Abstract
Purpose
Preeclampsia is a major cause of health problems for both pregnant women and unborn babies worldwide. However, the underlying causes of preeclampsia are not fully understood, leading to limited effective treatments. The goal of this study is to enhance our knowledge of its causes, devise prevention strategies, and develop treatments.
Methods
We performed a systematic literature search. Six models regarding the pathogenesis of preeclampsia are discussed in this review.
Results
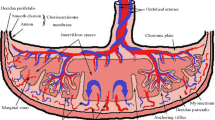
This review focuses on the latest advancements in understanding preeclampsia’s origins. Preeclampsia is a complex condition caused by various factors, processes, and pathways. Reduced blood flow and oxygen to the uterus and placenta, heightened inflammatory reactions, immune imbalances, altered genetic changes, imbalanced blood vessel growth factors, and disrupted gut bacteria may contribute to its development.
Conclusion
Preeclampsia is thought to result from the interplay of these factors.

Similar content being viewed by others
References
Chen Y, Lin M, Guo P, Xiao J, Huang X, Xu L, Xiong N, O’Gara MC, O’Meara M, Tan X (2021) Uterine fibroids increase the risk of hypertensive disorders of pregnancy: a prospective cohort study. J Hypertens 39(5):1002–1008. https://doi.org/10.1097/hjh.0000000000002729
Mistry HD, Kurlak LO, Gardner DS, Torffvit O, Hansen A, Broughton Pipkin F, Strevens H (2019) Evidence of augmented intrarenal angiotensinogen associated with glomerular swelling in gestational hypertension and preeclampsia: clinical implications. J Am Heart Assoc 8(13):e012611. https://doi.org/10.1161/jaha.119.012611
von Dadelszen P, Bhutta ZA, Sharma S, Bone J, Singer J, Wong H, Bellad MB, Goudar SS, Lee T, Li J, Mallapur AA, Munguambe K, Payne BA, Qureshi RN, Sacoor C, Sevene E, Vidler M, Magee LA (2020) The community-level interventions for pre-eclampsia (CLIP) cluster randomised trials in Mozambique, Pakistan, and India: an individual participant-level meta-analysis. Lancet 396(10250):553–563. https://doi.org/10.1016/s0140-6736(20)31128-4
Turbeville HR, Taylor EB, Garrett MR, Didion SP, Ryan MJ, Sasser JM (2019) Superimposed preeclampsia exacerbates postpartum renal injury despite lack of long-term blood pressure difference in the dahl salt-sensitive rat. Hypertension 73(3):650–658. https://doi.org/10.1161/hypertensionaha.118.12097
Yang F, Janszky I, Gissler M, Roos N, Wikström AK, Yu Y, Chen H, Bonamy AE, Li J, László KD (2022) Association of Maternal Preeclampsia With Offspring Risks of Ischemic Heart Disease and Stroke in Nordic Countries. JAMA Netw Open 5(11):e2242064. https://doi.org/10.1001/jamanetworkopen.2022.42064
Torbergsen T, Oian P, Mathiesen E, Borud O (1989) Pre-eclampsia—a mitochondrial disease? Acta Obstet Gynecol Scand 68(2):145–148. https://doi.org/10.3109/00016348909009902
Marín R, Chiarello DI, Abad C, Rojas D, Toledo F, Sobrevia L (2020) Oxidative stress and mitochondrial dysfunction in early-onset and late-onset preeclampsia. Biochim Biophys Acta Mol Basis Dis 1866(12):165961. https://doi.org/10.1016/j.bbadis.2020.165961
Roca-Portoles A, Tait SWG (2021) Mitochondrial quality control: from molecule to organelle. Cell Mol Life Sci 78(8):3853–3866. https://doi.org/10.1007/s00018-021-03775-0
Eisner V, Picard M, Hajnóczky G (2018) Mitochondrial dynamics in adaptive and maladaptive cellular stress responses. Nat Cell Biol 20(7):755–765. https://doi.org/10.1038/s41556-018-0133-0
Wang Y, Xu E, Musich PR, Lin F (2019) Mitochondrial dysfunction in neurodegenerative diseases and the potential countermeasure. CNS Neurosci Ther 25(7):816–824. https://doi.org/10.1111/cns.13116
Hu XQ, Zhang L (2022) Mitochondrial Dysfunction in the Pathogenesis of Preeclampsia. Curr Hypertens Rep 24(6):157–172
Deer E, Herrock O, Campbell N, Cornelius D, Fitzgerald S, Amaral LM, LaMarca B (2023) The role of immune cells and mediators in preeclampsia. Nat Rev Nephrol. https://doi.org/10.1038/s41581-022-00670-0
Tanwar S, Rhodes F, Srivastava A, Trembling PM, Rosenberg WM (2020) Inflammation and fibrosis in chronic liver diseases including non-alcoholic fatty liver disease and hepatitis C. World J Gastroenterol 26(2):109–133. https://doi.org/10.3748/wjg.v26.i2.109
Du M, Wang W, Huang L, Guan X, Lin W, Yao J, Li L (2022) Natural killer cells in the pathogenesis of preeclampsia: a double-edged sword. Journal of Maternal-Fetal & Neonatal Medicine 35(6):1028–1035
Peraçoli JC, Fortes MR, Rudge MV, Rezkallah-Iwasso MT, Peraçoli MT (1995) Studies of natural killer cells in pregnancy-induced hypertension. Braz J Med Biol Res 28(6):655–661
Borzychowski AM, Croy BA, Chan WL, Redman CW, Sargent IL (2005) Changes in systemic type 1 and type 2 immunity in normal pregnancy and pre-eclampsia may be mediated by natural killer cells. Eur J Immunol 35(10):3054–3063. https://doi.org/10.1002/eji.200425929
Zhang Z, Gong F, Jia L, Chang C, Hou L, Yang R, Zheng F (2004) Studies on activity of NK cells in preeclampsia patients. J Huazhong Univ Sci Technolog Med Sci 24(5):473–475. https://doi.org/10.1007/bf02831112
Bachmayer N, Rafik Hamad R, Liszka L, Bremme K, Sverremark-Ekström E (2006) Aberrant uterine natural killer (NK)-cell expression and altered placental and serum levels of the NK-cell promoting cytokine interleukin-12 in pre-eclampsia. Am J Reprod Immunol 56(5–6):292–301. https://doi.org/10.1111/j.1600-0897.2006.00429.x
Kalkunte S, Chichester CO, Gotsch F, Sentman CL, Romero R, Sharma S (2008) Evolution of non-cytotoxic uterine natural killer cells. Am J Reprod Immunol 59(5):425–432. https://doi.org/10.1111/j.1600-0897.2008.00595.x
Raghupathy R (2013) Cytokines as key players in the pathophysiology of preeclampsia. Med Princ Pract 22(Suppl 1):8–19. https://doi.org/10.1159/000354200
Derzsy Z, Prohászka Z, Rigó J Jr, Füst G, Molvarec A (2010) Activation of the complement system in normal pregnancy and preeclampsia. Mol Immunol 47(7–8):1500–1506. https://doi.org/10.1016/j.molimm.2010.01.021
Robertson SA, Green ES, Care AS, Moldenhauer LM, Prins JR, Hull ML, Barry SC, Dekker G (2019) Therapeutic Potential of Regulatory T Cells in Preeclampsia-Opportunities and Challenges. Front Immunol 10:478. https://doi.org/10.3389/fimmu.2019.00478
Tsuda S, Nakashima A, Shima T, Saito S (2019) New Paradigm in the Role of Regulatory T Cells During Pregnancy. Front Immunol 10:573. https://doi.org/10.3389/fimmu.2019.00573
Hu M, Eviston D, Hsu P, Mariño E, Chidgey A, Santner-Nanan B, Wong K, Richards JL, Yap YA, Collier F, Quinton A, Joung S, Peek M, Benzie R, Macia L, Wilson D, Ponsonby AL, Tang MLK, O’Hely M, Daly NL, Mackay CR, Dahlstrom JE, Vuillermin P, Nanan R (2019) Decreased maternal serum acetate and impaired fetal thymic and regulatory T cell development in preeclampsia. Nat Commun 10(1):3031
Docheva N, Arenas G, Nieman KM, Lopes-Perdigao J, Yeo KJ, Rana S (2022) Angiogenic Biomarkers for Risk Stratification in Women with Preeclampsia. Clin Chem 68(6):771–781
Li L, Yang H, Chen P, Xin T, Zhou Q, Wei D, Zhang Y, Wang S (2020) Trophoblast-Targeted Nanomedicine Modulates Placental sFLT1 for Preeclampsia Treatment. Front Bioeng Biotechnol 8:64. https://doi.org/10.3389/fbioe.2020.00064
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, Libermann TA, Morgan JP, Sellke FW, Stillman IE, Epstein FH, Sukhatme VP, Karumanchi SA (2003) Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Investig 111(5):649–658
Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, Schisterman EF, Thadhani R, Sachs BP, Epstein FH, Sibai BM, Sukhatme VP, Karumanchi SA (2004) Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 350(7):672–683
Phipps EA, Thadhani R, Benzing T, Karumanchi SA (2019) Pre-eclampsia: pathogenesis, novel diagnostics and therapies. Nat Rev Nephrol 15(5):275–289. https://doi.org/10.1038/s41581-019-0119-6
Gilbert JS, Verzwyvelt J, Colson D, Arany M, Karumanchi SA, Granger JP (2010) Recombinant vascular endothelial growth factor 121 infusion lowers blood pressure and improves renal function in rats with placentalischemia-induced hypertension. Hypertension 55(2):380–385
Narayan V, Thompson EW, Demissei B, Ho JE, Januzzi JL Jr, Ky B (2020) Mechanistic biomarkers informative of both cancer and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol 75(21):2726–2737. https://doi.org/10.1016/j.jacc.2020.03.067
Tian J, Xie B, Xiang L, Zhao Y, Zhou D (2016) Soluble Flt-1 improves the repair of ankle joint injury in rats. Am J Transl Res 8(11):4942–4950
Lecarpentier E, Zsengellér ZK, Salahuddin S, Covarrubias AE, Lo A, Haddad B, Thadhani RI, Karumanchi SA (2020) Total versus free placental growth factor levels in the pathogenesis of preeclampsia. Hypertension 76(3):875–883
Tsatsaris V, Goffin F, Munaut C, Brichant JF, Pignon MR, Noel A, Schaaps JP, Cabrol D, Frankenne F, Foidart JM (2003) Overexpression of the soluble vascular endothelial growth factor receptor in preeclamptic patients: pathophysiological consequences. J Clin Endocrinol Metab 88(11):5555–5563
Park S, Dimaio TA, Liu W, Wang S, Sorenson CM, Sheibani N (2013) Endoglin regulates the activation and quiescence of endothelium by participating in canonical and non-canonical TGF-β signaling pathways. J Cell Sci 126(Pt 6):1392–1405
Margioula-Siarkou G, Margioula-Siarkou C, Petousis S, Margaritis K, Vavoulidis E, Gullo G, Alexandratou M, Dinas K, Sotiriadis A, Mavromatidis G (2022) The role of endoglin and its soluble form in pathogenesis of preeclampsia. Mol Cell Biochem 477(2):479–491
Dymara-Konopka W, Laskowska M, Grywalska E, Hymos A, Błażewicz A, Leszczyńska-Gorzelak B (2023) Similar pro- and antiangiogenic profiles close to delivery in different clinical presentations of two pregnancy syndromes: preeclampsia and fetal growth restriction. IJMS 24(2):972
Margioula-Siarkou G, Margioula-Siarkou C, Petousis S, Margaritis K, Alexandratou M, Dinas K, Sotiriadis A, Mavromatidis G (2021) Soluble endoglin concentration in maternal blood as a diagnostic biomarker of preeclampsia: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol 258:366–381
Schmella MJ, Assibey-Mensah V, Parks WT, Roberts JM, Jeyabalan A, Hubel CA, Catov JM (2019) Plasma concentrations of soluble endoglin in the maternal circulation are associated with maternal vascular malperfusion lesions in the placenta of women with preeclampsia. Placenta 78:29–35
Xia Y, Kellems RE (2013) Angiotensin receptor agonistic autoantibodies and hypertension: preeclampsia and beyond. Circ Res 113(1):78–87
Zhou CC, Zhang Y, Irani RA, Zhang H, Mi T, Popek EJ, Hicks MJ, Ramin SM, Kellems RE, Xia Y (2008) Angiotensin receptor agonistic autoantibodies induce pre-eclampsia in pregnant mice. Nat Med 14(8):855–862
Duncan JW, Azubuike D, Booz GW, Fisher B, Williams JM, Fan F, Ibrahim T, LaMarca B, Cunningham MW (2020) Angiotensin II type 1 receptor autoantibody blockade improves cerebral blood flow autoregulation and hypertension in a preclinical model of preeclampsia. Hypertens Pregnancy 39(4):451–460
Booz GW, Kennedy D, Bowling M, Robinson T, Azubuike D, Fisher B, Brooks K, Chinthakuntla P, Hoang NH, Hosler JP, Cunningham MW (2021) Angiotensin II type 1 receptor agonistic autoantibody blockade improves postpartum hypertension and cardiac mitochondrial function in rat model of preeclampsia. Biol Sex Differ 12(1):58
Ling C, Rönn T (2019) Epigenetics in Human Obesity and Type 2 Diabetes. Cell Metab 29(5):1028–1044. https://doi.org/10.1016/j.cmet.2019.03.009
Moroney JB, Vasudev A, Pertsemlidis A, Zan H, Casali P (2020) Integrative transcriptome and chromatin landscape analysis reveals distinct epigenetic regulations in human memory B cells. Nat Commun 11(1):5435. https://doi.org/10.1038/s41467-020-19242-6
Ye Y, Tang Y, Xiong Y, Feng L, Li X (2019) Bisphenol A exposure alters placentation and causes preeclampsia-like features in pregnant mice involved in reprogramming of DNA methylation of WNT2. FASEB J 33(2):2732–2742. https://doi.org/10.1096/fj.201800934RRR
Serpeloni F, Radtke K, de Assis SG, Henning F, Nätt D, Elbert T (2017) Grandmaternal stress during pregnancy and DNA methylation of the third generation: an epigenome-wide association study. Transl Psychiatry 7(8):e1202. https://doi.org/10.1038/tp.2017.153
Yu MM, Feng YH, Zheng L, Zhang J, Luo GH (2019) Short hairpin RNA-mediated knockdown of nuclear factor erythroid 2-like 3 exhibits tumor-suppressing effects in hepatocellular carcinoma cells. World J Gastroentero 25(10):1210–1223
Cheng JX, Chen L, Li Y, Cloe A, Yue M, Wei J, Watanabe KA, Shammo JM, Anastasi J, Shen QJ, Larson RA, He C, Le Beau MM, Vardiman JW (2018) Author correction: RNA cytosine methylation and methyltransferases mediate chromatin organization and 5-azacytidine response and resistance in leukaemia. Nat Commun 9(1):2286
Andrawus M, Sharvit L, Atzmon G (2022) Epigenetics and pregnancy: conditional snapshot or rolling event. Int J Mol Sci 23(20):12698. https://doi.org/10.3390/ijms232012698
Hu XQ, Song R, Zhang L (2019) Effect of oxidative stress on the estrogen-NOS-NO-K(Ca) channel pathway in uteroplacental dysfunction: its implication in pregnancy complications. Oxid Med Cell Longev 2019:9194269. https://doi.org/10.1155/2019/9194269
Ma M, Zhou QJ, Xiong Y, Li B, Li XT (2018) Preeclampsia is associated with hypermethylation of IGF-1 promoter mediated by DNMT1. Am J Transl Res 10(1):16–39
Jia Y, Li T, Huang X, Xu X, Zhou X, Jia L, Zhu J, Xie D, Wang K, Zhou Q, Jin L, Zhang J, Duan T (2017) Dysregulated DNA methyltransferase 3A upregulates IGFBP5 to suppress trophoblast cell migration and invasion in preeclampsia. Hypertension 69(2):356–366
Kaur L, Sundrani D, Dave K, Randhir K, Mehendale S, Bayyana S, Kalyanaraman K, Chandak GR, Joshi S (2023) Hypoxia inducible factors (HIF1α and HIF3α) are differentially methylated in preeclampsia placentae and are associated with birth outcomes. Mol Cell Biochem 478(10):2309–2318
Sultana Z, Maiti K, Aitken J, Morris J, Dedman L, Smith R (2017) Oxidative stress, placental ageing-related pathologies and adverse pregnancy outcomes. Am J Reprod Immunol. https://doi.org/10.1111/aji.12653
Franci G, Sarno F, Nebbioso A, Altucci L (2017) Identification and characterization of PKF118-310 as a KDM4A inhibitor. Epigenetics 12(3):198–205. https://doi.org/10.1080/15592294.2016.1249089
Hou L, Wei Y, Lin Y, Wang X, Lai Y, Yin M, Chen Y, Guo X, Wu S, Zhu Y, Yuan J, Tariq M, Li N, Sun H, Wang H, Zhang X, Chen J, Bao X, Jauch R (2020) Concurrent binding to DNA and RNA facilitates the pluripotency reprogramming activity of Sox2. Nucleic Acids Res 48(7):3869–3887. https://doi.org/10.1093/nar/gkaa067
Kawamura A, Münzel M, Kojima T, Yapp C, Bhushan B, Goto Y, Tumber A, Katoh T, King ON, Passioura T, Walport LJ, Hatch SB, Madden S, Müller S, Brennan PE, Chowdhury R, Hopkinson RJ, Suga H, Schofield CJ (2017) Highly selective inhibition of histone demethylases by de novo macrocyclic peptides. Nat Commun 8:14773. https://doi.org/10.1038/ncomms14773
Alahari S, Post M, Rolfo A, Weksberg R, Caniggia I (2018) Compromised JMJD6 Histone Demethylase Activity Affects VHL Gene Repression in Preeclampsia. J Clin Endocrinol Metab 103(4):1545–1557. https://doi.org/10.1210/jc.2017-02197
Bonasio R, Tu S, Reinberg D (2010) Molecular signals of epigenetic states. Science 330(6004):612–616. https://doi.org/10.1126/science.1191078
Li WZ, Zou Y, Song ZY, Wei ZW, Chen G, Cai QL, Wang Z (2020) Long non-coding RNA SNHG5 affects the invasion and apoptosis of renal cell carcinoma by regulating the miR-363-3p-Twist1 interaction. Am J Transl Res 12(2):697–707
Jiang W, Qu Y, Yang Q, Ma X, Meng Q, Xu J, Liu X, Wang S (2019) D-lnc: a comprehensive database and analytical platform to dissect the modification of drugs on lncRNA expression. RNA Biol 16(11):1586–1591. https://doi.org/10.1080/15476286.2019.1649584
Chatuphonprasert W, Jarukamjorn K, Ellinger I (2018) Physiology and Pathophysiology of Steroid Biosynthesis, Transport and Metabolism in the Human Placenta. Front Pharmacol 9:1027. https://doi.org/10.3389/fphar.2018.01027
Sun N, Qin S, Zhang L, Liu S (2021) Roles of noncoding RNAs in preeclampsia. Reprod Biol Endocrinol 19(1):100. https://doi.org/10.1186/s12958-021-00783-4
Brkić J, Dunk C, O’Brien J, Fu G, Nadeem L, Wang YL, Rosman D, Salem M, Shynlova O, Yougbaré I, Ni H, Lye SJ, Peng C (2018) MicroRNA-218-5p Promotes Endovascular Trophoblast Differentiation and Spiral Artery Remodeling. Mol Ther 26(9):2189–2205
Jiang S, Chen Q, Liu H, Gao Y, Yang X, Ren Z, Gao Y, Xiao L, Zhong M, Yu Y, Yang X (2020) Preeclampsia-associated lncRNA INHBA-AS1 regulates the proliferation, invasion, and migration of placental trophoblast cells. Mol Ther Nucleic Acids 22:684–695
Zhu Q, Xia P, Zhou X, Li X, Guo W, Zhu B, Zheng X, Wang B, Yang D, Wang J (2019) Hepatitis B Virus Infection Alters Gut Microbiota Composition in Mice. Front Cell Infect Microbiol 9:377. https://doi.org/10.3389/fcimb.2019.00377
Jin J, Gao L, Zou X, Zhang Y, Zheng Z, Zhang X, Li J, Tian Z, Wang X, Gu J, Zhang C, Wu T, Wang Z, Zhang Q (2022) Gut Dysbiosis Promotes Preeclampsia by Regulating Macrophages and Trophoblasts. Circ Res 131(6):492–506. https://doi.org/10.1161/circresaha.122.320771
Maifeld A, Bartolomaeus H, Löber U, Avery EG, Steckhan N, Markó L, Wilck N, Hamad I, Šušnjar U, Mähler A, Hohmann C, Chen CY, Cramer H, Dobos G, Lesker TR, Strowig T, Dechend R, Bzdok D, Kleinewietfeld M, Michalsen A, Müller DN, Forslund SK (2021) Fasting alters the gut microbiome reducing blood pressure and body weight in metabolic syndrome patients. Nat Commun 12(1):1970. https://doi.org/10.1038/s41467-021-22097-0
Yao M, Xiao Y, Yang Z, Ge W, Liang F, Teng H, Gu Y, Yin J (2022) Identification of Biomarkers for Preeclampsia Based on Metabolomics. Clin Epidemiol 14:337–360. https://doi.org/10.2147/clep.S353019
Acknowledgements
We thank contributors for this review. We thank Prof. Hongsheng Gao discussed this article. We thank Qin Zhu, Wen Wen PHD, Xin Zhang MD, and Yujuan Yuan PHD helped us collect literature. We thank the teachers and classmates who helped us write this manuscript. We thank all the peer reviewers for their opinions and suggestions. We thank the Major Science and Technology Projects of Xinjiang Uygur Autonomous Region for invaluable project support.
Funding
This work was supported by the Major Science and Technology Projects of Xinjiang Uygur Autonomous Region [2022A03012-2].
Author information
Authors and Affiliations
Contributions
NL: Project development and Supervision; MY: Data collection and Manuscript writing; MW: Writing-Reviewing and Editing; All the authors reviewed the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interest to disclose.
Ethics approval
This is a review, no ethical approval is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, M., Wang, M. & Li, N. Advances in pathogenesis of preeclampsia. Arch Gynecol Obstet 309, 1815–1823 (2024). https://doi.org/10.1007/s00404-024-07393-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-024-07393-6