Abstract
Background
Hip fracture is an important and prevalent medical condition associated with adverse outcomes. The aim of this article is to systematically review and summarise the predictors of poor functional outcomes and mortality for patients with hip fractures.
Methods
We conducted a systemic literature search using PubMed, EMBASE and Cochrane Library. We included English peer-reviewed cohort studies that examined predictors of poor functional outcomes (such as independence in Activities of Daily Living) and mortality for patients with hip fracture published in the past 15 years (from 1 Jan 2004 up to 30 May 2019). Two independent researchers evaluated the articles for eligibility. Consensus on the eligibility was sought and a third researcher was involved if there was disagreement. A standardised form was used to extract relevant data. The Newcastle-Ottawa Scale (NOS) was used to assess the quality of the included studies.
Results
We retrieved 4339 and included 81 articles. We identified two emerging predictors of poor functional outcomes and mortality for patients with hip fractures: low hand grip strength and frailty in line with an emerging concept of “physical performance”. The predictors identified in this systematic review can be grouped into 1) medical factors, such as presence of co-morbidities, high American Society of Anesthesiologists (ASA) grade, sarcopenia, 2) surgical factors including delay in operation (e.g. > 48 h), type of fracture s, 3) socio-economic factors which include age, gender, ethnicity, and 4) system factors including lower case-volume centers.
Conclusions
This systematic review identified multiple significant predictors of poor functional outcomes and mortality, with the hand grip strength and frailty being important emerging predictors in the most recent literature. These predictors would further inform healthcare providers of their patients’ health status and allow for early intervention for modifiable predictors.
Similar content being viewed by others
Introduction
Hip fracture is an important medical condition associated with adverse outcomes, including mortality [1]. The incidence of hip fractures is expected to increase due to ageing populations worldwide - there were 1.6 million hip fractures worldwide in year 2000 and this number is expected to increase to 4.5–6.3 million by 2050 according to International Osteoporosis Foundation [1, 2]. One-year mortality rate for patients with hip fracture was reported to be up to 20–24% and the mortality risk may persist beyond 5 years [3, 4]. As for functional outcomes, it was reported that 40% of hip fracture patients were unable to walk independently, 60% required assistance, and 33% were totally dependent or in a nursing home 1 year after hip fracture [3, 5, 6]. With increasing incidence and associated poor clinical outcomes, the impact of hip fractures on the healthcare system is significant.
Previous studies reported various predictors of adverse clinical outcomes for patients with hip fractures. A recent systematic review identified several predictors of mortality up to 12 months including cognitive impairment, age > 85 years and pre-fracture mobility [7]. However, it did not examine other important clinical outcomes other than mortality, especially functional ability. “Developing and maintaining the functional ability that enables well-being” has been the new vision of healthy ageing by World Health Organization [8]. Information about patient’s functional outcome is especially important given that the rapid ageing populations worldwide have resulted in increasing attention from researchers and policy makers to ageing related syndromes affecting patients’ functioning such as sarcopenia and frailty [9, 10].
It is well recognized that muscle function and physical performance are important clinical information that are relevant to patients’ functioning [11, 12]. A recent work by European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) working group on frailty and sarcopenia reviewed large number of approaches to measure muscle function and physical performance and recommended the use of grip strength to measure muscle strength and the use of 4-m gait speed or the Short Physical Performance Battery test to measure physical performance in daily practice [11]. In fact, grip strength has been the measure of choice for the assessment of overall muscle strength for the diagnosis of sarcopenia and frailty, as it has standardized, validated, easy to use protocols [13,14,15]. Given the rapid development and global emphasis on functional ability of the elderly, it is imperative to conduct an updated review on patients with hip fractures to include functional outcomes.
This review aims to summarize the existing literature on predictors of poor functional outcomes and mortality for patients with hip fractures. This would provide the latest evidence-based information that would assist healthcare providers to target modifiable predictors in order to reduce the incidence of poor outcomes.
Methods
Data sources and searches
We performed a systematic literature search for published literature in the past 15 years (from 1 Jan 2004 up to 30 May 2019) in three databases PubMed, EMBASE and Cochrane Library according to the Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA®) checklist. We chose to review the articles in the recent 15 years because by focusing on more recent data, we can summarize the evidence relevant to today’s medical practice. Hand search was also performed based on the references from the included studies.
Using the PubMed Advanced Search Builder, the following key search terms were used:
Critical Care Outcomes[Mesh] OR Patient Outcome Assessment[Mesh] OR Outcome Assessment (Health Care)[Mesh] OR Patient Reported Outcome Measures[Mesh] OR Fatal Outcome[Mesh] OR Treatment Outcome[Mesh] AND Hip Fractures[Mesh] AND predict*.
The detailed search strategy for the three databases can be found in Additional File 1.
Study selection
Two independent researchers evaluated the articles for eligibility through screening of the title and abstract first, followed by full text. Consensus on the eligibility of the articles was sought and the third researcher was involved if there was disagreement.
We included English peer-reviewed cohort studies that examined poor functional outcomes and mortality for patients with hip fracture published in the past 15 years (from 1 Jan 2004 up to 30 May 2019). Exclusion criteria were studies with inappropriate format (e.g. audit, self-administered survey, cross-sectional studies, systematic reviews, randomized controlled trials, case reports, and poster abstracts), and non-English articles.
Quality assessment
The Newcastle-Ottawa Scale (NOS) was used to assess the quality of cohort studies [16],
Results
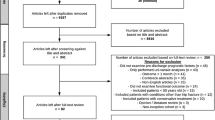
As shown in Fig. 1, 4339 articles were retrieved from the initial search process. One hundred twenty-four articles are potentially relevant for full text review after removing 67 duplicates and 4148 articles by title and abstract. Eighty-one articles were included in this article after full text review further excluded 43 articles. A summary of the included articles is presented in Additional file 1 [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97]. Predictors of poor functional outcomes and mortality for patients with hip fracture are grouped into medical, surgical, socio-economic and system factors. The excluded articles based on full text review are listed in Additional file 1.
Table 1 showed the predictors of poor functional outcomes. The medical predictors of poor functional outcomes include poor pre-fracture functional status, cognitive impairment, presence of multiple co-morbidities, high ASA grade, low hand grip strength, Body Mass Index (BMI), sarcopenia (as defined by The European Working Group on Sarcopenia in Older People Criteria [98]), frailty, depression, serum albumin and folic acid level, visual impairment, heart failure, hypercholesterolemia, osteoporotic treatment, osteoarthritis, pressure ulcers. The surgical predictors are extra-capsular fractures, delay in surgery for more than 48 h, associated dislocation and non-weight bearing status post-surgery. Older age, male gender, and place of residence are socio-economic predictors of poor functional outcomes. Process of care and length of stay are system predictors of poor functional outcomes.
Table 2 showed the predictors of mortality. The medical predictors of mortality are presence of multiple co-morbidities, high ASA grade, cognitive impairment, poor pre-fracture functional status, poor functional level at discharge, cardiac diseases, frailty, cancer, renal failure, cerebrovascular accident, diabetes, delirium, malnutrition, and low hemoglobin levels. The surgical predictors of mortality include delay in surgery for more than 48 h, extra-capsular fractures, perioperative fracture and non-operative management of hip fractures. Older age, male gender and being a resident in institutional care homes are socio-economic predictors of mortality. Lower case-volume centers (< 12 cases over 2 years), poor nurse staffing (low ratio of nurses to bed) and inappropriate prescription (medication prescriptions not consistent with clinical guidelines) were system predictors of mortality.
Discussion
This systematic review identified multiple predictors of poor functional outcomes and mortality for patients with hip fracture. Hand grip strength and frailty are two emerging predictors identified in this article. These two predictors were relatively new predictors identified in recent literature and were not found in the last major review [7]. Low hand grip strength was found to be a significant predictor of reduced gait speed and increased double support time [27]. Di Monaco M et al. reported a significant positive correlation between handgrip strength measured on admission to rehabilitation services and the Barthel Index scores assessed both on discharge from rehabilitation and at the 6-month follow-up [28]. The included studies analyzed hang grip strength as a continuous variable and did not specifically establish a threshold of absolute value above which the risk of poor functional outcome is higher. As for frailty, it is predictive of poorer basic ADL as well as 30-day mortality for hip fracture patients who underwent hip surgery [21, 52]. Krishnan M et al. reported that the 30-day mortality was 17.2% for patients of ‘high frailty’ (Frailty Index > 0.4), compared with 3.4% in ‘intermediate frailty’ patients (Frailty Index: 0.25–0.4) [58].
The above findings echoed with the emerging concept of “physical performance” as important functional capability measurement [11]. With an ageing population, frailty is becoming an important clinical syndrome resulting in poor functional outcomes, disability, and hospitalization [98, 99]. As there is increasing attention from researchers and policy makers on functional outcomes of patients, there is great interest in measuring and reporting them. However, various functional outcomes measures were used in the existing literature such as independence in mobility, FIM gain, Barthel Index efficacy, and EMS efficacy. Recent papers started to propose more specific and consistent methods to measure functional outcomes. For example, European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) working group on frailty and sarcopenia conducted comprehensive literature review and the experts panel recommended the use grip strength to measure muscle strength and 4-m gait speed or the Short Physical Performance Battery test to measure physical performance [11]. These recent developments would allow more standardized reporting of functional outcomes measured by validated, easy to use parameters in future medical literature.
The concept of physical performances has been changing over time. Previously, physical performances measures such as Timed-Get-Up-and-Go Test, Gait Speed Test and Modified Barthel Index were used as outcome measures under the domain of activity limitation [100]. ESCEO working group on frailty and sarcopenia now describes physical performance as a multidimensional concept where an objectively measured whole body function is related to the mobility of the individual [11]. In this recent review paper on the assessment of muscle function and physical performance in daily clinical practice by Charlotte Beaudart et al., a low grip strength is associated with poor outcomes and mortality [11]. Similarly, Robert D. Boutin et al. reported that CT findings of decreased thoracic paravertebral muscle size in older patients with hip fractures are associated with increased mortality [101]. While measurements of physical performance such as Gait Speed Test and Short Physical Performance Battery are strong predictors of loss of walking abilities and increased mortality, unfortunately such measurements may be biased in patients with hip fractures due to varying weight-bearing status.
This review found conflicting evidence for gender as a predictor of functional outcomes. Some studies reported that the female gender was a predictor of poorer functional outcomes as measured by ADLs [37] and EMS score [40]. Pajulammi HM et al. however concluded that the effect of gender on mobility recovery was minimal [25]. Kristensen MT et al. also reported that effect of gender on NMS was not significant [41]. However, female gender in other studies was found to be predictor of better functional outcomes as measured by early ambulation status [23], gait speed [27], and FIM gain [39, 45, 46]. This may be explained by the fact that the populations of these studies were heterogeneous. Future studies may focus on certain sub-populations to further elucidate the relationship between demographic factors and functional outcomes and mortality for patients with hip fracture.
With regard to the quality assessment of the included articles, the Newcastle-Ottawa Scale (NOS) was used to assess the quality of cohort studies. NOS covers three domains: selection of the cohorts, comparability of the cohorts, and assessment of the outcomes. Good quality studies are defined as those that achieve 3 or 4 stars in selection domain and 1 or 2 stars in comparability domain and 2 or 3 stars in outcome domain [16]. We used this scale because of it is easy to use and recommended by the Cochrane Collaboration [102, 103].
This review summarized and allows readers to have an oversight view of the predictors of poor functional outcomes and mortality for patients with hip fractures. Through identification of these predictors, healthcare providers would be better equipped to identify patients at risk of poor functional outcomes and/or death during their hospital admission. Healthcare providers can then tailor a patient-centered holistic care plan to assist patients to transit smoothly from the peri-operative period to the post-acute rehabilitation period. The post-acute care plan for these patients can also be tailored to facilitate better functional outcomes and lower mortality.
This paper has several limitations. Firstly, majority of the included articles were single-center observational studies, which are sensitive to selection bias and confounding factors. The number of good quality longitudinal cohort studies are sparse. Secondly, the measurements of the predictors are not standardized in different studies. For example, cognitive function is assessed by MMSE in most of the included studies but some used IQCODE, SPMSQ or cognitive FIM score. The inconsistencies in the instrument scales may have affected the sensitivity and specificity of the study in identifying the predictors. The search strategy of this article may also be further optimized by including more literature databases, non-English articles, and combining Mesh terms with free text keywords to further increase the comprehensiveness of the search strategy. Finally, the review protocol for this study was not registered.
Conclusion
This systematic review identified multiple predictors of poor functional outcomes and mortality for patients with hip fracture. Hand grip strength and frailty are two emerging ones. These predictors would further inform healthcare providers of their patients’ health status and allow for early intervention for modifiable predictors.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- ADL:
-
Activities of Daily Living
- ASA:
-
American Society of Anesthesiologists
- EMS:
-
Elderly Mobility scale
- FIM:
-
Functional Independence Measure
- IQCODE:
-
Informant Questionnaire on Cognitive Decline in the Elderly
- MMSE:
-
Mini-Mental State Examination
- NMS:
-
New Mobility Score
- ORs:
-
Odds Ratios
- POMA:
-
Performance-Oriented Mobility Assessment
- REFS:
-
Reported Edmonton Frail Scale
- SPMSQ:
-
Short Portable Mental State Questionnaire
References
Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407-13.
Cooper C, Campion G, Melton L3. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285-9.
Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton III LJ. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50(10):1644-50.
Magaziner J, Lydick E, Hawkes W, Fox KM, Zimmerman SI, Epstein RS, Hebel JR. Excess mortality attributable to hip fracture in white women aged 70 years and older. Am J Public Health. 1997;87(10):1630-6.
Riggs BL, Melton Iii LJ. The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone. 1995;17(5):S505-11.
Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol. 1990;45(3):M101-7.
Smith T, Pelpola K, Ball M, Ong A, Myint PK. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014;43(4):464-71.
World Health Organization. World report on ageing and health. World Health Organization; 2015.
Denison HJ, Cooper C, Sayer AA, Robinson SM. Prevention and optimal management of sarcopenia: a review of combined exercise and nutrition interventions to improve muscle outcomes in older people. Clin Interv Aging. 2015;10:859.
Clegg A, Rogers L, Young J. Diagnostic test accuracy of simple instruments for identifying frailty in community-dwelling older people: a systematic review. Age Ageing. 2015;44(1):148-52.
Beaudart C, Rolland Y, Cruz-Jentoft AJ, Bauer JM, Sieber C, Cooper C, Al-Daghri N, de Carvalho IA, Bautmans I, Bernabei R, Bruyère O. Assessment of muscle function and physical performance in daily clinical practice. Calcif Tissue Int. 2019:1-4.
National Collaborating Centre for Acute Care (UK. Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition; 2006.
Beaudart C, McCloskey E, Bruyère O, Cesari M, Rolland Y, Rizzoli R, de Carvalho IA, Thiyagarajan JA, Bautmans I, Bertière MC, Brandi ML. Sarcopenia in daily practice: assessment and management. BMC Geriatr. 2016;16(1):170.
Lauretani F, Russo CR, Bandinelli S, Bartali B, Cavazzini C, Di Iorio A, et al. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol. 2003;95(5):1851-60.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146-56.
Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2011.
McGilton KS, Chu CH, Naglie G, van Wyk PM, Stewart S, Davis AM. Factors influencing outcomes of older adults after undergoing rehabilitation for hip fracture. J Am Geriatr Soc. 2016;64(8):1601-9.
González-Montalvo JI, Alarcón T, Gotor P, Queipo R, Velasco R, Hoyos R, et al. Prevalence of sarcopenia in acute hip fracture patients and its influence on short-term clinical outcome. Geriatr Gerontol Int. 2016;16(9):1021-7.
Ariza-Vega P, Lozano-Lozano M, Olmedo-Requena R, Martín-Martín L, Jiménez-Moleón JJ. Influence of cognitive impairment on mobility recovery of patients with hip fracture. Am J Phys Med Rehabil. 2017;96(2):109-15.
Pedersen TJ, Lauritsen JM. Routine functional assessment for hip fracture patients: are there sufficient predictive properties for subgroup identification in treatment and rehabilitation? Acta Orthop. 2016;87(4):374-9.
Kua J, Ramason R, Rajamoney G, Chong MS. Which frailty measure is a good predictor of early post-operative complications in elderly hip fracture patients? Arch Orthop trauma Surg. 2016;136(5):639-47.
Cary MP, Pan W, Sloane R, Bettger JP, Hoenig H, Merwin EI, et al. Self-care and mobility following Postacute rehabilitation for older adults with hip fracture: a multilevel analysis. Arch Phys Med Rehabil. 2016;97(5):760-71.
Cohn MR, Cong G-T, Nwachukwu BU, Patt ML, Desai P, Zambrana L, et al. Factors Associated With Early Functional Outcome After Hip Fracture Surgery. Geriatr Orthop Surg Rehabil. 2016;7(1):3-8.
Mariconda M, Costa GG, Cerbasi S, Recano P, Orabona G, Gambacorta M, et al. Factors predicting mobility and the change in activities of daily living after hip fracture: a 1-year prospective cohort study. J Orthop Trauma. 2016;30(2):71-7.
Pajulammi HM, Pihlajamäki HK, Luukkaala TH. Nuotio MS. Pre- and perioperative predictors of changes in mobility and living arrangements after hip fracture-A population-based study. Arch Gerontol Geriatr. 2015;1;61(2):182-9.
Orive M, Anton-Ladislao A, García-Gutiérrez S, Las Hayas C, González N, Zabala J, et al. Prospective study of predictive factors of changes in pain and hip function after hip fracture among the elderly. Osteoporos Int. 2016;27(2):527-36.
Thingstad P, Egerton T, Ihlen EF, Taraldsen K, Moe-Nilssen R, Helbostad JL. Identification of gait domains and key gait variables following hip fracture. BMC Geriatr. 2015;15(1):150.
Di Monaco M, Castiglioni C, De Toma E, Gardin L, Giordano S, Tappero R. Handgrip strength is an independent predictor of functional outcome in hip-fracture women: A prospective study with 6-month follow-up. Medicine (United States). 2015;94(6).
Martín-Martín LM, Arroyo-Morales M, Sánchez-Cruz JJ, Valenza-Demet G, Valenza MC, Jiménez-Moleón JJ. Factors influencing performance-oriented mobility after hip fracture. J Aging Health. 2015;27(5):827-42.
Märdian S, Schaser KD, Gruner J, Scheel F, Perka C, Schwabe P. Adequate surgical treatment of periprosthetic femoral fractures following hip arthroplasty does not correlate with functional outcome and quality of life. Int Orthop. 2015;39(9):1701-8.
Uriz-Otano F, Uriz-Otano JI, Malafarina V. Factors associated with short-term functional recovery in elderly people with a hip fracture. Influence of cognitive impairment. J Am Med Dir Assoc. 2015;16(3):215-20.
Gialanella B, Ferlucci C, Monguzzi V, Prometti P. Determinants of outcome in hip fracture: role of daily living activities. Eur J Phys Rehabil Med. 2015;51(3):253-60.
Tan AKH, Taiju R, Menon EB, GCH K. Postoperated hip fracture rehabilitation effectiveness and efficiency in a community hospital. Ann Acad Med Singapore. 2014;43(4):209-15.
Ariza-Vega P, Jiménez-Moleón JJ, Kristensen MT. Non-weight-bearing status compromises the functional level up to 1 yr after hip fracture surgery. Am J Phys Med Rehabil. 2014;93(8):641-8.
Savino E, Martini E, Lauretani F, Pioli G, Zagatti AM, Frondini C, et al. Handgrip strength predicts persistent walking recovery after hip fracture surgery. Am J Med. 2013;126(12):1068-75.
Siebens HC, Sharkey P, Aronow HU, Horn SD, Munin MC, DeJong G, et al. Outcomes and weight-bearing status during rehabilitation after arthroplasty for hip fractures. PM R. 2012;4(8):548-55.
Sylliaas H, Thingstad P, Wyller TB, Helbostad J, Sletvold O, Bergland A. Prognostic factors for self-rated function and perceived health in patient living at home three months after a hip fracture. Disabil Rehabil. 2012;34(14):1225-31.
Kristensen MT, Kehlet H. Most patients regain prefracture basic mobility after hip fracture surgery in a fast-track programme. Dan Med J. 2012;59(6):A4447
Semel J, Gray JM, Ahn HJ, Nasr H, Chen JJ. Predictors of outcome following hip fracture rehabilitation. PM R. 2010;2(9):799-805.
Luk JKH, Chiu PKC, Tam S, Chu LW. Relationship between admission albumin levels and rehabilitation outcomes in older patients. Arch Gerontol Geriatr. 2011;53(1):84-9.
Kristensen MT, Foss NB, Ekdahl C, Kehlet H. Prefracture functional level evaluated by the New Mobility Score predicts in-hospital outcome after hip fracture surgery. Acta Orthop. 2010;81(3):296-302.
Shakouri SK, Eslamian F, Azari BK, Sadeghi-Bazargani H, Sadeghpour A, Salekzamani Y. Predictors of functional improvement among patients with hip fracture at a rehabilitation ward. Pakistan J Biol Sci. 2009;12(23):1516-20.
Feng L, Scherer SC, Tan BY, Chan G, Fong NP, Ng TP. Comorbid cognitive impairment and depression is a significant predictor of poor outcomes in hip fracture rehabilitation. Int Psychogeriatrics. 2010;22(2):246-53.
Chin RPH, Ng BHP, Cheung LPC. Factors predicting rehabilitation outcomes of elderly patients with hip fracture. Hong Kong Med J. 2008;14(3):209.
Mizrahi EH, Fleissig Y, Arad M, Blumstein T, Adunsky A. Rehabilitation outcome of hip fracture patients: the importance of a positive albumin gain. Arch Gerontol Geriatr. 2008;47(3):318-26.
Mizrahi EH, Fleissig Y, Arad M, Blumstein T, Adunsky A. Admission albumin levels and functional outcome of elderly hip fracture patients: is it that important? Aging Clin Exp res. 2007;19(4):284-9.
Press Y, Grinshpun Y, Berzak A, Friger M, Clarfield AM. The effect of co-morbidity on the rehabilitation process in elderly patients after hip fracture. Arch Gerontol Geriatr. 2007;45(3):281-94.
Rostagno C, Buzzi R, Campanacci D, Boccacini A, Cartei A, Virgili G, et al. In hospital and 3-month mortality and functional recovery rate in patients treated for hip fracture by a multidisciplinary team. PLoS One. 2016;11(7):e0158607.
Nuotio M, Tuominen P, Luukkaala T. Association of nutritional status as measured by the mini-nutritional assessment short form with changes in mobility, institutionalization and death after hip fracture. Eur J Clin Nutr. 2016;70(3):393.
Manoli A, Driesman A, Marwin RA, Konda S, Leucht P, Egol KA. Short-term outcomes following hip fractures in patients at least 100 years old. J Bone Joint Surg Am. 2017;99(13):e68.
Neuman MD, Silber JH, Passarella MR, Werner RM. Comparing the contributions of acute and postacute care facility characteristics to outcomes after hospitalization for hip fracture. Med Care. 2017;55(4):411.
Dayama A, Olorunfemi O, Greenbaum S, Stone ME, McNelis J. Impact of frailty on outcomes in geriatric femoral neck fracture management: an analysis of national surgical quality improvement program dataset. Int J Surg. 2016;28:185-90.
Ireland AW, Kelly PJ, Cumming RG. Risk factor profiles for early and delayed mortality after hip fracture: analyses of linked Australian Department of Veterans’ affairs databases. Injury. 2015;46(6):1028-35.
Neuman M, Silber J, Magaziner J, Passarella M, Mehta S, Werner R. Survival and functional outcomes after hip fracture among nursing home residents. JAMA Intern Med. 2014;174:1273–80.
Kau CY, EBK K. Can preoperative scoring systems be applied to Asian hip fracture populations? Validation of the Nottingham Hip Fracture Score (NHFS) and identification of preoperative risk factors in hip fractures. Ann Acad Med Singapore. 2014;43(9):448-53.
Gosch M, Wörtz M, Nicholas JA, Doshi HK, Kammerlander C, Lechleitner M. Inappropriate prescribing as a predictor for long-term mortality after hip fracture. Gerontology. 2014;60(2):114-22.
Belmont PJ, Garcia EJ, Romano D, Bader JO, Nelson KJ, Schoenfeld AJ. Risk factors for complications and in-hospital mortality following hip fractures: a study using the National Trauma Data Bank. Arch Orthop Trauma Surg. 2014;134(5):597-604.
Krishnan M, Beck S, Havelock W, Eeles E, Hubbard RE, Johansen A. Predicting outcome after hip fracture: using a frailty index to integrate comprehensive geriatric assessment results. Age Ageing. 2014;43(1):122-6.
Dailiana ZH, Papakostidou I, Varitimidis S, Michalitsis SG, Veloni A, Malizos KN. Surgical treatment of hip fractures: factors influencing mortality. Hippokratia. 2013;17(3):252.
Switzer JA, Bennett RE, Wright DM, Vang S, Anderson CP, Vlasak AJ, et al. Surgical time of day does not affect outcome following hip fracture fixation. Geriatr Orthop Surg Rehabil. 2013;4(4):109-16.
Griffiths EJ, Cash DJW, Kalra S, Hopgood PJ. Time to surgery and 30-day morbidity and mortality of periprosthetic hip fractures. Injury. 2013;44(12):1949-52.
Clement ND, Green K, Murray N, Duckworth AD, McQueen MM, Court-Brown CM. Undisplaced intracapsular hip fractures in the elderly: predicting fixation failure and mortality. A prospective study of 162 patients. J Orthop Sci. 2013;18(4):578-85.
Uzoigwe CE, Burnand HGF, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44(6):726-9.
Pioli G, Lauretani F, Davoli ML, Martini E, Frondini C, Pellicciotti F, et al. Older people with hip fracture and IADL disability require earlier surgery. J Gerontol Ser A Biol Sci Med Sci. 2012;67(11):1272-7.
Stewart NA, Chantrey J, Blankley SJ, Boulton C, Moran CG. Predictors of 5 year survival following hip fracture. Injury. 2011;42(11):1253-6.
Frost SA, Nguyen ND, Black DA, Eisman JA, Nguyen TV. Risk factors for in-hospital post-hip fracture mortality. Bone. 2011;49(3):553-8.
Adunsky A, Lerner-Geva L, Blumstein T, Boyko V, Mizrahi E, Arad M. Improved survival of hip fracture patients treated within a comprehensive geriatric hip fracture unit, compared with standard of care treatment. J Am Med Dir Assoc. 2011;12(6):439-44.
Talsnes O, Hjelmstedt F, Dahl OE, Pripp AH, Reikerås O. Clinical and biochemical prediction of early fatal outcome following hip fracture in the elderly. Int Orthop. 2011;35(6):903-7.
Hershkovitz A, Polatov I, Beloosesky Y, Brill S. Factors affecting mortality of frail hip-fractured elderly patients. Arch Gerontol Geriatr. 2010;51(2):113-6.
Björkelund KB, Hommel A, Thorngren KG, Lundberg D, Larsson S. Factors at admission associated with 4 months outcome in elderly patients with hip fracture. AANA J. 2009;77(1):49.
Burgos E, Gómez-Arnau JI, Díez R, Muñoz L, Fernández-Guisasola J, Garcia Del Valle S. Predictive value of six risk scores for outcome after surgical repair of hip fracture in elderly patients. Acta Anaesthesiol Scand. 2008;52(1):125-31.
Ercin E, Bilgili MG, Sari C, Basaran SH, Tanriverdi B, Edipoglu E, et al. Risk factors for mortality in geriatric hip fractures: a compressional study of different surgical procedures in 785 consecutive patients. Eur J Orthop Surg Traumatol. 2017;27(1):101-6.
Elkassabany NM, Passarella M, Mehta S, Liu J, Neuman MD. Hospital Characteristics, Inpatient Processes of Care, and Readmissions of Older Adults with Hip Fractures. J Am Geriatr Soc. 2016;64(8):1656-61.
Fields AC, Dieterich JD, Buterbaugh K, Moucha CS. Short-term complications in hip fracture surgery using spinal versus general anaesthesia. Injury. 2015;46(4):719-23.
Dubljanin-Raspopović E, Marković-Denić L, Marinković J, Nedeljković U, Bumbaširević M. Does early functional outcome predict 1-year mortality in elderly patients with hip fracture? Hip Clin Orthop Relat Res. 2013;471(8):2703-10.
Kim SM, Moon YW, Lim SJ, Yoon BK, Min YK, Lee DY, et al. Prediction of survival, second fracture, and functional recovery following the first hip fracture surgery in elderly patients. Bone. 2012;50(6):1343-50.
Dubljanin-Raspopović E, Denić LM, Marinković J, Grajić M, Vujadinović ST, Bumbaširević M. Use of early indicators in rehabilitation process to predict one-year mortality in elderly hip fracture patients. HIP Int. 2012;22(6):661-7.
Dubljanin-Raspopović E, Marković-Denić L, Matanović D, Grajić M, Krstić N, Bumbaširević M. Is pre-fracture functional status better than cognitive level in predicting short-term outcome of elderly hip fracture patients? Arch Med Sci. 2012;8(1):115.
Maggi S, Siviero P, Wetle T, Besdine RW, Saugo M, Crepaldi G. A multicenter survey on profile of care for hip fracture: predictors of mortality and disability. Osteoporos Int. 2010;21(2):223-31.
Siu AL, Boockvar KS, Penrod JD, Morrison RS, Halm EA, Litke A, et al. Effect of inpatient quality of care on functional outcomes in patients with hip fracture. Med Care. 2006;44(9):862.
Petersen MB, Jørgensen HL, Hansen K, Duus BR. Factors affecting postoperative mortality of patients with displaced femoral neck fracture. Injury. 2006;37(8):705-11.
Bokshan SL, Marcaccio SE, Blood TD, Hayda RA. Factors influencing survival following hip fracture among octogenarians and nonagenarians in the United States. Injury. 2018;49(3):685-90.
Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL. Functional outcomes and mortality vary among different types of hip fractures: a function of patient characteristics. Clin Orthop Relat Res. 2004;(425):64.
Lin PC, Chang SY. Functional recovery among elderly people one year after hip fracture surgery. J Nurs Res. 2004;12(1):72-82.
Di Monaco M, Castiglioni C, De Toma E, Gardin L, Giordano S, Di Monaco R, et al. Handgrip strength but not appendicular lean mass is an independent predictor of functional outcome in hip-fracture women: a short-term prospective study. Arch Phys Med Rehabil. 2014;95(9):1719-24.
Lieberman D, Friger M, Lieberman D. Inpatient rehabilitation outcome after hip fracture surgery in elderly patients: a prospective cohort study of 946 patients. Arch Phys Med Rehabil. 2006;87(2):167-71.
Nicholson JA, Scott CEH, Annan J, Ahmed I, Keating JF. Native hip dislocation at acetabular fracture predicts poor long-term outcome. Injury. 2018;49(10):1841-7.
González Quevedo D, Mariño IT, Sánchez Siles JM, Escribano ER, Granero Molina EJ, Enrique DB, et al. Patient survival and surgical re-intervention predictors for intracapsular hip fractures. Injury. 2017;48(8):1831-6.
Kagaya H, Takahashi H, Sugawara K, Dobashi M, Kiyokawa N, Ebina H. Predicting outcomes after hip fracture repair. Am J Phys Med Rehabil. 2005;84(1):46-51.
Gatot C, Chou ACC, Howe T Sen, yeo W, Chong HC, Koh JSB. Predictors for rehabilitation outcome in Asian geriatric hip fracture patients. J Orthop Surg. 2016;24(2):153-7.
Ganczak M, Chrobrowski K, Korzeń M. Predictors of a change and correlation in activities of daily living after hip fracture in elderly patients in a community hospital in Poland: a six-month prospective cohort study. Int J Environ Res Public Health. 2018;15(1):95.
Reuling EMBP, Sierevelt IN, Van Den Bekerom MPJ, Hilverdink EF, Schnater JM, Van Dijk CN, et al. Predictors of functional outcome following femoral neck fractures treated with an arthroplasty: limitations of the Harris hip score. Arch Orthop Trauma Surg. 2012;132(2):249-56.
Knauf T, Bücking B, Bargello M, Ploch S, Bliemel C, Knobe M, et al. Predictors of long-term survival after hip fractures?-5-year results of a prospective study in Germany. Arch Osteoporos. 2019;14;14(1):40. https://doi.org/10.1007/s11657-019-0586-1.
Makridis KG, Karachalios T, Kontogeorgakos VA, Badras LS, Malizos KN. The effect of osteoporotic treatment on the functional outcome, re-fracture rate, quality of life and mortality in patients with hip fractures: a prospective functional and clinical outcome study on 520 patients. Injury. 2015;46(2):378-83.
Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J, et al. The effect of perioperative anemia on clinical and functional outcomes in patients with hip fracture. J Orthop Trauma. 2004;18(6):369.
Söderqvist A, Miedel R, Ponzer S, Tidermark J. The influence of cognitive function on outcome after a hip fracture. J Bone Joint Surg Ser A. 2006;88(10):2115-23.
Boese CK, Buecking B, Schwarting T, Debus F, Ruchholtz S, Bliemel C, et al. The influence of pre-existing radiographic osteoarthritis on functional outcome after trochanteric fracture. Int Orthop. 2015;39(7):1405-10.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39:412-23.
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc. 2014;15(2):95-101.
Kostanjsek N. Use of The International Classification of Functioning, Disability and Health (ICF) as a conceptual framework and common language for disability statistics and health information systems. InBMC public health 2011 Dec (Vol. 11, No. 4, p. S3). BioMed Central.
Boutin RD, Bamrungchart S, Bateni CP, Beavers DP, Beavers KM, Meehan JP, et al. CT of patients with hip fracture: muscle size and attenuation help predict mortality. Am J Roentgenol. 2017;208(6):W208-15.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. Bmj. 2011;343:d5928.
Sanderson S, Tatt ID, Higgins JPT. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol. 2007;36(3):666-76.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
BYX conceptualized the study, devised the methodology and performed the literature review, wrote the first draft and revised subsequent revisions of the manuscript. SY, LLL, FFV, SGL reviewed the literature, critically revised the manuscript. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Search strategy and included/excluded articles.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xu, B.Y., Yan, S., Low, L.L. et al. Predictors of poor functional outcomes and mortality in patients with hip fracture: a systematic review. BMC Musculoskelet Disord 20, 568 (2019). https://doi.org/10.1186/s12891-019-2950-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-019-2950-0