Abstract
Introduction
The treatment option for borderline hip dysplasia (BHD) includes hip arthroscopy and periacetabular osteotomy (PAO). To the present day the controversial discussion remains, which intervention to prefer. Literature reports supporting an educated choice are scare, based on small patient cohorts and do not address the variability of acetabular morphology. Consequently, we intended to report PAO outcomes, from patients diagnosed with BHD, dependent on acetabular morphology, in a large patient cohort and aimed to define risk factors for poor clinical results and patient satisfaction.
Materials and methods
A prospective monocentre study was conducted. Patients enrolled underwent PAO for symptomatic BHD (LCEA, 18°–25°). A total of 107 hips were included with 94 complete data sets were available for evaluation with a minimum follow-up of 1 year and a mean follow-up of 2.3 years. The mean age was 31 ± 8.2 years, and 81.3% were female. As the primary outcome measure, we utilized the modified Harris hip score (mHHS) with minimal clinically important change (MCID) of eight to define clinical failure. Results were compared after a comprehensive radiographic assessment distinguishing between lateral deficient vs. anterior/posterolateral deficient acetabular and stable vs. unstable hip joints.
Results
Overall, clinical success was achieved in 91.5% of patients and the mHHS improved significantly (52 vs. 84.7, p < 0.001). Eight hips failed to achieve the MCID and four had radiographic signs of overcorrection. Comparing variable joint morphologies, the rate of clinical success was higher in patients with an anterior/posterolateral deficient acetabular covarage compared to lateral deficient acetabular (95.2% vs. 90.4%). tThe highest rate of clinical failure was recorded in unstable hip joints (85.7% vs. 92.5% in stable hips).
Conclusions
This study demonstrates that PAO is an effective means to treat symptomatic BHD with variable acetabular morphologies, achieving a clinical success in 91.5% of all patients. To maintain a high level of safety and patient satisfaction technical accuracy appears crucial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Borderline hip dysplasia (BHD) is a complex orthopaedic condition that involves subtle structural abnormalities of the hip joint. BDH has a prevalence of around 20% in the general population [1]. It is characterized by anatomical variations falling between normal acetabular coverage and classic hip dysplasia (HD). This acetabular undercoverage lead to increased biomechanical strain on the adjacent joint and soft tissue structures, culminating in progressive joint damage [2, 3].
Historically, developmental hip dysplasia was primarily defined using the Lateral centre-edge angle (LCEA), described by Wiberg [4]. In recent years, however, three-dimensional radiographic analyses have illuminated the various forms of acetabular coverage in hip dysplasia [5,6,7]. Additionally, radiographic parameters have been described to further evaluate not only the lateral acetabular coverage but also to determine acetabular undercoverage in anterior and posterior regions [8, 9]. Additionally, the femoro-epiphyseal-acetabular roof (FEAR) index was introduced by Wyatt et al. as a radiographic sign of joint instability in borderline hip dysplasia showing excellent intra- and interobserver reliability [10].
Despite these achievements, consensus remains elusive for the optimal treatment of patients with BHD [11]. Current therapeutic approaches focus on hip arthroscopy or bony correction through periacetabular osteotomy (PAO). Both procedures have demonstrated favourable results [11]. While some reports on hip arthroscopy revealed higher failure rates in BHD patients, the short-term follow-up of the more invasive PAO demonstrates safety and low revision rates [12,13,14]. However, it needs to be emphasized that available outcome reports of PAO in BHD are mainly based on small study cohorts [15, 16]. Solely, Nepple et al. reported the outcome after PAO for BHD in a larger patient cohort of 186 hips. The study results showed advantageous effects in patients undergoing primary PAO, while hips previously treated hip arthroscopically showed inferior outcomes [17]. Similarly, it is evident the postoperative results after hip arthroscopy of patients suffering from BHD are influenced by various hip morphology [18, 19]. Therefore, PAO could represent the preferable treatment modality for BHD independent of the individual acetabular configuration because PAO enables the correction of the osseous acetabular deformity using a minimally invasive approach in line with fast patient rehabilitation [20, 21]. Detailed analysis of PAO outcomes across variable types of acetabular and hip joint configurations in BDH are essential to further improve patient care.
Consequently, we set out to comprehensively assess pre- and postoperative radiographs in a cohort of > 100 patients treated for symptomatic BHD (LCEA 18°–25°) with emphasis on patient-reported outcomes contingent on different hip morphologies at a minimum follow-up of 1 year. We hypothesized that a precise bony deformity correction by PAO uniformly leads to improved postoperative patient-reported outcomes across various joint morphologies. Due to the fact that PAO enables the three-dimensional acetabular correction, it outlines a promising approach to address a wide spectrum of acetabular conditions with the aim to enhance patient-reported outcomes.
Materials and methods
Study design
We initiated a prospective follow-up study of 107 hips in 104 patients who underwent PAO due to symptomatic BHD (LCEA 18°–25°). The patients were treated at a single orthopaedic centre between 2019 and 2022.
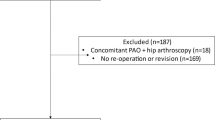
The patients presented with symptomatic and refractory hip pain lasting more than 6 months. BHD was diagnosed by a combination of patient reported symptoms, physical examination and radiographic parameters. Comprehensive radiographic diagnostic included X-rays of the anterior-posterior pelvis, as well as axial and oblique views of the affected hip joint. Indications for PAO were signs of osteoarthritis Tönnis grade < 2, a congruent hip joint, a history of therapy refractory hip pain in combination with radiographic signs of BHD. All patients gave written informed consent prior to study enrolment. Thirteen patients were excluded due to prior ipsilateral acetabular fracture (n = 1) and ipsilateral hip arthroscopy (n = 5) or the necessity of an additional femoral rotational osteotomy in the combination with the undergone PAO (n = 7) (Fig. 1).
Surgical technique
A modified, minimally invasive Bernese periacetabular osteotomy (PAO) technique was performed in all patients. This involved the use of a bikini incision and either a rectus-sparing (RS) approach (46/94) with bony detachment of the sartorius from its origin or a rectus- and sartorius-sparing (RASS) approach (48/94) as previously described by our group [22]. A mini-open arthrotomy was performed for a femoral head-neck osteochondroplasty in case of femoral asphericity right after PAO using the Smith-Peterson approach. All procedures were performed by the senior author (GIW). Physiotherapeutic training and mobilization of the operated hip joint started directly on the first postoperative day. In case of RASS approach, active hip flexion was permitted directly after surgery.
Complications and reoperations were assessed by consecutive patient follow-up. Implant removal was performed in 31 patients (34%) within the follow-up period and was not graded as intervention due to surgical complications.
Radiographic assessment
Radiographic assessment was performed by the first and senior authors. Preoperative and postoperative anterior-posterior pelvic X-rays were reviewed independently to analyse lateral centre-edge angle (LCEA). Further parameters included the, Tönnis osteoarthritis grade, medial centre-edge angle (MCEA), acetabular inclination (AI), anterior- and posterior wall index (AWI/PWI), signs of acetabular retroversion (crossover, posterior wall sign, sciatic spine sign), FEAR-index and Sourcil upsloping.
According to the radiographic assessment hip morphology was allocated to four distinct clusters—I.I lateral deficiency (LCEA 18°–25°, normal AWI/PWI) or I.II anterior/posterior—lateral deficiency (LCEA 18°–25°, low AWI/PWI) – II.I stable hip joint (LCEA 18°–25°, FEAR-index < 2°) or II.II unstable hip joint (LCEA 18°–25°, FEAR-index > 2°) (Fig. 2).
Data collection
Data was collected from electronic medical records, including patient demographics, preoperative comorbidities and operative details. The functional outcome after surgery was assessed by the modified Harris Hip Score (mHHS), International Hip Outcome Tool-12 (iHOT-12), University of California Los Angeles Activity scale (UCLA) and the Hip disability and Osteoarthritis Outcome Score (HOOS). In addition, the minimal clinically important difference (MCID) for the primary outcome measure, the mHHS, was analysed. A MCID of ≥ 8 was determined as a clinically meaningful change [23].
Statistical analysis
Descriptive statistics were used to summarize the patient characteristics and outcomes. Radiographic and patient reported outcome data were reported as mean with standard deviation. Statistical analysis and dataset presentation were performed using GraphPad Prism 9.4.1. A two-tailed paired t-test was used to compare pre- and postoperative patient-reported outcome and a two-tailed unpaired t-test was used to compare postoperative results between the groups. A p-value less than 0.05 was considered statistically significant.
Ethical considerations
All patients gave written informed consent prior to inclusion. Ethics approval (BB099/20) was obtained from the local independent ethics committee (IEC) of the University Medicine Greifswald according to the World Medical Association Declaration of Helsinki.
Results
Patient characteristics and preoperative radiographic parameters
A total of 107 hips in 104 patients were initially enrolled in this study. Thirteen patients did not fulfil the inclusion criteria due to prior ipsilateral acetabular fracture (n = 1), prior ipsilateral hip arthroscopy (n = 5) or the necessity of an additional femoral rotational osteotomy (n = 7) bringing the data set to a total of 94 hips in 91 patients. The mean age at the time of PAO was 31 ± 8.2 years, the mean BMI 24.7 ± 4.5. Seventeen patients (18.7%) were male, 74 (81.3%) were female. The mean follow-up was 2.3 ± 0.9 years.
The preoperative osteoarthritis assessment of the study cohort revealed 53 hips (56.4%) with Tönnis grade 0 and 41 hips (43.6%) with Tönnis grade 1. At the time of the surgical procedure, the mean LCEA was 20.4° ± 2.4° and the mean AI was 8.2° ± 4.4°. Acetabular retroversion was observed in 28.7% (27/94) of the included hips, based on the presence of all radiographic signs characteristics regarding acetabular retroversion (crossover sign, posterior wall sign, sciatic Spine sign) (Table 1).
Cluster I.I—lateral deficiency included 73 hips (77.7%) in 70 patients. The preoperative mean LCEA in this sub-group was 20.5 ± 2.3° with a mean AI of 7.8 ± 4.4°. The preoperative mean AWI was 45.6 ± 7.6% and the mean PWI equaled 89.1 ± 13.2% (Table 1).
Cluster I.II—anterior/posterior-lateral deficiency consisted of 21 hips (22.3%) in 21 patients. 14 hips exhibited a anterolateral deficient femoral head coverage and 7 hips showed a posterolateral acetabular deficiency. The preoperative mean LCEA in this subset was 20.0 ± 2.1° with a mean AI of 9.4 ± 4.2°. The preoperative mean AWI was 32.8 ± 12.3% and the mean PWI 84.1 ± 21.2%. In 28.6% (6/21 hips) all signs of acetabular retroversion were present (Table 1).
Cluster II.I—stable hip joint embraced 80 hips (85.1%) in 77 patients. The preoperative mean LCEA in this group measured 20.7 ± 2.5° with a mean AI of 7.7 ± 3.5°. The preoperative mean FEAR-index was –8.0 ± 5.7° (Table 1).
Cluster II.II—unstable hip joint showed 14 hips (14.9%) in 14 patients. The preoperative mean LCEA in this group was 18.7 ± 0.7° with a mean AI being 10.8 ± 3.1°. The preoperative mean FEAR-index was 6.4 ± 4.1° (Table 1).
Surgical procedure and postoperative radiographic parameters
In 51.1% (48/94 hips) a RS approach was performed and a RASS approach was used in 48.9% (46/94 hips) of all cases. A femoral head-neck osteochondroplasty in case of femoral asphericity was additionally performed in 79.8% (75/94 hips) (Table 2). The median number of screws used for osseous fixation was three.
Considering the entire study cohort, the mean LCEA has improved to 30.2° ± 3.9° and the mean AI hat improved to 0.1° ± 4° following the surgical procedure. No significant difference was observed between the defined subgroups (Table 2).
In patients with preoperative radiographic anterolateral/ posterolateral deficiency (cluster I.II), the AWI and PWI has improved postoperatively. Evaluating cluster II, an improvement in the FEAR Index, due to surgical correction, was observed in unstable hip joints (Table 2).
Patient-reported outcomes
At the latest follow-up, the patient-reported outcome measures had significantly improved across the study cohort compared to preoperative values. These findings include the mHHS and the iHot-12 scores (Fig. 3) as well as the UCLA and the HOOS domains – pain, sports, symptoms, activity in daily living and quality of life. Overall, 91.5% of patients achieved the mHHS MCID after the surgical procedure (Table 3).
In the subgroup analyses these findings were consistent in patients with radiographic signs of isolated lateral deficiency as well as in patients with radiographic signs of combined anterolateral/ posterolateral deficiency. The rate of patients achieving the mHHS MCID was higher in patients with combined anterolateral/posterolateral deficiency compared to isolated lateral deficiency (95.2% vs. 90.4%) postoperatively (Table 3).
Considering stable and unstable hip joints, the patient-reported outcome measures had significantly improved for stable hip joints. Patients with unstable hip joints showed a significant postoperative improvement for the mHHS and the HOOS scores regarding pain, sports and quality of life. Additionally, patients with stable hip joints achieved the mHHS MCID (92.5% vs. 85.7%) more often when compared to patients with unstable hip joints (Table 3).
Clinical failure analyses
Overall, eight hips in eight patients failed to achieve the mHHS MCID at the latest follow-up and were defined as clinical failure. The patients demographics did not differ from those of the remaining study cohort. The most commonly reported symptom was persisting pain (5/8) at the latest follow-up and two patients underwent a subsequent hip operation due to a unsatisfying outcome after the initial PAO. Half (4/8) of the patients with clinical failure had a LCEA > 30° combined with an AI of < 0° in the postoperative radiographic assessment (Table 4).
Discussion
This study illustrates that PAO significantly improved clinical symptoms and outcome scores across a variety of acetabular and joint morphologies with high patient safety in BHD. While the results demonstrate superior clinical outcomes in patients with anterolateral/posterolateral acetabular deficiency as well as for isolated lateral acetabular deficiency, the comparison of radiographically stable and unstable hip joints showed inferior postoperative outcomes for unstable hip joints.
To date, the optimal surgical therapy for patients in BHD remains a topic of debate. Studies on arthroscopy, PAO or their combination have reported improvement in clinical symptoms. While studies on radiographic and morphologic risk factors for poor outcome after arthroscopy are available, a comprehensive evaluation of clinical outcomes after PAO dependent on acetabular and hip joint morphologies is still lacking [18, 19, 24].
The most commonly used radiographic parameter to assess femoral head coverage is the LCEA of Wiberg [4]. In recent years, several additional radiographic parameters have been explored to characterize the acetabular and hip joint morphology more precisely [25,26,27]. While McClincy et al. identified gender specific acetabular subtypes in BHD, this study focused on different radiographically determined joint morphologies without gender differentiation [26]. Dornacher et al. reported up to 40% of hips with BDH combined with an anterior or posterior acetabular deficiency in their patient cohort [28], while the results of this study showing a proportion of 22.3% hips with substantial anterolateral or posterolateral acetabular deficiency. Thus, a thorough preoperative radiographic assessment is essential to facilitate a precise analysis of acetabular morphology.
Hip dysplasia and BDH have primarily been treated through acetabular reorientation via PAO or hip arthroscopy targeting intraarticular pathologies and CAM deformity [13, 29, 30]. In hip arthroscopy varying degrees of failure accompanied by a relatively high rate of reoperation have been reported [31, 32]. In this context, studies have highlighted limitations of hip arthroscopy, where a higher acetabular inclination, broken Shenton line, or acetabular retroversion correlated with higher revision rate or poor patient-reported outcomes [18, 19, 24]. In contrast, studies on PAO-treated borderline hip patients reported improved patient-reported outcomes and low complication and revision rates postoperatively [15, 17]. Recently, a small retrospective study in 42 hips with BHD reported improved patient-reported mid- to long-term outcomes of PAO for the first time [33]. In addition, the present study showed improved outcome after PAO in BHD with a minimum follow-up of 1 year.
When comparing the various acetabular and joint morphologies radiographically, unstable hip joints less frequently achieved the mHHS MCID (85.7% vs. 92.5% in stable hip joints) postoperatively. The FEAR-index, with a cut-off value of 2°, predicts hip instability with 90% probability on plain radiographs [10, 34]. Besides osseous undercoverage in anterior, lateral or posterior acetabular regions, BHD often includes labral and chondral comorbidities [35]. Since hip stability primarily depends on the osseous geometry, an osseous correction by PAO is recommended in case of instability. Additionally, studies have shown that distinct arthroscopic procedures may further worsen joint instability [36, 37]. While no correlation between the preoperative FEAR- index and the patient-reported outcome after PAO has been demonstrated [33], further research should investigate this aspect to enhance therapeutic approaches and surgical recommendations.
Despite the high overall success rate of over 90% reported in this study, eight patients failed to achieve the mHHS MCID and were defined as a clinical failure. Half of these patients exhibited postoperative radiographic signs of overcorrection (postoperative LCEA > 30° combined with a negative AI), supporting findings of Andronic et al. that reported an overcorrection in 66% of clinically failed cases and its negative correlation with patient-reported outcomes [33]. Thus, overcorrection could be a risk factor for poor outcome following PAO in BHD and must be evaluated in further studies.
While the present study reports improved patient-reported outcome in different joint subtypes, several limitations of this study must be considered. The study included only patients receiving PAO to treat BDH and there could be an increased risk for selection and treatment bias caused by a single surgeon performing all treatments in this study. A control group of patients receiving hip arthroscopy, or both was not available yet. Thus, a prospective cohort study is planned to compare hip arthroscopy and PAO in patients with BHD. Additionally, multi-centre studies could be beneficial to improve the generalizability of the results. Next, the data were limited by a minimum follow-up of 1 year. Thus, mid- and long-term outcomes have to be reported in future studies. Although a comprehensive radiographic assessment to describe the femoral and acetabular morphology was performed, most of the radiographic parameters were measured on plain pelvic X-rays, while MRI and femoral torsion measurements were not available in all patients of the study cohort. Therefore, results on accompanying soft tissue pathologies of the hip joint and femoral torsion affecting the outcome after PAO must be stated preliminary and must be further evaluated. Last, the group of patients with anterior/posterior-lateral deficiency included only 21 hips (14/7 hips), limiting a representative outcome assessment. Thus, future studies on this subgroup are planned to improve the clinical evidence in this distinct acetabular morphology.
Overall, the present study demonstrates significant clinical improvements across variable acetabular morphologies after periacetabular osteotomy in Borderline hip dysplasia. Appropriate experience in periacetabular osteotomy in combination with technical accuracy is crucial to maintain the high level of patients outcomes and safety. Further research is warranted to improve treatment recommendations, particularly regarding unstable hip joint conditions in Borderline hip dysplasia.
References
Freiman SM et al (2022) Prevalence of borderline acetabular dysplasia in symptomatic and asymptomatic populations: a systematic review and meta-analysis. Orthop J Sports Med 10(2):23259671211040456
Fredensborg N (1976) The CE angle of normal hips. Acta Orthop Scand 47(4):403–405
Henak CR et al (2011) Role of the acetabular labrum in load support across the hip joint. J Biomech 44(12):2201–2206
Wiberg G (1939) The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand 83(Suppl 58):7–38
Nepple JJ et al (2017) Three patterns of acetabular deficiency are common in young adult patients with acetabular dysplasia. Clin Orthop Relat Res 475(4):1037–1044
Wilkin GP et al (2017) A contemporary definition of hip dysplasia and structural instability: toward a comprehensive classification for acetabular dysplasia. J Arthroplast 32(9s):S20-s27
Larson CM et al (2015) Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res® 473:1247–1254
Anderson LA et al (2017) Acetabular wall indices help to distinguish acetabular coverage in asymptomatic adults with varying morphologies. Clin Orthop Relat Res® 475:1027–1033
Tönnis D (1976) Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res® 119:39–47
Wyatt M et al (2017) The Femoro-Epiphyseal Acetabular Roof (FEAR) index: a new measurement associated with instability in borderline hip dysplasia? Clin Orthop Relat Res 475:861–869
Murata Y et al (2021) Comparison between hip arthroscopic surgery and periacetabular osteotomy for the treatment of patients with borderline developmental dysplasia of the hip: a systematic review. Orthop J Sports Med 9(5):23259671211007400
Ricciardi BF et al (2017) Complications and short-term patient outcomes of periacetabular osteotomy for symptomatic mild hip dysplasia. Hip Int 27(1):42–48
McClincy MP et al (2019) Periacetabular osteotomy improves pain and function in patients with lateral center-edge angle between 18° and 25°, but are these hips really borderline dysplastic? Clin Orthop Relat Res 477(5):1145–1153
Nonnenmacher L et al (2023) Komplikationen und deren Behandlung nach PAO. Die Orthopädie 52(4):272–281
Møse FB et al (2019) High frequency of labral pathology in symptomatic borderline dysplasia: a prospective magnetic resonance arthrography study of 99 patients. J Hip Preserv Surg 6(1):60–68
Livermore A et al (2019) Correction of mildly dysplastic hips with periacetabular osteotomy demonstrates promising outcomes, achievement of correction goals, and excellent five-year survivorship. Bone Jt J 101(6_Supple_B):16–22
Nepple JJ et al (2023) Outcomes of periacetabular osteotomy for borderline acetabular dysplasia. JBJS 105(2):137–144
Zimmerer A et al (2020) Is hip arthroscopy an adequate therapy for the borderline dysplastic hip? Correlation between radiologic findings and clinical outcomes. Orthop J Sports Med 8(5):2325967120920851
Hatakeyama A et al (2018) Predictors of poor clinical outcome after arthroscopic labral preservation, capsular plication, and cam osteoplasty in the setting of borderline hip dysplasia. Am J Sports Med 46(1):135–143
Kalhor M et al (2021) Surgical anatomy of the rectus-sparing approach for periacetabular osteotomy: a cadaveric study. JBJS Essent Surg Tech 11(2)
Löchel J et al (2021) A new rectus and sartorius sparing approach for periacetabular osteotomy in patients with developmental dysplasia of the hip. J Clin Med 10(4):601
Wassilew GI et al (2022) Minimally invasive periacetabular osteotomy for adult hip dysplasia. Oper Orthop Traumatol 34(4):275–294
Kemp JL et al (2013) Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med 41(9):2065–2073
McQuivey KS et al (2020) A multicenter study of radiographic measures predicting failure of arthroscopy in borderline hip dysplasia: beware of the Tönnis angle. Am J Sports Med 48(7):1608–1615
Siebenrock KA et al (2012) The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res® 470:3355–3360
McClincy MP et al (2019) Mild or borderline hip dysplasia: are we characterizing hips with a lateral center-edge angle between 18° and 25° appropriately? Am J Sports Med 47(1):112–122
Reynolds D, Lucas J, Klaue K (1999) Retroversion of the acetabulum: a cause of hip pain. J Bone Jt Surg Br 81(2):281–288
Dornacher D et al (2023) Acetabular deficiency in borderline hip dysplasia is underestimated by lateral center edge angle alone. Arch Orthop Trauma Surg 143(7):3937–3944
Lerch TD et al (2017) One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res® 475:1154–1168
Domb BG et al (2018) Hip arthroscopic surgery with labral preservation and capsular plication in patients with borderline hip dysplasia: minimum 5-year patient-reported outcomes. Am J Sports Med 46(2):305–313
Gupta N et al (2017) Poorer arthroscopic outcomes of mild dysplasia with cam femoroacetabular impingement versus mixed femoroacetabular impingement in absence of capsular repair. Am J Orthop 46(1):E47–E53
Cvetanovich GL et al (2017) Do patients with borderline dysplasia have inferior outcomes after hip arthroscopic surgery for femoroacetabular impingement compared with patients with normal acetabular coverage? Am J Sports Med 45(9):2116–2124
Andronic O et al (2023) Factors influencing patient-reported outcomes following periacetabular osteotomy and open osteochondroplasty in the setting of borderline hip dysplasia: a retrospective study with minimum follow-up of five years. Bone Jt J 105(7):735–742
Batailler C et al (2019) Is the femoro-epiphyseal acetabular roof (FEAR) index on MRI a relevant predictive factor of instability in a borderline dysplastic hip? Bone Jt J 101(12):1578–1584
Kraeutler MJ et al (2020) A contemporary look at the evaluation and treatment of adult borderline and frank hip dysplasia. Am J Sports Med 48(9):2314–2323
Duplantier NL et al (2016) Hip dislocation or subluxation after hip arthroscopy: a systematic review. Arthrosc J Arthrosc Relat Surg 32(7):1428–1434
Wyatt MC, Beck M (2018) The management of the painful borderline dysplastic hip. J Hip Preserv Surg 5(2):105–112
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
G.I.W. serves as consultant for Mathys AG and receives institutional funding and research support from Mathys AG and Smith & Nephew. These companies did not financially support this study, had no role in study design, sample collection, data collection and analysis, decision to publish, or preparation of the manuscript. All other authors declare no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fischer, M., Nonnenmacher, L., Zimmerer, A. et al. The role of different acetabular morphologies on patient-reported outcomes following periacetabular osteotomy in borderline hip dysplasia. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05432-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05432-0