Abstract
Purpose
Opioids are a mainstay for pain management after total joint arthroplasty (TJA). The prevalence and risk factors for prolonged opioid use after TJA are important to understand to help slow the opioid epidemic. We aim to summarize and evaluate the prevalence and time trend of prolonged opioid use after TJA and pool its risk factors.
Methods
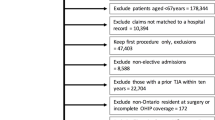
Following the preferred reporting items for systematic reviews and meta-analysis statement, we systematically searched PubMed, the Cochrane Library, and EMBASE, etc. from inception up to October 1, 2019. Cohort studies reporting risk factors for prolonged opioids use (≥ 3 months) after TJA were included. Studies characteristics, risk ratios (RR), and prevalence of prolonged opioid use were extracted and synthesized.
Results
A total of 15 studies were published between 2015 and 2019, with 416,321 patients included. 12% [95%CI 10–14%] of patients had prolonged opioid use after TJA and its time trend was associated with median enrollment years (P = 0.0013). Previous opioid use (RR = 1.73; P < 0.001), post-traumatic stress disorder (RR = 1.34; P < 0.001), benzodiazepine use (RR = 1.38; P < 0.001), tobacco abuse (RR = 1.26; P < 0.001), fibromyalgia (RR = 1.51; P < 0.001), and back pain (RR = 1.34; P < 0.001) were the largest effective risk factors for prolonged use of opioids.
Conclusions
To our knowledge, this is the first meta-analysis determining the risk factors of prolonged opioid use and characterizing its rate and time trend in TJA. Understanding risk factors for patients with higher potential for prolonged opioids use can be used to implement appropriate management strategies, reduce unsafe opioid prescriptions, and decrease the risk of prolonged opioid use after TJA.



Similar content being viewed by others
References
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L (2014) The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73(7):1323–1330. https://doi.org/10.1136/annrheumdis-2013-204763
Helmick CG, Felson DT, Lawrence RC, Gabriel S, Hirsch R, Kwoh CK, Liang MH, Kremers HM, Mayes MD, Merkel PA, Pillemer SR, Reveille JD, Stone JH (2008) Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum 58(1):15–25. https://doi.org/10.1002/art.23177
Kendrick BJ, Bottomley NJ, Gill HS, Jackson WF, Dodd CA, Price AJ, Murray DW (2012) A randomised controlled trial of cemented versus cementless fixation in Oxford unicompartmental knee replacement in the treatment of medial gonarthrosis using radiostereometric analysis. Osteoarthr Cartil 20:S36–S37. https://doi.org/10.1016/j.joca.2012.02.566
Health UDo, Services H (2018) HHS acting secretary declares public health emergency to address national opioid crisis. HHS gov https://www.hhsgov/about/news/2017/10/26/hhs-acting-secretary-declares-public-health-emergency-address-national-opioid-crisishtml. Published May 23
Sloan M, Premkumar A, Sheth NP (2018) Projected volume of primary total joint arthroplasty in the US, 2014 to 2030. J Bone Jt Surg Am 100(17):1455–1460. https://doi.org/10.2106/jbjs.17.01617
Vogt MT, Kwoh CK, Cope DK, Osial TA, Culyba M, Starz TW (2005) Analgesic usage for low back pain: impact on health care costs and service use. Spine 30(9):1075–1081. https://doi.org/10.1097/01.brs.0000160843.77091.07
Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P (2012) What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2(1):e000435. https://doi.org/10.1136/bmjopen-2011-000435
Hah JM, Sharifzadeh Y, Wang BM, Gillespie MJ, Goodman SB, Mackey SC, Carroll IR (2015) Factors associated with opioid use in a cohort of patients presenting for surgery. Pain Res Treat 2015:829696. https://doi.org/10.1155/2015/829696
Franklin PD, Karbassi JA, Li W, Yang W, Ayers DC (2010) Reduction in narcotic use after primary total knee arthroplasty and association with patient pain relief and satisfaction. J Arthroplasty 25(6 Suppl):12–16. https://doi.org/10.1016/j.arth.2010.05.003
Surgeons AAoO (2018) Information statement: opioid use, misuse, and abuse in orthopaedic practice. 2015. October https://www.aaos.org/uploadedFiles/PreProduction/About/Opinion_Statements/advistmt/1045%20Opioid%20Use,%20Misuse,%20and%20Abuse%20in%20Practice pdf. Accessed
Prentice HA, Inacio MCS, Singh A, Namba RS, Paxton EW (2019) Preoperative risk factors for opioid utilization after total hip arthroplasty. J Bone Jt Surg Am 101(18):1670–1678. https://doi.org/10.2106/jbjs.18.01005
Khazi ZM, Lu Y, Patel BH, Cancienne JM, Werner B, Forsythe B (2020) Risk factors for opioid use after total shoulder arthroplasty. J Shoulder Elbow Surg 29(2):235–243. https://doi.org/10.1016/j.jse.2019.06.020
Kim KY, Anoushiravani AA, Chen KK, Roof M, Long WJ, Schwarzkopf R (2018) Preoperative chronic opioid users in total knee arthroplasty-which patients persistently abuse opiates following surgery? J Arthroplasty 33(1):107–112. https://doi.org/10.1016/j.arth.2017.07.041
Namba RS, Singh A, Paxton EW, Inacio MCS (2018) patient factors associated with prolonged postoperative opioid use after total knee arthroplasty. J Arthroplasty 33(8):2449–2454. https://doi.org/10.1016/j.arth.2018.03.068
Rao AG, Chan PH, Prentice HA, Paxton EW, Navarro RA, Dillon MT, Singh A (2018) Risk factors for postoperative opioid use after elective shoulder arthroplasty. J Shoulder Elbow Surg 27(11):1960–1968. https://doi.org/10.1016/j.jse.2018.04.018
Politzer CS, Kildow BJ, Goltz DE, Green CL, Bolognesi MP, Seyler TM (2018) Trends in opioid utilization before and after total knee arthroplasty. J Arthroplast 33(7s):S147–S153.e141. https://doi.org/10.1016/j.arth.2017.10.060
Hadlandsmyth K, Vander Weg MW, McCoy KD, Mosher HJ, Vaughan-Sarrazin MS, Lund BC (2018) Risk for prolonged opioid use following total knee arthroplasty in veterans. J Arthroplast 33(1):119–123. https://doi.org/10.1016/j.arth.2017.08.022
Bedard NA, Pugely AJ, Dowdle SB, Duchman KR, Glass NA, Callaghan JJ (2017) Opioid use following total hip arthroplasty: trends and risk factors for prolonged use. J Arthroplast 32(12):3675–3679. https://doi.org/10.1016/j.arth.2017.08.010
Dwyer MK, Tumpowsky CM, Hiltz NL, Lee J, Healy WL, Bedair HS (2018) Characterization of post-operative opioid use following total joint arthroplasty. J Arthroplast 33(3):668–672. https://doi.org/10.1016/j.arth.2017.10.011
Bedard NA, Pugely AJ, Westermann RW, Duchman KR, Glass NA, Callaghan JJ (2017) Opioid use after total knee arthroplasty: trends and risk factors for prolonged use. J Arthroplast 32(8):2390–2394. https://doi.org/10.1016/j.arth.2017.03.014
Hansen CA, Inacio MCS, Pratt NL, Roughead EE, Graves SE (2017) Chronic use of opioids before and after total knee arthroplasty: a retrospective cohort study. J Arthroplast 32(3):811–817.e811. https://doi.org/10.1016/j.arth.2016.09.040
Sun EC, Bateman BT, Memtsoudis SG, Neuman MD, Mariano ER, Baker LC (2017) Lack of association between the use of nerve blockade and the risk of postoperative chronic opioid use among patients undergoing total knee arthroplasty: evidence from the marketscan database. Anesth Analg 125(3):999–1007. https://doi.org/10.1213/ane.0000000000001943
Inacio MC, Hansen C, Pratt NL, Graves SE, Roughead EE (2016) Risk factors for persistent and new chronic opioid use in patients undergoing total hip arthroplasty: a retrospective cohort study. BMJ Open 6(4):e010664. https://doi.org/10.1136/bmjopen-2015-010664
Goesling J, Moser SE, Zaidi B, Hassett AL, Hilliard P, Hallstrom B, Clauw DJ, Brummett CM (2016) Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain 157(6):1259–1265. https://doi.org/10.1097/j.pain.0000000000000516
Kim SC, Choudhry N, Franklin JM, Bykov K, Eikermann M, Lii J, Fischer MA, Bateman BT (2017) Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthr Cartil 25(9):1399–1406. https://doi.org/10.1016/j.joca.2017.04.002
Menendez ME, Ring D, Bateman BT (2015) Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res 473(7):2402–2412. https://doi.org/10.1007/s11999-015-4173-5
Morris BJ, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB (2015) Preoperative opioid use and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg 24(1):11–16. https://doi.org/10.1016/j.jse.2014.05.002
Mohamadi A, Chan JJ, Lian J, Wright CL, Marin AM, Rodriguez EK, von Keudell A, Nazarian A (2018) Risk factors and pooled rate of prolonged opioid use following trauma or surgery: a systematic review and meta-(regression) analysis. J Bone Jt Surg Am 100(15):1332–1340. https://doi.org/10.2106/jbjs.17.01239
Workman EA, Hubbard JR, Felker BL (2002) Comorbid psychiatric disorders and predictors of pain management program success in patients with chronic pain. Prim Care Companion J Clin Psychiatry 4(4):137–140. https://doi.org/10.4088/pcc.v04n0404
Eriksen WB, Brage S, Bruusgaard D (1997) Does smoking aggravate musculoskeletal pain? Scand J Rheumatol 26(1):49–54. https://doi.org/10.3109/03009749709065664
Nuesch E, Rutjes AW, Husni E, Welch V, Juni P (2009) Oral or transdermal opioids for osteoarthritis of the knee or hip. Cochrane Datab Syst Rev 4:Cd003115. https://doi.org/10.1002/14651858.CD003115.pub3
Smith SR, Deshpande BR, Collins JE, Katz JN, Losina E (2016) Comparative pain reduction of oral non-steroidal anti-inflammatory drugs and opioids for knee osteoarthritis: systematic analytic review. Osteoarthr Cartil 24(6):962–972. https://doi.org/10.1016/j.joca.2016.01.135
Funding
This study was supported through grants from the National Natural Science Foundation of China (81802210 and 81672219), National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University (Z20191008), the Key Project of Sichuan Science and Technology Department (2018SZ0223 and 2018SZ0250), and the National Clinical Research Center for Geriatrics, West China Hospital, Sichuan University (Z2018B20).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, L., Li, M., Zeng, Y. et al. Prevalence and risk factors for prolonged opioid use after total joint arthroplasty: a systematic review, meta-analysis, and meta-regression. Arch Orthop Trauma Surg 141, 907–915 (2021). https://doi.org/10.1007/s00402-020-03486-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03486-4