jack CR, Parisi JE, Dickson DW (2006) Frontotemporal lobar degeneration without lobar atrophy. Arch Neurol 63:1632–1638
Kipps CM, Hodges JR, Hornberger M (2010) Nonprogressive behavioural frontotemporal dementia: recent developments and clinical implications of the ‘bvFTD phenocopy syndrome.’ Curr Opin Neurol 23:628–632
Amador-Ortiz C, Ahmed Z, Zehr C, Dickson DW (2007) Hippocampal sclerosis dementia differs from hippocampal sclerosis in frontal lobe degeneration. Acta Neuropathol 113:245–252
Amador-Ortiz C, Lin WL, Ahmed Z, Personett D, Davies P, Duara R, Graff-Radford NR, Hutton ML, Dickson DW (2007) TDP-43 immunoreactivity in hippocampal sclerosis and Alzheimer’s disease. Ann Neurol 61:435–445
Josephs KA, Mackenzie I, Frosch MP, Bigio EH, Neumann M, Arai T, Dugger BN, Ghetti B, Grossman M, Hasegawa M, Herrup K, Holton J, Jellinger K, Lashley T, McAleese KE, Parisi JE, Revesz T, Saito Y, Vonsattel JP, Whitwell JL, Wisniewski T, Hu W (2019) LATE to the PART-y. Brain 142:47
Wider C, Dickson DW, Stoessl AJ, Tsuboi Y, Chapon F, Gutmann L, Lechevalier B, Calne DB, Personett DA, Hulihan M, Kachergus J, Rademakers R, Baker MC, Grantier LL, Sujith OK, Brown L, Calne S, Farrer MJ, Wszolek ZK (2009) Pallidonigral TDP-43 pathology in Perry syndrome. Parkinsonism Relat Disord 15:281–286
Yokota O, Davidson Y, Bigio EH, Ishizu H, Terada S, Arai T, Hasegawa M, Akiyama H, Sikkink S, Pickering-Brown S, Mann DM (2010) Phosphorylated TDP-43 pathology and hippocampal sclerosis in progressive supranuclear palsy. Acta Neuropathol 120:55–66
Koga S, Sanchez-Contreras M, Josephs KA, Uitti RJ, Graff-Radford N, van Gerpen JA, Cheshire WP, Wszolek ZK, Rademakers R, Dickson DW (2017) Distribution and characteristics of transactive response DNA binding protein 43 kDa pathology in progressive supranuclear palsy. Mov Disord 32:246–255
Uryu K, Nakashima-Yasuda H, Forman MS, Kwong LK, Clark CM, Grossman M, Miller BL, Kretzschmar HA, Lee VM, Trojanowski JQ, Neumann M (2008) Concomitant TAR-DNA-binding protein 43 pathology is present in Alzheimer disease and corticobasal degeneration but not in other tauopathies. J Neuropathol Exp Neurol 67:555–564
Koga S, Kouri N, Walton RL, Ebbert MTW, Josephs KA, Litvan I, Graff-Radford N, Ahlskog JE, Uitti RJ, van Gerpen JA, Boeve BF, Parks A, Ross OA, Dickson DW (2018) Corticobasal degeneration with TDP-43 pathology presenting with progressive supranuclear palsy syndrome: a distinct clinicopathologic subtype. Acta Neuropathol 136:389–404
Freeman SH, Spires-Jones T, Hyman BT, Growdon JH, Frosch MP (2008) TAR-DNA binding protein 43 in Pick disease. J Neuropathol Exp Neurol 67:62–67
Hasegawa M, Arai T, Akiyama H, Nonaka T, Mori H, Hashimoto T, Yamazaki M, Oyanagi K (2007) TDP-43 is deposited in the Guam parkinsonism-dementia complex brains. Brain 130:1386–1394
McKee AC, Gavett BE, Stern RA, Nowinski CJ, Cantu RC, Kowall NW, Perl DP, Hedley-Whyte ET, Price B, Sullivan C, Morin P, Lee HS, Kubilus CA, Daneshvar DH, Wulff M, Budson AE (2010) TDP-43 proteinopathy and motor neuron disease in chronic traumatic encephalopathy. J Neuropathol Exp Neurol 69:918–929
Josephs KA, Murray ME, Tosakulwong N, Whitwell JL, Knopman DS, Machulda MM, Weigand SD, Boeve BF, Kantarci K, Petrucelli L, Lowe VJ, Jack CR Jr, Petersen RC, Parisi JE, Dickson DW (2017) Tau aggregation influences cognition and hippocampal atrophy in the absence of beta-amyloid: a clinico-imaging-pathological study of primary age-related tauopathy (PART). Acta Neuropathol 133:705–715
Arai T, Mackenzie IR, Hasegawa M, Nonoka T, Niizato K, Tsuchiya K, Iritani S, Onaya M, Akiyama H (2009) Phosphorylated TDP-43 in Alzheimer’s disease and dementia with Lewy bodies. Acta Neuropathol 117:125–136
Schwab C, Arai T, Hasegawa M, Yu S, McGeer PL (2008) Colocalization of transactivation-responsive DNA-binding protein 43 and huntingtin in inclusions of Huntington disease. J Neuropathol Exp Neurol 67:1159–1165
Tan CF, Yamada M, Toyoshima Y, Yokoseki A, Miki Y, Hoshi Y, Kaneko H, Ikeuchi T, Onodera O, Kakita A, Takahashi H (2009) Selective occurrence of TDP-43-immunoreactive inclusions in the lower motor neurons in Machado-Joseph disease. Acta Neuropathol 118:553–560
Toyoshima Y, Tanaka H, Shimohata M, Kimura K, Morita T, Kakita A, Takahashi H (2011) Spinocerebellar ataxia type 2 (SCA2) is associated with TDP-43 pathology. Acta Neuropathol 122:375–378
Wilson AC, Dugger BN, Dickson DW, Wang DS (2011) TDP-43 in aging and Alzheimer’s disease—a review. Int J Clin Exp Pathol 4:147–155
Arnold SJ, Dugger BN, Beach TG (2013) TDP-43 deposition in prospectively followed, cognitively normal elderly individuals: correlation with argyrophilic grains but not other concomitant pathologies. Acta Neuropathol 126:51–57
Alzheimer A (1906) Über einen eigenartigen schweren Erkrankungsprozeβ der Hirnrincle [About a peculiar severe disease process of the cerebral cortex]. Neurol Central 25:1129–1136
Hippius H, Neundörfer G (2003) The discovery of Alzheimer’s disease. Dialogues Clin Neurosci 5:101–108
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7:263–269
Brooks BR, Miller RG, Swash M, Munsat TL (2000) El Escorial revisited: revised criteria for the diagnosis of amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 1:293–299
Al-Chalabi A, Hardiman O, Kiernan MC, Chiò A, Rix-Brooks B, van den Berg LH (2016) Amyotrophic lateral sclerosis: moving towards a new classification system. Lancet Neurol 15:1182–1194
Olney NT, Spina S, Miller BL (2017) Frontotemporal dementia. Neurol Clin 35:339–374
Snowden JS, Thompson JC, Stopford CL, Richardson AM, Gerhard A, Neary D, Mann DM (2011) The clinical diagnosis of early-onset dementias: diagnostic accuracy and clinicopathological relationships. Brain 134:2478–2492
Dickson DW (1998) Pick’s disease: a modern approach. Brain Pathol 8:339–354
Hyman BT, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Carrillo MC, Dickson DW, Duyckaerts C, Frosch MP, Masliah E, Mirra SS, Nelson PT, Schneider JA, Thal DR, Thies B, Trojanowski JQ, Vinters HV, Montine TJ (2012) National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimers Dement 8:1–13
Montine TJ, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Dickson DW, Duyckaerts C, Frosch MP, Masliah E, Mirra SS, Nelson PT, Schneider JA, Thal DR, Trojanowski JQ, Vinters HV, Hyman BT, Institute National, on Aging, Alzheimer’s Association, (2012) National Institute on Aging-Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol 123:1–11
Acknowledgements
We are grateful to Ms. Lea Dacy, Department of Neurology, Mayo Clinic, Rochester for her assistance. We also wish to thank the Mayo Clinic Libraries for providing materials for the literature review.
Funding
This study was funded by the National Institutes of Health grants R01 AG037491 and RF1 NS120992.
Author information
Authors and Affiliations
Contributions
AFC performed the literature search and prepared the original draft. KAJ had the idea for the article and critically revised the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Carlos, A.F., Josephs, K.A. Frontotemporal lobar degeneration with TAR DNA-binding protein 43 (TDP-43): its journey of more than 100 years. J Neurol 269, 4030–4054 (2022). https://doi.org/10.1007/s00415-022-11073-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11073-3