Abstract
Background
Since its first description in 1984, periacetabular osteotomy (PAO) has become an accepted treatment for hip dysplasia. The 30-year survivorship with this procedure has not been reported. Because these patients are often very young at the time of surgery, long-term followup and identification of factors associated with poor outcome could help to improve patient selection.
Questions/purposes
Looking at the initial group of patients with hip dysplasia undergoing PAO at the originator’s institution, we asked: (1) What is the cumulative 30-year survival rate free from conversion to THA, radiographic progression of osteoarthritis, and/or a Merle d’Aubigné-Postel score < 15? (2) Did hip function improve and pain decrease? (3) Did radiographic osteoarthritis progress? (4) What are the factors associated with one or more of the three endpoints: THA, radiographic progression of osteoarthritis, and/or Merle d’Aubigné-Postel score < 15?
Methods
We retrospectively evaluated the first 63 patients (75 hips) who underwent PAO for hip dysplasia between 1984 and 1987. At that time, hip dysplasia was the only indication for PAO and no patients with acetabular retroversion, the second indication for a PAO performed today, were included. During that period, no other surgical treatment for hip dysplasia in patients with closed triradiate cartilage was performed. Advanced osteoarthritis (≥ Grade 2 according to Tönnis) was present preoperatively in 18 hips (24%) and 22 patients (23 hips [31%]) had previous femoral and/or acetabular surgery. Thirty-nine patients (42 hips [56%]) were converted to a THA and one patient (one hip [1%]) had hip fusion at latest followup. Two patients (three hips [4%]) died from a cause unrelated to surgery 6 and 16 years after surgery with an uneventful followup. From the remaining 21 patients (29 hips), the mean followup was 29 years (range, 27–32 years). Of those, five patients (six hips [8%]) did not return for the most recent followup and only a questionnaire was available. The cumulative survivorship of the hip according to Kaplan-Meier was calculated if any of the three endpoints, including conversion to THA, progression of osteoarthritis by at least one grade according to Tönnis, and/or a Merle d’Aubigné-Postel score < 15, occurred. Hip pain and function were assessed with Merle d’Aubigné-Postel score, Harris hip score, limp, and anterior and posterior impingement tests. Progression of radiographic osteoarthritis was assessed with Tönnis grades. A Cox regression model was used to calculate factors associated with the previously defined endpoints.
Results
The cumulative survivorship free from conversion to THA, radiographic progression of osteoarthritis, and/or Merle d’Aubigné-Postel score < 15 was 29% (95% confidence interval, 17%-42%) at 30 years. No improvement was found for either the Merle d’Aubigné-Postel (15 ± 2 versus 16 ± 2, p = 0.144) or Harris hip score (83 ± 11 versus 85 ± 17, p = 0.602). The percentage of a positive anterior impingement test (39% versus 14%, p = 0.005) decreased at 30-year followup, whereas the percentage of a positive posterior impingement test (14% versus 3%, p = 0.592) did not decrease. The percentage of positive limp decreased from preoperatively 66% to 18% at 30-year followup (p < 0.001). Mean osteoarthritis grade (Tönnis) increased from preoperatively 0.8 ± 1 (0–3) to 2.1 ± 1 (0–3) at 30-year followup (p < 0.001). Ten factors associated with poor outcome defined as THA, radiographic progression of osteoarthritis, and/or Merle d’Aubigné-Postel score < 15 were found: preoperative age > 40 years (hazard ratio [HR] 4.3 [3.7–4.9]), a preoperative Merle d’Aubigné-Postel score < 15 (HR 4.1 [3.5–4.6]), a preoperative Harris hip score < 70 (HR 5.8 [5.2–6.4]), preoperative limp (HR 1.7 [1.4–1.9]), presence of a preoperative positive anterior impingement test (HR 3.6 [3.1–4.2]), presence of a preoperative positive posterior impingement test (HR 2.5 [1.7–3.2]), a preoperative internal rotation of < 20° (HR 4.3 [3.7–4.9]), a preoperative Tönnis Grade > 1 (HR 5.7 [5.0–6.4]), a postoperative anterior coverage > 27% (HR 3.2 [2.5–3.9]), and a postoperative acetabular retroversion (HR 4.8 [3.4–6.3]).
Conclusions
Thirty years postoperatively, 29% of hips undergoing PAO for hip dysplasia can be preserved, but more than 70% will develop progressive osteoarthritis, pain, and/or undergo THA. Periacetabular osteotomy is an effective technique to treat symptomatic hip dysplasia in selected and young patients with closed triradiate cartilage. Hips with advanced joint degeneration (osteoarthritis Tönnis Grade ≥ 2) should not be treated with PAO. Postoperative anterior acetabular overcoverage or postoperative acetabular retroversion were associated with decreased joint survival.
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Introduction
Since its first description in 1988 [9], periacetabular osteotomy (PAO) has become one of the most frequently performed surgical procedures to treat hip dysplasia. Several long-term studies have proven the efficacy of this procedure [1, 3, 14, 41]. The abnormal anatomy and decreased area of the lunate surface in hip dysplasia [40] result in axial overloading with decreased contact area, increased contact pressure, and maximum loading at the acetabular rim [17]. At 20-year followup, 60% of patients undergoing PAO for hip dysplasia reportedly presented with good to excellent clinical results, no progression of osteoarthritis, and no need for conversion to THA [41]. An unfavorable outcome was associated with increased age at surgery, decreased preoperative Merle d’Aubigné-Postel score [8], preoperative positive anterior impingement test, preoperative limp, preoperative osteoarthritis, and a decreased postoperative extrusion index.
The 30-year survivorship with this procedure has not been reported. Because these patients are often very young at the time of surgery, long-term followup and identification of factors associated with osteoarthritis progression, poor clinical outcome, and conversion to THA could help to improve patient selection.
The aim of this study was to review the series of the very first patients after PAO for hip dysplasia at the originator’s institution with a followup of 30 years, of whom the results after 10 and 20 years have been presented previously in this journal [39, 41]. We asked: (1) What is the cumulative 30-year survival rate of the hip free from any of the following endpoints: conversion to THA, progression of osteoarthritis, and a Merle d’Aubigné-Postel score [8] < 15? (2) Did function of the hip improve and pain decrease assessed with the Merle d’Aubigné-Postel score, Harris hip score (HHS), the prevalence of limp, anterior and posterior impingement test, and full ROM? (3) Did osteoarthritis progress at 30-year followup evaluated using the Tönnis score? (4) What are the factors associated with any of the endpoints defined as conversion to THA, progression of osteoarthritis, or a Merle d’Aubigné-Postel score < 15?
Patients and Methods
We retrospectively evaluated the same subset of 63 patients (75 hips) on whom we previously reported with a 10- and 20-year followup after PAO for the treatment of hip dysplasia [39, 41]. The study was approved by the local institutional review board.
The operations were performed between April 1984 and December 1987. These patients represent a series of the very first Bernese PAOs performed at the originator’s institution [9, 26, 37] with a minimum followup of 27 years (mean, 29 years; range, 27–32 years). During the period in question, the only indication for a PAO was dysplasia in hips with closed triradiate cartilage. To protect the open triradiate cartilage in very young patients, a triple osteotomy was performed in these hips. No other surgical treatments were performed for hip dysplasia during this time. Since 1997, a second indication for PAO has been acetabular retroversion with the goal of anteverting the acetabulum [38]. There was considerable heterogeneity in the current patient series in terms of indications, preoperative osteoarthritis, and a high number of previous surgeries (Table 1). Five patients (six hips [8%]) presented with an underlying neurologic disorder with dysplasia (meningomyelocele, cerebral palsy, paraparesis). Two patients (two hips [3%]) had a proximal femoral focal deficiency, and posttraumatic acetabular deficiency was present in two patients (two hips [3%]). Advanced osteoarthritis (≥ Grade 2 according to Tönnis [51]) was preoperatively present in 18 hips (24%) (Table 1). Twenty-two patients (23 hips [31%]) had previous surgery (Table 2) to achieve sufficient acetabular coverage (intertrochanteric osteotomy, acetabular osteotomy, shelfplasty, or a combination). Twelve patients (16%) had bilateral procedures and 13 patients (16 hips [21%]) had a concomitant intertrochanteric osteotomy (Table 2). Severity of hip dysplasia was graded according to the classification of Severin et al. [36].
From the initial 63 patients (75 hips), 39 patients (42 hips [56%]) were converted to THA and one patient (one hip [1%]) had hip fusion (Fig. 1) at latest followup. Two patients (three hips [4%]) died from a cause unrelated to surgery 6 and 16 years after surgery with an uneventful followup (no conversion to THA, no progression of osteoarthritis, a Merle d’Aubigné-Postel score > 15). From the remaining 21 patients (29 hips; Fig. 1), we had a mean followup of 29 years (range, 27–32 years). Of those, five patients (six hips [8%]) did not return for the most recent followup but they returned a questionnaire. In addition, radiographic and clinical information of these five patients (six hips) was available from the last followups ranging from 11 to 21 years. Sixteen patients (23 hips) were available for complete clinical and radiographic evaluation at most recent followup.
Patient selection for the 30-year PAO followup study is shown. *Died unrelated to surgery with an uneventful followup 6 and 16 years after surgery; †patients did not return for 30-year followup but returned a questionnaire with clinical scores. These patients had a last clinical and radiographic followup at 11 to 21 years after surgery.
We calculated survival rate at the 30-year followup and defined failure if any of the following occurred: conversion to THA, progression of osteoarthritis by at least one grade according to the Tönnis classification [51], or a Merle d’Aubigné-Postel score [8] of < 15 at most recent followup. From the five patients (six hips) with questionnaire followup only, one patient (one hip) was considered a failure as a result of osteoarthritis progression at 11 years. The other four patients (five hips) were considered survivors because they did not show progression of osteoarthritis at latest radiographic followup (range, 12–21 years) and they presented with good to excellent clinical results (minimal HHS of 96, high activity level with a UCLA score of at least 5, and a maximum WOMAC score of 6) at the time of questionnaire followup (range, 28–30 years).
Clinical evaluation at most recent followup was performed by one of the authors (TDL, not involved in the surgical care of the patients). Clinical evaluation included assessment of limp, the presence of a positive anterior impingement test (pain in combined flexion and internal rotation), the presence of a posterior impingement test (pain in combined extension and external rotation), and full goniometric ROM. As a clinical scoring system, the Merle d’Aubigné-Postel [8] and the HHS [13] were assessed. Different observers performed the clinical evaluation preoperatively and at 10-, 20-, and 30-year followup. However, substantial inter- and intraobserver agreement has been published for the anterior impingement test [27], ROM [18, 30, 55], and the Merle d’Aubigné-Postel score [22].
Radiographic evaluation consisted of an AP pelvic radiograph and a cross-table lateral view of the hip acquired in a standardized fashion [49]. Osteoarthritis was graded according to the classification of Tönnis [51]. Coxometric parameters on the pre- and postoperative AP pelvis radiographs were assessed using validated software (Hip2Norm; University of Bern, Bern, Switzerland) [47, 50, 58]. Because the original radiographs were not calibrated, we did not adjust the radiographs for variances of pelvic tilt but did so for pelvic rotation. We assessed the following six acetabular parameters for quantification of reorientation in all patients: caudocranial femoral head coverage, anterior coverage, posterior coverage, lateral center-edge angle, acetabular index, and extrusion index. Similar to a previous study [1], the acetabular reorientation was judged optimal if at least four of the six parameters were within previously determined reference values [46]. Additionally, femoral head sphericity was assessed by the head sphericity index [42]. An aspherical head was then defined by a sphericity index of 0.87 or less [1]. Based on this allocation, eight patients (eight hips [11%]) had a spherical head. Fifty-five patients (67 hips [89%]) were judged as having an aspherical femoral head.
We then calculated factors associated with any of the endpoints defined as conversion to THA, progression of osteoarthritis, or a Merle d’Aubigné-Postel score < 15. Therefore, we evaluated both demographic (Table 1) and surgery-related data (Table 2) of the patient series. In addition, we evaluated preoperative radiographic data describing the morphology of the hip (Table 3), joint degeneration using the Tönnis grading system, and postoperative radiographic data describing the corrected morphology of the hip (Table 3).
Survival rate was calculated using the method of Kaplan-Meier [21]. Hips without a 30-year followup or from patients who died were included as censored data. Normal distribution was tested for all continuous parameters using the Kolmogorov-Smirnov test. Because not all of them were normally distributed, we used nonparametric tests only. Hip function and pain were compared among the preoperative status and the different followups using the Friedman test. Pairwise comparison of clinical data was performed using the Wilcoxon signed-rank test with Bonferroni adjustment for the level of significance. Binominal clinical data were compared using the chi square test. Radiographic data were compared between the preoperative and postoperative status using the Wilcoxon signed-rank test for continuous data and the Fisher’s exact test for binominal data. The Cox proportional hazard model [6] was used to detect factors associated with one or more of the previously defined endpoints and corresponding hazard ratios were calculated.
Results
We found a cumulative survivorship free from THA, progression of osteoarthritis, and a Merle d’Aubigné-Postel score of < 15 of 29% (95% confidence interval [CI], 17%–42%) at 30-year followup (Fig. 2). Fifty hips (67%) reached one of the defined endpoints. Forty-two hips (56%) had been converted to THA and one hip (1%) was fused (the one hip with fusion was taken into account as THA for statistics) after a mean followup of 16 ± 8 years (range, 1–30 years). Seven hips (9%) had a Merle d’Aubigné-Postel score of < 15 at most recent followup. Four hips (5%) sustained progression of osteoarthritis during the followup period.
Survival rate of hips after PAO up to a followup of 30 years is shown. Endpoints were defined as conversion to THA, progression of osteoarthritis, and a Merle d’Aubigné-Postel [8] score of < 15. Values are expressed as cumulative survivorship with 95% confidence interval (CI) in parentheses for each 10-year interval.
Hip function and pain at 30-year followup compared with the preoperative status did not improve except for the prevalence of a positive anterior impingement test (39% versus 14%; p = 0.005) and for the prevalence of limp, which decreased from 66% to 18% (p = 0.016). No difference between the 30-year followup and the preoperative status was found for the Merle d’Aubigné-Postel score (preoperative 15 ± 2 [9–18] versus 16 ± 2 [12–18], p = 0.144) or the HHS (preoperative 83 ± 11 [50–100] versus 85 ± 17 [43–100], p = 0.602). In both scores an improvement was found for the 10-year followup with no more improvement at 20- and 30-year followups (Table 4). There was no difference for the prevalence of a posterior impingement test (14% versus 3%; p = 0.592) at the 30-year followup compared with the preoperative status. At the most recent followup, flexion, internal rotation, external rotation, and abduction were decreased compared with the preoperative status, whereas extension and adduction did not differ (Table 4).
Osteoarthritis progressed from a preoperative mean osteoarthritis score according to Tönnis of 0.8 ± 1 (0–3) to 2.1 ± 1 (0–3) (THA or hip fusion was taken into account as Tönnis Grade 3; p < 0.001). Preoperatively 50 of 66 hips (76%) had no or only minor degenerative changes (Tönnis Grade ≤ 1; Fig. 3). At 30-year followup, 19 of 66 hips (29%) showed no progression of osteoarthritis (Fig. 3). Progression of osteoarthritis was dependent on the preoperative osteoarthritis score (Fig. 3). In 15 of 30 hips (50%) with no preoperative signs of osteoarthritis (Tönnis Grade 0), no progression of osteoarthritis was seen at 30-year followup. With increasing preoperative osteoarthritis, the proportion of hips with no progression of osteoarthritis at 30-year followup decreased: three of 20 hips (15%) with preoperative Grade 1, one of 15 hips (7%) with preoperative Grade 2, and no hip with preoperative Grade 3 avoided progression of osteoarthritis at most recent followup.
The distribution of preoperative osteoarthritis according to the Tönnis grades [51] in hips undergoing PAO is shown. At 30-year followup, the progression of osteoarthritis or conversion to THA depending on the preoperative grade of osteoarthritis is displayed.
We found 10 factors associated with any of the following endpoints including THA, progression of osteoarthritis, and a Merle d’Aubigné-Postel score of < 15 (Table 5). This included the demographic factor of age at operation > 40 years (hazard ratio [HR] 4.3 with 95% confidence interval [CI], 3.7–4.9, p < 0.001) with direct implication on 30-year survival (Fig. 4A). In addition, six preoperative clinical factors including a preoperative Merle d’Aubigné-Postel score < 15 (HR 4.1 with 95% CI, 3.5–4.6, p < 0.001), a preoperative HHS < 70 (HR 5.8 with 95% CI, 5.2–6.4, p < 0.001; Fig. 4B), presence of preoperative limp (HR 1.7 with 95% CI, 1.4–1.9, p = 0.001), presence of a preoperative positive anterior impingement test (HR 3.6 with 95% CI, 3.1–4.2, p < 0.001), presence of a preoperative positive posterior impingement test (HR 2.5 with 95% CI, 1.7–3.2, p = 0.021), and preoperative internal rotation < 20° (HR 4.3 with 95% CI, 3.7–4.9, p = 0.021) were found. Furthermore, we noted three radiographic factors including preoperative osteoarthritis Tönnis Grade > 1 (HR 5.7 with 95% CI, 5.0–6.4, p < 0.001; Fig. 4C), a postoperative anterior coverage > 27% (HR 3.2 with 95% CI, 2.5–3.9, p = 0.001), and postoperative retroversion defined as an anterior acetabular coverage > 27% with combined posterior coverage < 36% defined according to Tannast et al. [46] (HR 4.8 with 95% CI, 3.4–6.3, p = 0.034).
Survivorship rate at 30 years was dependent on different factors associated with endpoints (THA, progression of osteoarthritis [OA], and a Merle d’Aubigné-Postel score < 15). (A) In hips with an age at operation < 20 years, survival was 56% at 30 years, whereas no hip survived at 30 years with a preoperative age > 45 years. (B) Hips with no preoperative osteoarthritis had a survival rate of 42% at 30 years compared with 8% of hips with a preoperative osteoarthritis score according to Tönnis Grade ≥ 2. (C) Forty-seven percent of hips with a preoperative HHS > 90 survived 30 years compared with 4% in hips with a HHS < 70.
Discussion
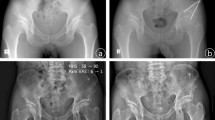
Since its introduction in 1984, PAO [9] has become one of the most frequently performed surgical procedures to treat hip dysplasia in adolescents and young adults. Several mid- to long-term studies have been published showing the potential beneficial effect on joint survival after PAO [1, 3, 7, 14, 35, 39, 41, 54]. To our knowledge, however, no reports about the 30-year survivorship with this procedure have been published. Because these patients are often very young at the time of surgery, long-term followup and identification of factors associated with osteoarthritis progression, poor clinical outcome, and conversion to THA could help to improve patient selection. At the 30-year followup, we found in 29% of the hips a good to excellent clinical result, no progression of osteoarthritis, and/or no conversion to THA (Fig. 5A–E); however, more than 70% will develop progressive osteoarthritis, pain, and/or undergo THA (Fig. 6A–E). There were 10 factors associated with THA, progression of osteoarthritis, or a poor clinical result including increased preoperative age, decreased preoperative Merle d’Aubigné-Postel score or HHS, preoperative limp, preoperative anterior and posterior impingement test, decreased preoperative internal rotation, increased osteoarthritis, postoperative anterior acetabular overcoverage, or postoperative acetabular retroversion (Table 5).
(A) A 15-year-old female patient presented with hip dysplasia and subluxation of the joint (broken Shenton’s line). (B) PAO to increase femoral head coverage was performed. At 10-year (C), 20-year (D), and 30-year followup (E), the joint space was well preserved and the patient presented without hip pain (Merle d’Aubigné-Postel score 18).
(A) A 28-year-old woman presented with hip dysplasia with preserved joint space. (B) Twelve years later the patient presented with complete joint space narrowing and cystic changes of the femoral head. (C) Despite the preoperative degeneration of the joint, PAO was performed to improve femoral head coverage. Joint space width improved after surgery. (D) At 13-year followup after PAO, the joint showed marked progression of osteoarthritis and (E) conversion to THA was performed.
The limitations of the current study are similar to those from our previous report [41]. First, there is a lack of a control group with dysplastic hips without surgical treatment. Second, the clinical parameters were assessed by different observers at each followup, which is a reflection of the long timespan of the study. Therefore, differences in clinical outcome scores such as the Merle d’Aubigné-Postel score or HHS could have been missed. However, substantial inter- and intraobserver agreement has been reported for the anterior impingement test [27], ROM [18, 30, 55], and the Merle d’Aubigné-Postel score [8]. Thus, we do not believe that this affects our conclusions to a relevant degree. Third, the current series of patients reflects the learning curve and the very first experiences of a new, demanding surgical technique that could be associated with a higher rate of complications and results. Additionally, there was considerable heterogeneity in terms of indications, varying degrees of dysplasia (Table 1), osteoarthritis grade (Fig. 3), a high number of previous operations (Table 2), and additional underlying diseases. Although these variations likely reduced the overall 30-year survivorship results, they at least allow an analysis of factors confounding long-term survival.
Last, five patients (six hips) did not return for 30-year followup. One patient (one hip) was considered a failure because of osteoarthritis progression at latest followup. The remaining four patients (five hips) were included as survivors because they had good to excellent scores (HHS > 96, UCLA score > 5, and WOMAC score < 6) at 28 to 30 years followup. In addition, latest radiographic followup of these patients was available from 12 to 21 years after surgery and did not show progression of osteoarthritis. Therefore, survival at 30 years could be overestimated because one of these hips without 30-year radiographic followup could have had progression of osteoarthritis without an increase in pain or limitations of daily activities.
Comparing the survival rate at 30-year followup with the previous reports [39, 41] of the same patient series shows a decrease after 10 years with a linear decline after 20-year followup (Fig. 2). Inclusion of the secondary endpoints (progression of osteoarthritis and a Merle d’Aubigné Postel score of < 15) allows a more distinct conclusion for the reader regarding success and failure of surgery. However, most reports comprise conversion to THA as a single endpoint (Table 6). With this single endpoint, the 30-year survivorship of the current series was 43% (42 of 75 hips [56%] were converted to THA and one hip (1%) underwent hip fusion; Fig. 7). This result is in line with the reported results about PAO and other pelvic osteotomies for hip dysplasia showing a continuous linear decline up to 30 years (Fig. 7). Reported survival for PAO ranges from 93% to 64% between 10- and 20-year followup (Fig. 7) [1, 14, 39, 41, 52]. Superior survival was reported for some triple, Chiari, and rotational osteotomies with survival rates ranging from 100% to 82% after 10 to 23 years after surgery (Fig. 7) [15, 16, 19, 20, 56, 57]. The increased survivorship could be the result of the decreased age at operation [2, 3, 12, 33, 57], typically in hips with Chiari or triple osteotomies [2, 12, 19]. Other possible reasons include the lack of hips with advanced osteoarthritis [14, 44, 54], a lower followup rate [7, 11, 23, 25, 31, 32, 35, 45, 53], and a decreased percentage of hips with previous surgery [28, 54]. In addition, the current patient series is consecutive and includes the very first cases from a new surgical technique and therefore represent the beginning of the learning curve. Comparing survivorship of pelvic osteotomies with survivorship of THA (with reoperation as the endpoint) in females younger than 50 years (comparable demographics to those found for pelvic osteotomies) from the Swedish Hip Registry [10] shows a similar decline over 30 years (Fig. 7). This indicates that, theoretically, PAO can reduce the need for revision THA by at least one surgical intervention.
The bubble chart shows the followup time, size of the study in terms of number of patients included (size of bubble), treatment (color), and survival rate with conversion to THA as the only endpoint of selected literature [1–3, 7, 11, 12, 14–16, 19, 20, 23, 25, 31–35, 39, 41, 44, 45, 52–54, 56, 57] for pelvic osteotomies in hips with dysplasia. The gray line represents the survivorship of THAs performed in female patients younger than 50 years of age from the Swedish Hip Registry [10] for comparison with the pelvic osteotomies.
No improvement in hip pain and function was found for the hips without conversion to THA at the 30-year followup despite the decreased prevalence of limp and anterior impingement test (Table 4). After improvement of the clinical scores at 10-year followup, both the Merle d’Aubigné-Postel score and the HHS decreased to the preoperative values at 30 years followup (Table 4). ROM was decreased after surgery and at 30 years followup. Using computer-assisted and dynamic assessment of ROM, it could be shown that the typically excessive ROM in dysplastic hips is decreased to a normal level after PAO [43]. Studies reporting short- to midterm followup (< 15 years) for PAO and other pelvic osteotomies found an improved clinical outcome [5, 20, 44, 54, 57]. This difference in clinical outcome might be the result of the longer followup in the current study or the previously mentioned demographic differences including decreased age at operation [3], less hips with advanced osteoarthritis [54, 14, 44], or a decreased percentage of hips with previous surgery [44, 28, 57, 54].
Mean osteoarthritis was advanced at the 30-year followup and in only 19 of 66 hips (29%) osteoarthritis was unchanged (Fig. 2). Some reports with a followup ranging from 10 to 20 years were in accordance with our results [4, 29, 57]. Others have reported on preservation of the joint without progression of osteoarthritis at midterm followup [53]. This difference might be mainly the result of the decreased followup and the preoperative decreased proportion of hips with advanced degeneration. Progression of joint degeneration was clearly associated with the preoperative grade of joint degeneration (Fig. 3): 18 out of 50 (36%) hips with no or only mild degeneration (≤ Tönnis Grade 1) had no progression at 30-year followup compared to one of 16 hips (6%) with advanced osteoarthritis (≥ Tönnis Grade 2).
Factors associated with the endpoints conversion to THA, progression of osteoarthritis, or a Merle d’Aubigné-Postel score < 15 found at the 30- and 20-year followup [41] were preoperative age > 40 years, a preoperative Merle d’Aubigné-Postel score < 15, preoperative limp, a preoperative positive anterior impingement test, and preoperative osteoarthritis > 1 Grade according to Tönnis (Table 5). Additional factors found at the 30-year followup were a preoperative HHS < 70, a preoperative positive posterior impingement test, limited preoperative internal rotation < 20°, postoperative anterior overcoverage, and postoperative acetabular retroversion. In contrast, a decreased postoperative extrusion index was no longer found to be a factor associated with failure. Eight of 10 factors are given at the time of surgery and can possibly be influenced by the surgery. These eight factors are determined by the degeneration of the joint and the age of the patient. The two factors that can be controlled by the surgeon are the postoperative anterior overcoverage and postoperative acetabular retroversion. Accurate acetabular reorientation with avoidance of retroversion was previously associated with decreased survivorship [1, 48]. Accurate acetabular anteversion in combination with adequate femoral offset resulted in a survivorship of 91% at 10-year followup after PAO [1]. In the literature, the most commonly reported factors associated with failure after pelvic osteotomies for hip dysplasia were increased age [1, 14, 28, 41, 54, 57], advanced radiographic joint degeneration [1, 7, 14, 16, 24, 33, 41, 52, 54], and increased preoperative pain with decreased clinical scores [1, 16, 24, 41] (Table 6). Also, with increasing severity of dysplasia [1, 52, 56], a decreased survival rate after PAO or Chiari osteotomy was found. Next, various factors associated with failure that are subject to surgical accuracy are reported (Table 6). These include a postoperative deficient acetabular coverage [1, 7, 11, 14, 23, 41] as a result of undercorrection or postoperative joint incongruency [11, 14, 28, 57]. In addition, excessive acetabular coverage [11, 14], acetabular retroversion [1], or nonspherical femoral head [1, 33, 56] were reported, which potentially can result in postoperative femoroacetabular impingement.
In conclusion, at 30-year followup after PAO, the joint is preserved in 29% of hips without pain or progression of osteoarthritis. However, 71% of hips developed progressive arthritis, pain, and/or underwent THA. Eight of 10 factors associated with failure were inherently given at the time of first presentation to the orthopaedic surgeon. Therefore, it becomes clear that results could be improved by early referrals by a well-instructed general practitioner. Other factors such as accurate reorientation of the acetabular fragment can be controlled by the surgeon. The optimal patient for PAO based on our results would be younger than 40 years with little or no pain, no limp or positive impingement test, and osteoarthritis Grade ≤ 1 according to Tönnis. Therefore, today’s results might be better given the more precise indication limiting PAO to hips without advanced osteoarthritis, more comprehensive understanding of the goals of reorientation, and concomitant head-neck osteoplasty; however, this will be for future studies to determine.
References
Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602–1614.
Calvert PT, August AC, Albert JS, Kemp HB, Catterall A. The Chiari pelvic osteotomy. A review of the long-term results. J Bone Joint Surg Br. 1987;69:551–555.
Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005;87:254–259.
Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007;89:1417–1423.
Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041–2052.
Cox D. Regression models and life tables. J R Stat Soc [Ser B]. 1972;34:187–220.
Dahl LB, Dengsø K, Bang-Christiansen K, Petersen MM, Stürup J. Clinical and radiological outcome after periacetabular osteotomy: a cross-sectional study of 127 hips operated on from 1999-2008. Hip Int. 2014;24:369–380.
D’Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475.
Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36.
Garellick G, Kärrholm J, Lindahl H, Malchau H, Rogmark C, Rolfson O. Swedish Hip Arthroplasty Registry Annual Report 2013. Available at: http://www.shpr.se/Libraries/Documents/AnnualReport_2013-04-1_1.sflb.ashx. Accessed April 22, 2016.
Grammatopoulos G, Wales J, Kothari A, Gill HS, Wainwright A, Theologis T. What is the early/mid-term survivorship and functional outcome after Bernese periacetabular osteotomy in a pediatric surgeon practice? Clin Orthop Relat Res. 2016;474:1216–1223.
Guille JT, Forlin E, Kumar SJ, MacEwen GD. Triple osteotomy of the innominate bone in treatment of developmental dysplasia of the hip. J Pediatr Orthop. 1992;12:718–721.
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755.
Hartig-Andreasen C, Troelsen A, Thillemann TM, Søballe K. What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res. 2012;470:2978–2987.
Hasegawa Y, Iwase T, Kitamura S, Yamauchi Ki K, Sakano S, Iwata H. Eccentric rotational acetabular osteotomy for acetabular dysplasia: follow-up of one hundred and thirty-two hips for five to ten years. J Bone Joint Surg Am. 2002;84:404–410.
van Hellemondt GG, Sonneveld H, Schreuder MHE, Kooijman MP, de Kleuver M. Triple osteotomy of the pelvis for acetabular dysplasia: results at a mean follow-up of 15 years. J Bone Joint Surg Br. 2005;87:911–915.
Hipp JA, Sugano N, Millis MB, Murphy SB. Planning acetabular redirection osteotomies based on joint contact pressures. Clin Orthop Relat Res. 1999;364:134–143.
Holm I, Bolstad B, Lütken T, Ervik A, Røkkum M, Steen H. Reliability of goniometric measurements and visual estimates of hip ROM in patients with osteoarthrosis. Physiother Res Int. 2000;5:241–248.
Ito H, Tanino H, Yamanaka Y, Nakamura T, Minami A, Matsuno T. The Chiari pelvic osteotomy for patients with dysplastic hips and poor joint congruency: long-term follow-up. J Bone Joint Surg Br. 2011;93:726–731.
Kaneuji A, Sugimori T, Ichiseki T, Fukui K, Takahashi E, Matsumoto T. Rotational acetabular osteotomy for osteoarthritis with acetabular dysplasia: conversion rate to total hip arthroplasty within twenty years and osteoarthritis progression after a minimum of twenty years. J Bone Joint Surg Am. 2015;97:726–732.
Kaplan E, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481.
Kirmit L, Karatosun V, Unver B, Bakirhan S, Sen A, Gocen Z. The reliability of hip scoring systems for total hip arthroplasty candidates: assessment by physical therapists. Clin Rehabil. 2005;19:659–661.
de Kleuver M, Kooijman MA, Pavlov PW, Veth RP. Triple osteotomy of the pelvis for acetabular dysplasia: results at 8 to 15 years. J Bone Joint Surg Br. 1997;79:225–229.
Kralj M, Mavcic B, Antolic V, Iglic A, Kralj-Iglic V. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7-15-year follow-up of 26 hips. Acta Orthop. 2005;76:833–840.
Lack W, Windhager R, Kutschera HP, Engel A. Chiari pelvic osteotomy for osteoarthritis secondary to hip dysplasia. Indications and long-term results. J Bone Joint Surg Br. 1991;73:229–234.
Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. Instr Course Lect. 2001;50:229–238.
Martin RL, Sekiya JK. The interrater reliability of 4 clinical tests used to assess individuals with musculoskeletal hip pain. J Orthop Sports Phys Ther. 2008;38:71–77.
Matheney T, Kim Y-J, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123.
Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999;363:21–32.
McWhirk LB, Glanzman AM. Within-session inter-rater reliability of goniometric measures in patients with spastic cerebral palsy. Pediatr Phys Ther. 2006;18:262–265.
Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10-23 years. Acta Orthop Scand. 1998;69:259–265.
Nozawa M, Shitoto K, Matsuda K, Maezawa K, Kurosawa H. Rotational acetabular osteotomy for acetabular dysplasia. A follow-up for more than ten years. J Bone Joint Surg Br. 2002;84:59–65.
Ohashi H, Hirohashi K, Yamano Y. Factors influencing the outcome of Chiari pelvic osteotomy: a long-term follow-up. J Bone Joint Surg Br. 2000;82:517–525.
Pedersen AB, Mehnert F, Havelin LI, Furnes O, Herberts P, Kärrholm J, Garellick G, Mäkela K, Eskelinen A, Overgaard S. Association between fixation technique and revision risk in total hip arthroplasty patients younger than 55 years of age. Results from the Nordic Arthroplasty Register Association. Osteoarthritis Cartilage. 2014;22:659–667.
Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926.
Severin E. Contribution to the knowledge of congenital dislocation of the hip joint: late results of closed reduction and arthrographic studies on recent cases. Acta Chir Scand. 1941;84:1–142.
Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239–245.
Siebenrock KA, Schaller C, Tannast M, Keel M, Büchler L. Anteverting periacetabular osteotomy for symptomatic acetabular retroversion: results at ten years. J Bone Joint Surg Am. 2014;96:1785–1792.
Siebenrock KA, Schöll E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20.
Steppacher SD, Lerch TD, Gharanizadeh K, Liechti EF, Werlen SF, Puls M, Tannast M, Siebenrock KA. Size and shape of the lunate surface in different types of pincer impingement: theoretical implications for surgical therapy. Osteoarthritis Cartilage. 2014;22:951–958.
Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644.
Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790.
Steppacher SD, Zurmühle CA, Puls M, Siebenrock KA, Millis MB, Kim Y-J, Tannast M. Periacetabular osteotomy restores the typically excessive range of motion in dysplastic hips with a spherical head. Clin Orthop Relat Res. 2015;473:1404–1416.
van Stralen RA, van Hellemondt GG, Ramrattan NN, de Visser E, de Kleuver M. Can a triple pelvic osteotomy for adult symptomatic hip dysplasia provide relief of symptoms for 25 years? Clin Orthop Relat Res. 2013;471:584–590.
Takatori Y, Ninomiya S, Nakamura S, Morimoto S, Moro T, Nagai I, Mabuchi A. Long-term results of rotational acetabular osteotomy in patients with slight narrowing of the joint space on preoperative radiographic findings. J Orthop Sci. 2001;6:137–140.
Tannast M, Hanke MS, Zheng G, Steppacher SD, Siebenrock KA. What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res. 2015;473:1234–1246.
Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26:1199–1205.
Tannast M, Pfander G, Steppacher SD, Mast JW, Ganz R. Total acetabular retroversion following pelvic osteotomy: presentation, management, and outcome. Hip Int. 2013;23(Suppl 9):S14-26.
Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis–what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552.
Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190.
Tönnis D. General radiography of the hip joint. In: Tönnis D, ed. Congenital Dysplasia, Dislocation of the Hip. New York, NY, USA: Springer; 1987.
Troelsen A, Elmengaard B, Søballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179.
Trumble SJ, Mayo KA, Mast JW. The periacetabular osteotomy. Minimum 2 year followup in more than 100 hips. Clin Orthop Relat Res. 1999;363:54–63.
Wells J, Millis M, Kim Y-J, Bulat E, Miller P, Matheney T. Survivorship of the Bernese periacetabular osteotomy: what factors are associated with long-term failure? Clin Orthop Relat Res. 2016 May 12. [Epub ahead of print]
Wyss TF, Clark JM, Weishaupt D, Nötzli HP. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152–158.
Yanagimoto S, Hotta H, Izumida R, Sakamaki T. Long-term results of Chiari pelvic osteotomy in patients with developmental dysplasia of the hip: indications for Chiari pelvic osteotomy according to disease stage and femoral head shape. J Orthop Sci. 2005;10:557–563.
Yasunaga Y, Ochi M, Yamasaki T, Shoji T, Izumi S. Rotational Acetabular osteotomy for pre- and early osteoarthritis secondary to dysplasia provides durable results at 20 years. Clin Orthop Relat Res. 2016;474:2145–2153.
Zheng G, Tannast M, Anderegg C, Siebenrock KA, Langlotz F. Hip2Norm: an object-oriented cross-platform program for 3D analysis of hip joint morphology using 2D pelvic radiographs. Comput Methods Programs Biomed. 2007;87:36–45.
Acknowledgments
Funding was provided by Schweizerischer Nationalfonds zur Förderung der Wissenschaftlichen Forschung (CH) (Grant No. PP00P3_144856).
Author information
Authors and Affiliations
Corresponding author
Additional information
One author (MT) has received funding from the Swiss National Science Foundation.
Each author certifies that he, or a member of his immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Lerch, T.D., Steppacher, S.D., Liechti, E.F. et al. One-third of Hips After Periacetabular Osteotomy Survive 30 Years With Good Clinical Results, No Progression of Arthritis, or Conversion to THA. Clin Orthop Relat Res 475, 1154–1168 (2017). https://doi.org/10.1007/s11999-016-5169-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-016-5169-5