Abstract
Introduction
A horizontal vestibulo-ocular reflex gain (VOR gain) of < 0.6, measured by the video head impulse test (VHIT), is one of the diagnostic criteria for bilateral vestibulopathy (BV) according to the Báràny Society. Several VHIT systems are commercially available, each with different techniques of tracking head and eye movements and different methods of gain calculation. This study compared three different VHIT systems in patients diagnosed with BV.
Methods
This study comprised 46 BV patients (diagnosed according to the Báràny criteria), tested with three commercial VHIT systems (Interacoustics, Otometrics and Synapsys) in random order. Main outcome parameter was VOR gain as calculated by the system, and the agreement on BV diagnosis (VOR gain < 0.6) between the VHIT systems. Peak head velocities, the order effect and covert saccades were analysed separately, to determine whether these parameters could have influenced differences in outcome between VHIT systems.
Results
VOR gain in the Synapsys system differed significantly from VOR gain in the other two systems [F(1.256, 33.916) = 35.681, p < 0.000]. The VHIT systems agreed in 83% of the patients on the BV diagnosis. Peak head velocities, the order effect and covert saccades were not likely to have influenced the above mentioned results.
Conclusion
To conclude, using different VHIT systems in the same BV patient can lead to clinically significant differences in VOR gain, when using a cut-off value of 0.6. This might hinder proper diagnosis of BV patients. It would, therefore, be preferred that VHIT systems are standardised regarding eye and head tracking methods, and VOR gain calculation algorithms. Until then, it is advised to not only take the VOR gain in consideration when assessing a VHIT trial, but also look at the raw traces and the compensatory saccades.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bilateral vestibulopathy (BV) is a heterogeneous chronic condition in which the vestibular function is severely impaired or absent in both ears [1]. A greatly reduced or absent vestibulo-ocular reflex (VOR) is a main clinical marker of BV, among other symptoms [2]. To quantify the VOR function in all planes of the semicircular canals, the video head impulse test (VHIT) is widely used [3]. The vestibulo-ocular reflex gain (VOR gain) is considered to be the main outcome parameter of the VHIT. VOR gain represents the relationship between eye and head velocity, and can be calculated in various ways. For example, VOR gain can be calculated as the ratio between eye and head velocity at a certain point in time, at peak head velocity, or throughout the whole head movement (i.e. the area under the curve gain, regression analysis) [4,5,6]. VOR gain should be close to 1.0 in healthy subjects [7]. Therefore, a decreased VOR function should result in a decreased VOR gain. Moreover, a horizontal angular VOR gain of < 0.6 on both sides, as measured by the VHIT, is one of the diagnostic criteria for BV according to the Bárány Society [8].
BV patients can also show catch-up saccades during the VHIT. These saccades are a compensation mechanism for the retinal slip during head movements, and can occur during or shortly after a head impulse (“covert” saccades and “overt” saccades, respectively). As an adaptation effect, the latency of the catch-up saccades can decrease and therefore, the amount of covert saccades can increase [9]. These covert saccades could influence VOR gain calculations, especially when area under the curve gain calculation is used.
Several VHIT systems are commercially available, each with different methods of gain calculation and different techniques of tracking eye and head movements. Small study populations show significant differences in VOR gain between different VHIT systems within healthy subjects and patients. Despite these differences in VOR gain, all systems identified vestibular deficits similarly [5, 6]. It is unknown what the effect of using different VHIT systems is on the VOR gain in subjects with severely impaired vestibular function on both ears. In case the use of different VHIT systems would result in different clinical diagnoses within the same patient (e.g. classifying a patient “yes” or “no” with BV), it might be necessary to standardise systems regarding VOR gain calculation algorithms and eye and head tracking methods.
Objective of this study was to compare three commercial VHIT systems (Interacoustics, Otometrics, and Synapsys) in a large group of BV patients. Main outcome parameters were horizontal VOR gain as calculated by the system, and the agreement between the systems on identifying BV according to the diagnostic criteria (horizontal VOR gain < 0.6). Since there are technological differences inherent to the VHIT systems (i.e. different VOR gain calculation algorithms and different head and eye tracking), it was hypothesised that different VHIT systems could lead to clinically relevant differences in VHIT outcome within the same BV patient.
Methods
Study population
This study comprised 46 patients diagnosed with BV at the Division of Balance Disorders at Maastricht University Hospital, based on the diagnostic criteria for BV from the Bárány Society [8]. Since VOR gain obtained by VHIT was used as an outcome parameter in this study, this criterium was removed from the inclusion criteria. Patients diagnosed with BV solely based on VHIT outcomes were, therefore, not part of this study population. Inclusion criteria comprised (1) reduced caloric response (sum of bithermal maximum peak slow phase eye velocities of < 6°/s on each side), (2) and/or reduced horizontal angular VOR gain < 0.1 on rotatory chair and a phase lead > 68°. Exclusion criteria comprised being unable to stop vestibular suppressants for 1 week (cinnarizine and all psychiatric medication), and the inability to undergo one of the vestibular examinations.
Testing protocol
Experimental setup [7]
One trained examiner (FL) performed all VHIT’s. A fixed distance of two metres from the back of the chair to the point of fixation was ensured [10]. Patients were seated on a static chair, to prevent upper body movement during head impulses. The room was well lit, to ensure a small pupil in every patient. Patients fixated on a green (532-nm) 1-mw laser dot projected on a large full visual field black (or white) painted wall. This facilitated a wider range for measuring the eye movements. At the same time, it minimised the change of artefacts due to light reflections onto the pupil. The fixating point was adjusted to the eye level of every patient. Each test started with calibration of the system. The examiner assessed the quality of the calibration and determined whether the process needed to be repeated. The examiner stood behind the patient, holding the head firmly during head impulses. Patients were instructed to relax their neck, keep their eyes wide open and fixate on the target in front of them. The examiner continuously repeated these instructions to facilitate optimal awareness of the patient. The head impulses comprised fast horizontal rotational head movements (> 120°/s) with a low amplitude, unpredictable in timing and direction. Only outward impulses were given [11].
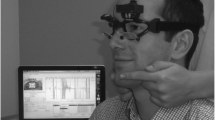
The camera of the Interacoustics and Otometrics systems is head fixed and is integrated in a pair of goggles. Therefore, before start of testing, goggle movement was minimised by tightly fastening the strap of the goggles around the patients’ head. The camera was always set on the right eye and focused on the pupil while the patient looked at the point of fixation with eyes wide open. In case the eyelids were in front of the pupil, the examiner adjusted the rim of the goggles so they would hold the eyelids back. After calibration, the patient was instructed to not touch (the strap of) the goggles, their face and/or their hair. The camera of the Synapsys system is space fixed, and therefore, no goggles were used. The camera that measured eye and head movements was placed in front of the patient. Eye movements from both eyes were measured (Fig. 1).
VHIT systems
Three different VHIT systems were used in this study: EyeSeeCam (Interacoustics VOG; Munich, Germany), ICS Impulse (GN Otometrics; Taastrup, Denmark), and Ulmer (Synapsys, Marseille, France). Each patient sequentially underwent the horizontal VHIT with the different VHIT systems. The Synapsys system was not used in 17 patients, and the Interacoustics system was not used in one patient, due to the unavailability of the systems at the time of testing. The order of testing of the different VHIT systems was randomised by draw.
VOR gain calculation by the different VHIT systems
VOR gain, as calculated by the systems, was used as main outcome parameter. The three systems calculate VOR gain differently. Interacoustics uses instantaneous gain; it divides eye- and head velocity at a certain point in time (small window around 60 ms) after onset of the head movement [12]. Otometrics calculates VOR gain as the ratio of the area under the eye velocity and head velocity curve (from 60 ms before peak head acceleration to the last value of 0°/s as the head returns to rest). If needed, the eye movement is desaccaded by the system before the VOR gain is calculated [13]. The Synapsys system calculates the VOR gain over the period from 40 ms before to 80 ms after peak head acceleration for each impulse. In case of a covert saccade, the 80-ms window is reduced, and stops at time of onset of the covert saccade [14]. However, the method of gain calculation used by the Synapsys system was unknown to this research group, despite multiple efforts to obtain more information from the manufacturer.
Covert saccades
Covert saccades might influence VOR gain (calculation). Therefore, covert saccades in this study population were analysed separately to assess whether they differed between tests (as an adaptation effect) in this BV population when repeatedly tested. The frequency of occurrence of covert saccades, and the latency of the first covert saccade of a trace were analysed.
Extracting data
To extract saccades, head and eye velocity (Interacoustics and Otometrics) and position (Synapsys) traces were exported and processed using Wolfram Mathematica 11.3 (Wolfram Research, Champaign, IL, USA). Only traces that were accepted by the systems were exported.
Pre-processing data
Synapsys measures both eyes during VHIT, but in this study, it was chosen to only use traces from the right eye, to better facilitate comparison with Interacoustics and Otometrics, which only register data from the right eye. In case of missing values from the right eye, data from the left eye were used. Because of the lower resolution of the Synapsys camera (100 Hz), the original eye and head position data were resampled to 250 Hz using linear interpolation. By differentiating these eye and head position traces, the velocity traces were calculated for eye and head movements recorded with the Synapsys system. Eye and head velocity traces from Interacoustics and Otometrics were directly extracted from the system itself. Eye and head position data for these two systems were calculated using numerical integration. Head and eye acceleration data were calculated for all three systems by differentiating the eye and head velocity signal.
Cleaning data
To establish artefact-free traces for analysis, traces were removed when (1) peak head velocity was < 120°/s, or (2) the head velocity trace contained a bounce at the end of the impulse of > 50% of peak head velocity, or (3) head velocity never crossed zero after peak head velocity (within the recorded time frame), or (4) the head velocity trace contained missing values, or (5) the shape of the head velocity trace implied an inadequate head impulse, assessed by visual inspection and consensus between three authors (RB, DS, TD), or (6) when the mean head velocity of the interval of 80 ms prior and 120 ms after a peak head velocity was not in the range of ± 3 SD of the set of mean head velocities calculated in the same interval in all traces of one patient [4, 15, 16].
Saccade detection
A custom-made algorithm was developed in Mathematica, and applied to extract saccades from the eye traces. To increase accuracy, every saccade was verified by visual inspection in the eye and head velocity and position traces. Two authors needed to achieve consensus (TD, DS) before a saccade was approved. Head impulse onset was specified as head velocity exceeding 10°/s, head impulse offset was defined as head velocity crossing 0°/s. Onset of a saccade was marked as the point where eye velocity crossed 0°/s or eye acceleration reached 2000°/s2. Saccades were included when (1) they occurred after peak head velocity, and (2) had a magnitude of more than 60°/s, and (3) peak velocity of the saccade was recorded, and (4) occurred at least in two traces around the same location within the same trial and patient. A saccade was classified as covert when onset occurred before head velocity crossed zero, and as overt when onset occurred after head velocity crossed zero.
Saccade analysis: defining frequency and latency
In this study, the first covert saccades of the first seven artefact-free traces were used for analysis [17]. The frequency and latency of the covert saccades were extracted from the original eye velocities in the Interacoustics and Otometrics system, and from the calculated eye velocities in the Synapsys system. The frequency of occurrence of a covert saccade was first registered as a binary outcome (Yes/No) for every trace separately. From these data, a ratio per patient was calculated (in percentage). Latency (in milliseconds) was registered as the onset of the covert saccade, and was normalised to the start of the head impulse [18].
Statistical analysis
Data were analysed using SPSS Statistics 24 for Windows and R (v.3.5.2.). The α-value was set on p < 0.05. In case of multiple comparisons, the Bonferroni correction was applied. When no interaction was found between leftwards and rightwards head impulses, the direction of the impulse was removed from the statistical model and both sides were analysed together.
Statistical analysis of VOR gain and agreement of VHIT systems regarding BV diagnosis
A repeated-measures ANOVA was used to compare mean VOR gain between the three systems. A VOR gain of < 0.6 was classified as “bilateral vestibulopathy”, a VOR gain of ≥ 0.6 was classified as “no bilateral vestibulopathy” [8]. In case the VHIT systems showed a discrepancy in classifying BV, it was classified as “no agreement”.
Statistical analysis of VOR gain and repetitive testing (the order effect)
To evaluate the order effect, a repeated-measures ANOVA was used to compare mean VOR gain between the first and the last executed VHIT trial (regardless of the VHIT system).
Statistical analysis of peak head velocity
Peak head velocities (extracted from the raw traces of the VHIT systems) of all traces of all patients were combined per VHIT system. Median peak head velocities were compared between VHIT systems using a Mann–Whitney U test. In patients with “no agreement” between systems, peak head velocities were analysed separately within the BV patient. Median peak head velocities of those particular trials were compared between VHIT systems using a Mann–Whitney U test.
Statistical analysis of saccades
The frequency of occurrence of covert saccades was compared between the first and the last executed VHIT trial (regardless of the VHIT system) using a generalised linear mixed-effects model. Additionally, the latency of the first covert saccade was compared between the first and the last executed VHIT trial (regardless of the VHIT system) with a paired T test. Patients with missing values (no saccades) were not included in this last analysis.
Results
Patient characteristics
In total, 46 BV patients were included: 23 males and 23 females. Mean age was 59 years (standard deviation 11 years). Definite and probable etiologies comprised: ototoxic effects of antibiotics (n = 8) or chemotherapy (n = 1), post-infectious due to Lyme disease (n = 1), Hashimoto’s thyroiditis (n = 1), Herpes infection (n = 1), meningitis (n = 2), inherited, e.g. by DFNA9 gene mutation (n = 7), bilateral Menière’s disease (n = 3), autoimmune disease (n = 1). In 21 patients, no etiology could be determined (idiopathic).
All three VHIT systems were able to capture the same type of eye movement responses to head impulses. This is illustrated in Fig. 2, which presents the raw data of one BV patient (patient 21), selected as a representative sample of the whole study population. Further details of VHIT characteristics (VOR gain, peak head velocity, timing of saccades) of all tested patients will be discussed below.
Raw eye and head movement data of one BV patient (patient 21), obtained by three different VHIT systems during three consecutive VHIT trials. Grey dotted lines represent eye movements, orange lines represent head movements, red lines represent saccades. Note that eye movements obtained with the Synapsys system have a different graphical representation. This is based on the fact that a space-fixed camera with a lower sampling rate was used, instead of a head-fixed camera
VOR gain and agreement of VHIT systems regarding BV diagnosis
Figure 3 illustrates that different VOR gains were obtained by different VHIT systems, within the same BV patients. There was a statistically significant difference between the three systems in VOR gains [F(1.256, 33.916) = 35.681, p < 0.000]. VOR gains obtained with the Synapsys system differed significantly from VOR gains obtained with the other two systems. No statistically significant difference was found in VOR gains between the Interacoustics and Otometrics system. Mean VOR gains of all patients were 0.33, 0.35 and 0.10 for Interacoustics, Otometrics and Synapsys system, respectively.
VOR gains for leftwards and rightwards horizontal VHIT, as tested with three different VHIT systems. Every symbol represents the VOR gain of one VHIT trial in one patient obtained with one VHIT system. The horizontal line at a VOR gain of 0.6 represents the cut-off value according to the BV criteria of the Bárány society [8]. VOR gains obtained with the Synapsys system differed significantly from VOR gains obtained with the other two systems. No statistically significant difference was found in VOR gains between the Interacoustics and Otometrics system
The VHIT systems agreed in 83% of the 46 patients on the BV diagnosis (“bilateral vestibulopathy” or “no bilateral vestibulopathy”) according to the criteria of the Bárány Society [8]. In eight patients (17%), no agreement was found (Table 1). These eight patients were diagnosed with BV resulting from various etiologies: ototoxic effects of gentamicin (n = 1) and chemotherapy (n = 1), bilateral Menière’s disease (n = 1), post-infectious due to Lyme’s disease, (n = 1) inherited (n = 1), and idiopathic (n = 3).
In the 28 patients tested with all three VHIT systems, the percentage of agreement between the VHIT systems was 79% (68% BV, 11% no BV), and in 21% there was no agreement. The mean VOR gains obtained in these 28 patients were 0.36, 0.36 and 0.09 for Interacoustics, Otometrics and Synapsys respectively.
VOR gain and repetitive testing
No order effect was present, since no difference in VOR gain was found between the first and the last VHIT trials, regardless of the system used for VHIT.
Peak head velocity
For every VHIT system, median peak head velocities with their interquartile range of all traces together from all patients are presented in Table 2. A significant difference in the velocity of the head impulses between the three systems was found (p < 0.001). Regarding the Synapsys system, significantly lower median peak head velocities (maximum 43°/s lower) and VOR gains (maximum 0.37 lower) were present than in the other two systems. Interacoustics and Otometrics did not significantly differ regarding VOR gain, only regarding median peak head velocity (maximum 11°/s).
Peak head velocities were separately analysed in the eight patients with “no agreement” on the diagnosis of BV according to the VHIT systems (Fig. 3). In one out of the eight patients, the median peak head velocity of the given head impulses was significantly higher in the system with the lower VOR gain. This patient showed in the Interacoustics system a VOR gain of 0.74 with median peak head velocity of 196°/s (leftwards impulses) and a VOR gain of 0.73 with median peak head velocity of 214°/s (rightwards impulses), versus a VOR gain of 0.57 with median peak head velocity of 265°/s (leftwards impulses) and a VOR gain of 0.58 with median peak head velocity of 255°/s (rightwards impulses) in the Otometrics system.
In the other seven patients, no statistically significant difference in peak head velocities between VHIT systems was found, or the system with significantly higher (or lower) peak head velocities also measured higher (or lower, respectively) VOR gains in that patient [19].
Frequency and latency of covert saccades
According to the strict methods as described above, frequency of covert saccades could be analysed in 34 patients, and latency of covert saccades in 20 patients. In this study, no statistically significant difference in the frequency of occurrence of covert saccades and in the latency of the first appearing covert saccade was found between the first and the last VHIT trials, regardless of the system (Fig. 4).
Characteristics of the first appearing covert saccade from the first seven artefact-free traces of all patients together. a The frequency of covert saccades (percentage of impulses with at least one covert saccade) in the first and last VHIT trial. b Latency of the first covert saccade (the moment of onset of the saccade in milliseconds, start of head impulse is 0 ms) in the first and last VHIT trials. No statistically significant difference was found within the characteristics between the first and the last VHIT trials regardless of the VHIT system (Interacoustics, Otometrics or Synapsys)
Discussion
This study compared the VOR gains obtained with three commercially available VHIT systems (Interacoustics, Otometrics and Synapsys) in a large group of BV patients. In 83% of the patients the VHIT systems agreed on the diagnoses of BV, when using a cut-off horizontal VOR gain of < 0.6 [8]. Additionally, while VOR gains did not significantly differ between the Interacoustics and Otometrics system, they both significantly differed from VOR gains obtained with the Synapsys system.
The fact that agreement between VHIT systems on BV diagnosis was present in 83% of the cases implies that in 17%, no agreement was present. This is suboptimal for diagnostic devices used in clinical setting. It would be preferred to further investigate the origin of these differences in outcome between VHIT systems, to improve the diagnostic pathway in BV patients. The origin might have (partially) resulted from inherent differences in the VHIT systems themselves, e.g. differences in eye and head tracking, and/or VOR gain calculation. This has been described before in healthy subjects, but this is the first study that shows the possible significant impact on the diagnosis of BV [5, 6]. It has been hypothesised that mainly the differences in VOR gain calculation algorithm are responsible for the VOR gain differences (van der Lans, manuscript in preparation). After all, especially in BV patients, the transfer function of the VOR is often not linear, and the appearance of covert saccades might interfere with VOR gain calculation. This implies that VOR gain outcomes are very sensitive to pre-processing (e.g. desaccading) and interpretation of the traces by the VOR gain calculation algorithm. To overcome some of these challenges, the Suppression Head Impulse Test (SHIMP) was proposed, that might decrease the amount of covert saccades and better show the residual vestibular function [3, 13, 20]. However, this paradigm still depends on the VOR gain calculation algorithm, and its clinical relevance in BV is yet to be determined (van Dooren, manuscript in preparation). Generally, it seems therefore necessary that VHIT systems are standardised regarding eye and head tracking methods and VOR gain calculation algorithms, to improve proper diagnosis of BV. If this is not possible, it could be investigated whether VHIT system-specific cut-off values to diagnose BV are a possibility to increase agreement between VHIT systems. Nevertheless, it remains important to not only assess VOR gain, but also the raw traces and compensatory saccades. In addition, BV is diagnosed using a combination of symptoms and several vestibular tests (caloric test, rotatory chair test, VHIT). Since these vestibular tests are complementary, only performing VHIT might not be enough to rule out BV [8, 21].
In this BV population, outcomes of the Synapsys system differed significantly from the other two VHIT systems: Synapsys showed a lower VOR gain than Interacoustics and Otometrics (Fig. 3). This could (partially) be explained by differences in gain calculation algorithms, different eye- and head tracking methods (Synapsys uses a space-fixed camera, the other two systems use a camera fixed to a pair of goggles), or differences in sampling frequency (Synapsys uses a lower sampling frequency of 100 Hz, compared to 220 Hz and 245 Hz for Interacoustics and Otometrics, respectively). Furthermore, during visual inspection the Synapsys system showed less smooth eye velocity traces, and more missing values than Interacoustics and Otometrics (Fig. 2). However, when the Synapsys system considered a patient “no BV” (VOR gain ≥ 0.6), this was always in agreement with both of the other two systems. Nevertheless, the other way around (“BV” with Synapsys and “no BV” in the other two systems) also occurred. It is unknown whether this was a systematic mistake of the Synapsys system, or whether Synapsys was the only system that was able to best detect BV in the high-frequency range of this population. This question was beyond the scope of this article, but could be addressed in the future.
When observing differences in VOR gains between different VHIT systems and VHIT trials, it is very important to first rule out measurement artefacts, like clinically relevant differences in peak head velocities, the order effect, and differences in frequency and latency of covert saccades that could influence the VOR gain calculations [5, 16, 21]. Regarding differences in peak head velocities, a higher peak head velocity might result in lower VOR [19]. However, in contrast to these findings, the system with significantly lower median peak head velocities during VHIT trials (Synapsys), also showed the lowest VOR gains in this study. Therefore, it is very unlikely that differences in peak head velocity between Synapsys and the other VHIT systems might have caused most of the VOR gain differences between VHIT systems in this study. The statistically significant difference in median peak head velocities between VHIT trials of Interacoustics and Otometrics was only small (11°/s difference), and, therefore, probably not influenced the (not significant) VOR gain differences between the two systems [19]. Regarding the order effect and the frequency and latency of covert saccades, VOR gains and covert saccades did not show differences in this BV population with repetitive testing. This is in agreement with previous studies on healthy subjects and patients with vestibular dysfunction [7, 22]. Therefore, it can be concluded that it is very unlikely that measurement artefacts like the order effect or covert saccades could explain the significant differences in VOR gains found between the three VHIT systems in this study.
Limitations
In patients with low VOR gains, biphasic eye movement artefacts can occur at the beginning of head impulses, when using a head-mounted VHIT system (e.g. Fig. 2, eye movements obtained during rightward impulses with Interacoustics and Otometrics system). This might lead to erroneous higher VOR gains, especially when using the instantaneous gain calculation method (Interacoustics) compared to the area under the curve gain calculation method (Otometrics) [13, 16]. This type of artefact was not specifically addressed in this study. Since VOR gains obtained with the Interacoustics and Otometrics systems did not significantly differ in this study, comparison of these two systems was most likely not compromised by this artefact. However, it cannot be ruled out that this artefact might (partially) explain some of the relatively lower VOR gains in the Synapsys system.
Conclusion
To conclude, using different VHIT systems in the same BV patient can lead to clinically significant differences in VOR gain, when using a cut-off value of 0.6. This might hinder proper diagnosis of BV patients. It would, therefore, be preferred that VHIT systems are standardised regarding eye and head tracking methods, and VOR gain calculation algorithms. Until then, it is advised to not only take the VOR gain in consideration when assessing a VHIT trial, but also look at the raw traces and the compensatory saccades.
Availability of data and material
The data that support the findings of this study are available from the corresponding author, TD, upon reasonable request.
References
Lucieer F et al (2018) Full spectrum of reported symptoms of bilateral vestibulopathy needs further investigation—a systematic review. Front Neurol 9:352
Lucieer F et al (2016) Bilateral vestibular hypofunction: insights in etiologies, clinical subtypes, and diagnostics. Front Neurol 7:26
Halmagyi GM et al (2017) The video head impulse test. Front Neurol 8:258
Cleworth TW et al (2017) Differences in head impulse test results due to analysis techniques. J Vestib Res 27(2–3):163–172
Janky KL et al (2017) Effects of device on video head impulse test (vHIT) gain. J Am Acad Audiol 28(9):778–785
Lee SH et al (2018) Comparison of video head impulse test (vHIT) gains between two commercially available devices and by different gain analytical methods. Otol Neurotol 39(5):e297–e300
van Dooren TS et al (2018) The video head impulse test and the influence of daily use of spectacles to correct a refractive error. Front Neurol 9:125
Strupp M et al (2017) Bilateral vestibulopathy: diagnostic criteria consensus document of the classification committee of the Barany society. J Vestib Res 27(4):177–189
Mantokoudis G et al (2016) Adaptation and compensation of vestibular responses following superior canal dehiscence surgery. Otol Neurotol 37(9):1399–1405
Castro P et al (2018) Viewing target distance influences the vestibulo-ocular reflex gain when assessed using the video head impulse test. Audiol Neurootol 23(5):285–289
Park JW et al (2019) Differences in video head impulse test gains from right versus left or outward versus inward head impulses. Laryngoscope 129(7):1675–1679. https://doi.org/10.1002/lary.27607
Interacoustics, EyeSeeCam vHIT system Manual (2014)
Macdougall HG et al (2013) The video Head Impulse Test (vHIT) detects vertical semicircular canal dysfunction. PLoS One 8(4):e61488
Wiener-Vacher SR, Wiener SI (2017) Video head impulse tests with a remote camera system: normative values of semicircular canal vestibulo-ocular reflex gain in infants and children. Front Neurol 8:434
Xie Y et al (2017) Compensatory saccades are associated with physical performance in older adults: data from the baltimore longitudinal study of aging. Otol Neurotol 38(3):373–378
Mantokoudis G et al (2015) Quantifying the vestibulo-ocular reflex with video-oculography: nature and frequency of artifacts. Audiol Neurootol 20(1):39–50
Wenzel A et al (2019) Reducing the number of impulses in video head impulse testing—it’s the quality not the numbers. Int J Pediatr Otorhinolaryngol 125:206–211
Rey-Martinez J et al (2017) The role of predictability in saccadic eye responses in the suppression head impulse test of horizontal semicircular canal function. Front Neurol 8:536
Kim TS et al (2018) Changes of video head impulse test results in lateral semicircular canal plane by different peak head velocities in patients with vestibular neuritis. Acta Otolaryngol 138(9):785–789
MacDougall HG et al (2016) A new saccadic indicator of peripheral vestibular function based on the video head impulse test. Neurology 87(4):410–418
van de Berg R, van Tilburg M, Kingma H (2015) Bilateral vestibular hypofunction: challenges in establishing the diagnosis in adults. ORL J Otorhinolaryngol Relat Spec 77(4):197–218
Singh NK, Govindaswamy R, Jagadish N (2019) Test-retest reliability of video head impulse test in healthy individuals and individuals with dizziness. J Am Acad Audiol 30(9):744–752. https://doi.org/10.3766/jaaa.17080
Funding
HK, RB and DS were supported by the Tomsk State University competitiveness improvement programme.
Author information
Authors and Affiliations
Contributions
Design of the work: HK, RB. Acquisition: FL. Analysis: TD, DS, BV, AJ. Interpretation: TD, NG, AP, VV, HK, RB. Revising the work: TD, DS, FL, AJ, NG, AP, VV, HK, RB. Final approval of the version to be published: TD, DS, FL, BV, AJ, NG, AP, VV, HK, RB. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: TD, DS, FL, BV, AJ, NG, AP, VV, HK, RB.
Corresponding author
Ethics declarations
Conflicts of interest
No conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Dooren, T.S., Starkov, D., Lucieer, F.M.P. et al. Comparison of three video head impulse test systems for the diagnosis of bilateral vestibulopathy. J Neurol 267 (Suppl 1), 256–264 (2020). https://doi.org/10.1007/s00415-020-10060-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-10060-w