Abstract
Purpose
We performed a systematic review and meta-analysis with trial sequential analysis (TSA) to answer whether early closure of defunctioning ileostomy may be suitable after low anterior resection.
Methods
MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials were searched, up to October 2021, for RCTs comparing early closure (EC ≤ 30 days) and delayed closure (DC ≥ 60 days) of defunctioning ileostomy. The risk ratio (RR) with 95% CI was calculated for dichotomous variables and the mean difference (MD) with 95% CI for continuous variables. The GRADE methodology was implemented for assessing Quality of Evidence (QoE). TSA was implemented to address the risk of random error associated with sparse data and/or multiple testing.
Results
Seven RCTs were included for quantitative synthesis. 599 patients were allocated to either EC (n = 306) or DC (n = 293). EC was associated with a higher rate of wound complications compared to DC (RR 2.56; 95% CI 1.33 to 4.93; P = 0.005; I2 = 0%, QoE High), a lower incidence of postoperative small bowel obstruction (RR 0.46; 95% CI 0.24 to 0.89; P = 0.02; I2 = 0%, QoE moderate), and a lower rate of stoma-related complications (RR 0.26; 95% CI 0.16 to 0.42; P < 0.00001; I2 = 0%, QoE moderate). The rate of minor low anterior resection syndrome (LARS) (RR 1.13; 95% CI 0.55 to 2.33; P = 0.74; I2 = 0%, QoE low) and major LARS (RR 0.80; 95% CI 0.59 to 1.09; P = 0.16; I2 = 0%, QoE low) did not differ between the two groups. TSA demonstrated inconclusive evidence with insufficient sample sizes to detect the observed effects.
Conclusion
EC may confer some advantages compared with a DC. However, TSA advocated a cautious interpretation of the results.
Prospero Register ID
CRD42021276557
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Low anterior resection (LAR) with total mesorectal excision is considered the optimal surgical treatment for resectable primary rectal cancer [1, 2]. However, anastomotic leakage (AL) remains the most feared complication after LAR [3], with an incidence of 3 to 25% [4].
In order to protect the colorectal anastomosis and reduce the severity of pelvic sepsis associated with AL, a reversible faecal diversion through a temporary defunctioning ileostomy is usually fashioned during LAR [5,6,7,8,9], especially for patients at increased risk for AL, such as those with locally advanced tumours, located in the low rectum, and treated with neoadjuvant radiotherapy [10,11,12].
Defunctioning ileostomies are typically reversed after a time interval of 8–12 weeks, during which time 20 to 74% of patients will experience ileostomy-related complications [13,14,15,16].
As the incidence of stoma-related complications seems to increase with the time to ileostomy closure [17], it has been suggested that early ileostomy closure could reduce the length of exposure to stoma-related morbidity, improve quality of life, and reduce stoma-related costs, with no detriment to the integrity of the colorectal anastomosis [18,19,20].
Some recent meta-analyses have suggested that early ileostomy closure is effective and safe in selected patients [21,22,23,24]. However, others reported that early closure increased the rate of post-operative complications [25]. Similarly, several randomised controlled trials (RCTs) have reported promising results [18, 26,27,28,29], whereas other RCTs had to be prematurely terminated due to safety concerns [30, 31]. Over the last year, a new RCT has been published that has provided further evidence concerning the safety and feasibility of early closure of defunctioning ileostomy, which has not been included in any of the systematic reviews published to date [30].
Given the above, we decided to perform an updated systematic review and meta-analysis with trial sequential analysis (TSA) to answer whether early closure of temporary diverting ileostomy is suitable for selected patients without post-operative complications after LAR.
Material and methods
Study objective
We performed a systematic review and meta-analysis with TSA of RCTs with the aim to systematically review the currently available evidence on early defunctioning ileostomy closure (≤ 30 days after index operation, EC) in patients who underwent LAR for rectal cancer in terms of safety, long-term functional outcomes and costs, and to compare the above with delayed timing of ileostomy closure (> 60 days after index operation, DC) using the meta-analytic method and The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach [32].
This meta-analysis was conducted according to the recommendations of the 2020 updated Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) guidelines [33] and the Cochrane Handbook for Systematic Reviews of Interventions [34].
All stages of study identification, selection, quality assessment, and data extraction were performed independently by two reviewers (MP and AP). Inconsistencies were resolved through discussion between the two reviewers until a consensus was reached. This meta-analysis adheres to AMSTAR II criteria (A MeaSurement Tool to Assess Systematic Reviews) [35].
Inclusion and exclusion criteria
The clinical question according to the PICOS framework was:
-
(P) Population: patients with temporary defunctioning ileostomy after LAR for rectal cancer.
-
(I) Intervention: early ileostomy closure (EC); ≤ 30 days after ileostomy was performed.
-
(C) Comparison: delayed ileostomy closure (DC); ≥ 60 days after ileostomy was performed.
-
(O) Outcomes, as reported in the included studies: intraoperative and post-operative outcomes of safety and feasibility; functional outcomes; quality of life.
-
(S) Studies: RCTs comparing the two approaches.
The following studies were excluded: emergency ileostomy in case of AL, ileostomy performed during other types of surgery other than LAR for cancer, studies that involved paediatric patients (< 18 years of age), studies that included other types of enteral stomas such as colostomy, proximal/mid small bowel stomas, or where the type of stoma was not specified, systematic or narrative reviews, meta-analyses, abstracts, case reports, study protocols, non-human studies, non-comparative studies. In addition, studies in which closure time was influenced by factors (i.e. chemotherapy, the occurrence of complications after LAR, delays due to operating theatre unavailability) other than patient’s randomisation and allocation into a predefined study group were excluded.
Study identification
MEDLINE (via PubMed), EMBASE, and the Cochrane Central Register of Controlled Trials were systematically searched for any relevant human clinical study comparing EC and DC of defunctioning ileostomy after LAR for rectal cancer. Grey literature searches were conducted on ClinicalTrials.gov, Google Scholar, CORE, Grey Literature Report, and Open Grey. Reference lists of relevant studies were searched manually, and the “related articles” function in PubMed was used. In addition, the reference list from the selected articles was also scrutinised. The search strategy combined medical subject headings (MeSH) and keywords, using the terms of “Ileostomy”, “Defunctioning stoma”, “Early”, “Closure”, “Reversal”, “Proctectomy”, “Low Anterior Resection”, “Rectal Cancer”, and “Colorectal Cancer”. The detailed search strategy is accessible in the registered protocol (PROSPERO: CRD42021276557). No restrictions were placed on publication status or language. Full-text articles in languages other than English with a title/abstract indicating fulfilment of the eligibility criteria were translated electronically. Literature was searched from inception to October 31, 2021.
Study selection
The studies identified by the search strategy were subsequently selected based on title, abstract, and full-text review by two independent reviewers (MP and AP) in Rayyan web app for systematic reviews (https://www.rayyan.ai/).
RCTs comparing EC (Intervention) and DC (Control) as the most appropriate timing for ileostomy reversal after LAR for rectal cancer were included in the meta-analysis. Whenever there was an overlap in patient cohorts of two or more studies, and no difference in the study period was reported, the most recent report was included in the pooled analysis. Secondary analyses from the included RCTs were also included if they focused on outcomes other than those analysed in the primary study.
Data extraction
A double-blinded procedure was performed to increase the accuracy of the data extracted, which resulted in high and satisfactory inter-observer agreement (Kappa = 0.92).
The following individual data were independently extracted using standardised extraction forms (Excel 2019, Microsoft Corporation®). Demographic and baseline characteristics collected for each report included the following predefined data: (1) study identifier (first author, nationality, year of publication, clinical trials centres, study period, inclusion criteria, exclusion criteria, index operation, intervention, comparator, analysed outcomes, follow-up times); (2) baseline characteristics of the enrolled patients (sex, Age, BMI, comorbidities, type of surgery and technique of primary anastomosis construction, indication for colorectal resection, neoadjuvant therapy); (3) clinical outcomes (post-operative morbidity, mortality, leak of rectal or ileal anastomosis, unplanned reoperations, operative time, post-operative length of hospital stay, time to start chemotherapy); (4) morbidity outcomes analysis (Clavien-Dindo complications ≥ 3, post-operative ileus/small bowel obstruction, wound complications, post-operative intra-abdominal abscess, post-operative enterocutaneous fistula, bleeding, stoma-related complications, anastomotic stenosis, other medical complications, hospital readmission); (5) quality of life, functional outcomes, and costs (Gastrointestinal Quality of Life Index (GQLI), EORTC QLQ-C30 Quality of Life, low anterior resection syndrome, Memorial Sloan Kettering Cancer Centre Bowel Function Instrument).
Outcomes measures
The following primary outcomes were analysed:
-
Overall post-operative morbidity: defined as any complication occurring during the hospital stay, within 30 days, or 12 months after ileostomy closure.
The following secondary outcomes were analysed:
-
Morbidity outcomes stratified per different type of complication: leak of rectal anastomosis, leak of ileal anastomosis, Clavien-Dindo ≥ 3 complications, post-operative ileus/small bowel obstruction, wound complications, post-operative intra-abdominal abscess, post-operative enterocutaneous fistula, bleeding, stoma-related complications, anastomotic stenosis, other medical complications, hospital readmission, unplanned reoperations;
-
Functional outcomes: Low anterior resection syndrome (LARS), Memorial Sloan Kettering Cancer Centre Bowel Function Instrument (MSKCC-BFI);
-
Quality of life: Gastrointestinal Quality of Life Index (GQLI), EORTC QLQ-C30 Quality of Life;
-
Costs: Stoma-related costs, total costs;
-
Operative time;
-
Post-operative length of hospital stay;
-
Time to start chemotherapy.
Anastomotic leak was defined as any leak from the rectal anastomosis detected clinically and/or radiologically, including intra-abdominal abscess, enterocutaneous fistula, and anastomotic insufficiency [36]. Stoma-related complications were defined as the presence of any complications attributable to the presence of the ileostomy (i.e. dermatitis, parastomal infection, dehydration from high stoma output, renal insufficiency, stenosis, retraction, necrosis, prolapse, skin irritation, parastomal hernia) occurring between the index operation and stoma closure [37].
Statistical analysis
Variables for meta-analysis were considered if they were reported by at least two RCTs. All statistical analyses were performed using Reviewer Manager software (Reviewer Manager – RevMan – version 5.4.1, Sept. 2020, The Nordic Cochrane Centre, Cochrane Collaboration, www.training.cochrane.org) and RevMan Web 2020 [38]. The relative risk (RR) with 95% confidence interval (95% CI) was calculated for dichotomous variables and the mean difference (MD) with 95% CI for continuous variables. The point estimate of the RR value was considered statistically significant if the 95% CI did not cross the value at null hypothesis (RR = 1). The point estimate of the MD value was considered statistically significant if the 95% CI did not cross the value at null hypothesis (MD = 0). Statistical heterogeneity of the results across studies was assessed using the Higgins inconsistency index I2 and Chi-square test. A Chi-square test P < 0.10 and an I2 value of 50 to 90% were considered indicative of substantial heterogeneity. In addition to statistical heterogeneity, both clinical (variability in the baseline characteristics of the patients, interventions and outcomes studied) and methodological (variability in the study methods and risk of bias) heterogeneity were considered to inform the decision to use the fixed- or random-effects model. Fixed-effects model (Mantel–Haenszel) was used if substantial heterogeneity was absent, whereas a random-effects model was implemented for meta-analysis if substantial heterogeneity was found, according to the method of DerSimonian and Laird [39]. The analyses were performed using the Trial Sequential Analysis software version 0.9.5.10 Beta (The Copenhagen Trial Unit, Centre for Clinical Intervention Research, The Capital Region, Copenhagen University Hospital – Rigshospitalet, 2021).
Trial sequential analysis
The TSA was performed to address the risk of random error associated with sparse data and/or multiple testing which can affect cumulative meta-analysis analyses, and to assess whether further trials need to be conducted [40]. Indeed, the TSA can inform regarding how much more information is required to get a conclusive answer about the effect of the intervention versus its comparator and this is represented by the distance between the accrued information and the required information. We applied the TSA on the following patient-centred dichotomous outcomes, which are relevant for clinical practice due to their consequences for patient management, and are the most frequently reported in the literature: post-operative morbidity as the primary outcome, leak of rectal anastomosis, and unplanned reoperations as secondary outcomes.
We estimated the diversity-adjusted required information size (DARIS) based on the proportion of patients with an outcome in the control group, calculating the average control group event proportion, an alpha (type I error) of 5%, a beta (type II error) of 20%, and diversity model-based. Both the naïve and TSA-adjusted confidence intervals were reported. We set the conservative trial monitoring boundaries by Lan-DeMets-O’Brien-Fleming as the α-spending function [41, 42]. We calculated the cumulative Z-curve (the series of Z-statistics after each consecutive trial) of each cumulative meta-analysis and plotted it against the above monitoring boundaries according to the random-effects models. The crossing of the cumulative Z-curve into the trial sequential monitoring boundary for benefit indicates that a sufficient level of evidence has been reached, and no further trials may be needed to demonstrate the superiority of the intervention. Otherwise, when the cumulative Z-curve does not cross any of the trial sequential monitoring boundaries, there is likely insufficient evidence to reach a conclusion, and additional trials may be required [43].
We developed two scenarios according to two different risk ratio reduction (RRR) values. Scenario 1 was based on RRR values pragmatically chosen to represent a conservative intervention effect: 10% for post-operative morbidity outcome, 1% leak of rectal anastomosis, 5% unplanned reoperations [21,22,23,24,25, 44]. Scenario 2 represented a sensitivity analysis where an RRR of 25% was chosen to represent an optimistic intervention effect for all outcomes. The results are presented as the TSA figures with corresponding legends and interpretations.
Planned sensitivity and subgroup analyses
Sensitivity analyses of post-operative morbidity and other clinically relevant outcomes were performed, depending on:
-
The different primary bowel diseases (rectal cancer versus rectal cancer plus others);
-
Depending on some concerns of bias according to the ROB-2 evaluation.
Furthermore, given that substantial differences in clinical settings, especially regarding the timing of stoma closure within the EC group, the effect of the timing of EC for all outcomes was analysed by a subgroup analysis of very early closure (defined as closure ≤ 14 days), early closure (defined as closure between 15 and 30 days), in comparison with DC (defined as closure ≥ 60 days).
Risk of bias and quality of evidence assessment
The risk of bias of the included RCTs was independently assessed by two authors (MP and AP) using the Cochrane Risk of Bias Tool version 2 (RoB 2) [45]. In addition, the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology was implemented for assessing the quality of evidence (QoE) [46, 47], which was reported in the results with Summary of Findings Tables.
Results
Study selection
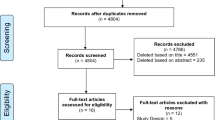
A total of 455 records were identified through database searching. Seven more references were identified by searching lists of retrieved studies. After removing 163 duplicates and four study protocols of ongoing studies, 288 records had their titles and abstracts evaluated. This resulted in 39 articles suitable for full-text review, where ten were retrospective studies, four were prospective non-randomised studies, eight included colostomy closure procedures, five had no comparative cohort, and one did not focus on the selected outcomes of interest. Finally, 11 RCTs were included for quantitative synthesis, of which seven were primary studies [18, 26,27,28,29,30,31] and four were secondary analyses of the primary RCTs [48,49,50,51] (Table 1). In total, 599 patients were allocated to either Early ileostomy closure (EC) (n = 306) or Delayed ileostomy closure (DC) (n = 293). General patient characteristics of the patients as reported in the studies are shown in Supplementary Table 1. Supplementary Table 2 shows the evidence report of each included study. Figure 1 reports the flow diagram of the study selection phases and reported excluded reasons for full texts not being eligible.
Study characteristics
Considerable variability was found among the included studies concerning the definition and the time frame of EC and DC. Some studies defined EC as the closure of the stoma within 8 days after LAR [18, 26], whereas in others, patients allocated to EC had their ileostomy closed within 2 weeks of LAR [27, 28]. Delay until stoma closure in the EC group was 17 days in the study by Klek et al. [29] and 15 days in the study by Elsner et al. [30]. Finally, in the study by Bausys et al. patients in the EC group had undergone stoma closure 30 days after creation [31]. Significant heterogeneity also existed in terms of delay until ileostomy closure in the DC group, with timing for closure that varied between 57 [26] and 278 days [29] after stoma creation. Most studies included patients with rectal cancer as the sole indication for LAR. Two studies [18, 26] included benign, borderline, and inflammatory bowel diseases. Different follow-up times were reported, ranging from 30 days [31] to 12 months [18, 27]. Two RCTs were prematurely terminated for safety reasons [30, 31].
Primary outcome: Overall post-operative morbidity
No statistically significant difference was found between the two groups in terms of overall postoperative morbidity (7 studies, 599 patients; RR 0.99, 95% CI 0.78 to 1.78; P = 0.95; I2 = 37%, fixed-effects; QoE low; test for subgroup differences: Chi2 = 5.59, P = 0.02, I2 = 82.1%) (Fig. 2) (Supplementary Table 3).
Secondary outcomes: Morbidity outcomes stratified per different types of complication
EC and DC showed equivalent results in terms of leak of the rectal anastomosis (7 studies, 599 patients; RR 1.04; 95% CI 0.46 to 2.36; P = 0.92; I2 = 0%, Fixed-effects; QoE low; test for subgroup differences: Chi2 = 2.63, P = 0.11, I2 = 61.9%) (Fig. 3), leak of the ileal anastomosis (6 studies, 413 patients; RR 4.52; 95% CI 0.54 to 37.78; P = 0.16; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: not applicable), unplanned reoperation (7 studies, 599 patients; RR 1.60; 95% CI 0.84 to 3.06; P = 0.15; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: Chi2 = 2.19, P = 0.14, I2 = 54.4%), Clavien-Dindo ≥ 3 complications (5 studies, 387 patients; RR 1.74; 95% CI 0.39 to 7.72; P = 0.46; I2 = 59%, random-effects; QoE low; test for subgroup differences: Chi2 = 5.81, P = 0.02, I2 = 82.8%) (Fig. 3), postoperative intra-abdominal abscess (6 studies, 543 patients; RR 1.32; 95% CI 0.44 to 3.92; P = 0.62; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: Chi2 = 1.37, P = 0.24, I2 = 27.2%), postoperative enterocutaneous fistula (3 studies, 338 patients; RR 4.06; 95% CI 0.70 to 23.51; P = 0.12; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: Chi2 = 0.09, P = 0.76, I2 = 0%), postoperative bleeding (6 studies, 534 patients; RR 0.59; 95% CI 0.08 to 4.38; P = 0.60; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: Chi2 = 0.24, P = 0.62, I2 = 0%), anastomotic stenosis (6 studies, 534 patients; RR 1.49; 95% CI 0.25 to 9.01; P = 0.66; I2 = 28%, fixed-effects; QoE low; test for subgroup differences: not applicable), other medical complications (6 studies, 534 patients; RR 1.42; 95% CI 0.69 to 2.93; P = 0.34; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: Chi2 = 0.30, P = 0.59, I2 = 0%), and hospital readmission (2 studies, 152 patients; RR 1.36; 95% CI 0.40 to 4.63; P = 0.62; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: not applicable).
EC was associated with a higher rate of wound complications compared to DC (6 studies, 534 patients; RR 2.56; 95% CI 1.33 to 4.93; P = 0.005; I2 = 0%, fixed-effects; QoE high; test for subgroup differences: Chi2 = 1.67, P = 0.20, I2 = 40.2%) (Fig. 4), a lower incidence of postoperative small bowel obstruction (7 studies, 599 patients; RR 0.46; 95% CI 0.24 to 0.89; P = 0.02; I2 = 0%, fixed-effects; QoE moderate; test for subgroup differences: Chi2 = 3.08, P = 0.08, I2 = 67.6%) (Fig. 5), and a lower rate of stoma-related complications (5 studies, 453 patients; RR 0.26; 95% CI 0.16 to 0.42; P < 0.00001; I2 = 0%, fixed-effects; QoE moderate; test for subgroup differences: Chi2 = 0.05, P = 0.82, I2 = 0%) (Fig. 4) (Supplementary Table 4).
Secondary outcomes: Quality of life and functional outcomes
EC and DC showed equivalent functional outcomes in terms of quality of life, calculated with the GQLI (2 studies, 257 patients; MD 1.22; 95% CI − 2.80 to 5.24; P = 0.55; I2 = 44%, fixed-effects; QoE low; test for subgroup differences: not applicable) and with the EORTC QLQ-C30 Quality of Life (2 studies, 148 patients; MD 0.23; 95% CI − 3.01 to 3.48; P = 0.89; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: not applicable). The pooled analyses showed that the rates of minor LARS (2 studies, 133 patients; RR 1.13; 95% CI 0.55 to 2.33; P = 0.74; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: not applicable) and major LARS (2 studies, 133 patients; RR 0.80; 95% CI 0.59 to 1.09; P = 0.16; I2 = 0%, fixed-effects; QoE low; test for subgroup differences: not applicable) did not differ between the two groups (Fig. 6) (Supplementary Table 5).
Secondary outcomes: Operative time and post-operative length of hospital stay
Operative time in the EC group ranged between 20 (median, IQR 13) [26] and 130 min (median, range 60 − 240) [30], compared with 40 (median, IQR 9) [26] to 110 min (median, range 60 − 257) [30] in the DC group. Overall length of hospital stay in the EC group ranged between 14 (median, range 11 − 42) [27] and 28 days (median, range 17 − 77) [30], compared with 14 (median, range 7 − 44) [27] to 27 days (median, range 17 − 87) [30] in the DC group. Length of hospital stay after ileostomy closure showed wide variability, ranging between 4 (median, range 2 − 27) [27] and 7 days (median, range 6 − 9) [31] in the EC group and 4 (median, range 2 − 21) [28] to 6 days (median, range 6 − 7) [31] in the DC group (Supplementary Table 3). Quantitative synthesis was not performed for either operative time or length of hospital stay due to the lack of data reported as mean and standard deviation. The Hozo method to convert median and range into mean and standard deviation [52] was not used as the data distribution in the primary RCTs might be skewed, so the approach mentioned above may not be appropriate [34].
Secondary outcomes: Costs
Costs were evaluated by Lasithiotakis et al. [26], Klek et al. [29], and Park et al. [49]. However, quantitative synthesis was not performed due to the high methodological heterogeneity regarding outcome metrics and settings.
The study by Lasithiotakis et al. showed that EC was superior compared to DC in terms of costs of stoma care (27 £ median, 9 IQR versus 311 £ median, 108 IQR). In the study by Park et al. the difference in mean cost per patient was $4060 in favour of EC. Taking protocol-driven examinations into account, the sensitivity analysis resulted in an overall difference in mean cost per patient of $3608 in favour of EC. Similarly, in the study by Klek et al., a health care cost reduction in favour of EC was demonstrated: 152.9 ± 16.3 versus 2413.1 ± 759 (cost of stoma bags/treatment period) (Supplementary Table 5).
Secondary outcomes: Time to start chemotherapy
Time to start chemoradiotherapy was analysed by Klek et al. [29]. Mean time to start adjuvant treatment was 38.7 ± 5.7 and 33.2 ± 5.8 days in the EC and DC groups, respectively (P < 0.001) (Supplementary Table 3).
Subgroup analyses
Two subgroup meta-analyses (very early closure, defined as closure 8 − 14 days, and early closure, defined as closure between 15 and 30 days) showed that the rate of post-operative morbidity was slightly higher in the early closure group compared to the DC group (RR 1.60; 95% CI 0.99 to 2.58; P = 0.05; I2 = 35%, fixed-effects), although without statistical significance. Similarly, the unplanned reoperation rate showed an increased rate in the early closure group compared to the DC (RR 4.19; 95% CI 0.91 to 19.30; P = 0.07; I2 = 0% fixed-effects). The rate of Clavien-Dindo ≥ 3 complications was lower in the very early closure group compared to the DC group (RR 0.57; 95% CI 0.34 to 0.97; P = 0.04; I2 = 0%, fixed-effects), whereas the rate of wound complication was comparable between the early closure group and the DC group (RR 1.45; 95% CI 0.51 to 4.15; P = 0.48; I2 = 0%, Fixed-effects).
Sensitivity analyses
Sensitivity analyses excluding the RCTs by Lasithiotakis et al. [26] and Alves et al. [18] that also included patients with benign disease in the study population found an equivalent rate of post-operative small bowel obstruction comparing the very early closure (8 − 14 days) and the DC groups (RR 0.64; 95% CI 0.09 to 4.76; P = 0.66; I2 = 0%, fixed-effects). Sensitivity analyses excluding studies with some concerns of bias according to the ROB-2 evaluation found similar outcomes between the EC and DC groups in terms of overall post-operative morbidity, although in the subgroup comparison between the early closure group (15 − 30 days) and the DC group a statistically significant difference was found in favour of DC (RR 1.82; 95% CI 1.08 to 3.04; P = 0.02; I2 = 53%, random-effects). Equivalent outcomes were also found regarding the leak of rectal anastomosis and unplanned reoperation. Wound complication rate was higher in the EC compared to the DC group (4 studies, 450 patients; RR 3.20; 95% CI 1.50 to 6.86; P = 0.003; I2 = 0%, fixed-effects; test for subgroup differences: Chi2 = 0.24, P = 0.62, I2 = 0%), with the majority of wound complications occurring in the very early closure group (8 − 14 days) (RR 3.60; 95% CI 1.46 to 8.89; P = 0.005; I2 = 0%, fixed-effects). The rate of small bowel obstruction remained lower in the EC compared to the DC group (4 studies, 450 patients; RR 0.41; 95% CI 0.20 to 0.84; P = 0.01; I2 = 13%, fixed-effects; test for subgroup differences: Chi2 = 2.37, P = 0.12, I2 = 57.9%), with a greater effect in favour of the very early closure group (8 − 14 days) (RR 0.24; 95% CI 0.08 to 0.70; P = 0.009; I2 = 18%, fixed-effects).
Trial sequential analysis
For post-operative morbidity, scenario 1, using an RRR of 10% and a control event rate of 29.7%, we obtained a DARIS (Diversity Adjusted Required Information Size) of 16,330 patients. The cumulative Z-curve did not surpass either the traditional monitoring boundary or the trial sequential monitoring boundaries. TSA graph was not available due to insufficient information use (3.67%). Using an RRR of 25%, scenario 2, we obtained a DARIS of 2478 patients: the cumulative Z-curve did not surpass either the traditional monitoring boundary or the trial sequential monitoring boundaries with an alpha-spending adjusted CI of 0.61–1.63.
For leak of rectal anastomosis, scenario 1, using an RRR of 1% and a control event rate of 3%, we obtained a DARIS of 10,102,024 patients. The cumulative Z-curve did not surpass either the traditional or the trial sequential monitoring boundaries. Using an RRR of 25% and a control event rate of 3%, scenario 2, we obtained a DARIS of 14,267 patients: the cumulative Z-curve did not surpass either the traditional or the trial sequential monitoring boundaries. TSA graphs were unavailable for both scenarios due to insufficient information use (< 4%).
For unplanned reoperations, scenario 1, using an RRR of 5% and a control event rate of 4%, we obtained a DARIS of 294,169 patients. The cumulative Z-curve did not surpass either the traditional or the trial sequential monitoring boundaries. TSA graph was not available due to little information use (0.19%). Using an RRR of 25% and a control event rate of 4%, scenario 2, we obtained a DARIS of 10,604 patients: the cumulative Z-curve did not surpass either the traditional or the trial sequential monitoring boundaries with an alpha-spending adjusted CI of 0.11–22.54 (Fig. 7) (Supplementary Table 6).
Risk of bias and certainty of the evidence assessment
The quality of the seven included primary RCTs was evaluated according to the Cochrane Risk of Bias Tool (RoB) version 2 (Fig. 8). Four RCTs were considered at low risk of bias [18, 27, 30, 31], whereas three RCTs contained some concerns [26, 28, 29] (Supplementary Table 1). According to the GRADE criteria, the overall QoE was high only for wound complications. It was moderate for post-operative ileus/small bowel obstruction and stoma-related complication but low for post-operative morbidity, leak of rectal anastomosis, unplanned reoperation, and Clavien-Dindo complication ≥ 3 (Fig. 9). Potential publication bias was present for Clavien-Dindo complication ≥ 3. Funnel plots have been provided as supplemental digital content (Supp. Digit. Content Fig. 1).
Discussion
In keeping with previous studies, the current meta-analysis with TSA of RCTs, including data of 599 patients, indicates that patients who had undergone early ileostomy closure within 30 days from LAR for rectal cancer experienced lower occurrence of small bowel obstruction and stoma-related complication but, at the same time, incur a higher rate of ileostomy closure-related wound complications [21,22,23,24,25]. Wound complications after ileostomy closure can be decreased by the implementation of evidence-based recommendations on closure techniques. As reported in the Italian guidelines for the surgical management of enteral stomas in adults, purse-string closure in stoma reversal should be the preferred skin closure technique because it is associated with lower surgical site infection rates compared to other techniques [53]. All patients undergoing enterostomy closure should receive antibiotic prophylaxis. Although various regimens have been described, oral preoperative antibiotics appear to be associated with less morbidity than parenteral antibiotics, similar to findings already reported for colon surgery [54].
Based on the primary pooled analysis, the incidence of post-operative morbidity was similar for patients who underwent early and delayed ileostomy closure ≥ 60 days from LAR. However, the sensitivity analysis that excluded the study by Alves et al. suggested that the higher rate of wound complications in the early closure group was mainly attributable to a closure strategy within 8 days of the primary resection [18].
The subgroup meta-analyses on very early closure (closure 8–14 days) and early closure (closure between 15 and 30 days) showed that the rate of post-operative morbidity was lower if stoma closure was performed between the 8th and the 14th post-operative day after the primary LAR. In contrast, patients who underwent stoma closure between the 15th and the 30th day were exposed to 60% increased risk of post-operative complications compared to the delayed closure. Furthermore, patients in the early ileostomy closure group had 4.2 times increased risk of a second, unplanned reoperation and a 4.6 times increased risk of a Clavien-Dindo ≥ 3 complication compared to the delayed closure group.
In synthesis, our findings suggest that the ideal timing for ileostomy closure should be approximately between days 8 and 14 after construction, provided that a satisfactory CT scan-assessed gastrografin enema or a flexible endoscopy, or both, demonstrates no signs of anastomotic insufficiency. This is based on two primary considerations: the first is that the tensile strength of an anastomosis has been shown to rapidly increase at day 5 and to exceed its initial strength at day 7, and by this time, the vast majority of anastomotic leaks will have occurred [19, 55]. The second is that severe dense adhesions around the ileostomy site tend to form after 2 weeks and up to 6 weeks post-operation [56].
LARS is pragmatically defined as disordered bowel function leading to a detriment in quality of life after rectal resection, which encompasses the vital aspects of the patient experience [57]. The risk of developing major LARS seems higher with a defunctioning ileostomy, and a prolonged time to ileostomy closure seems to reinforce the negative effect on bowel function, suggesting that early reversal should be an essential part of the patient pathway [58]. Similarly, a sub-analysis of the EASY trial showed that patients undergoing early ileostomy closure had fewer problems with soiling and fewer had a permanent stoma [50]. Regarding the analysis of functional outcomes, our meta-analysis did not show any advantages for the early ileostomy closure group in terms of quality of life and incidence of LARS. However, our findings may be hampered by small sample sizes and a high risk of imprecision.
Two years of COVID-19 pandemic have dramatically modified the usual clinical practice. Some scientific surgical societies have recommended a prudent approach towards colorectal anastomosis [59, 60]. The majority of surgical procedures have been performed for emergent or oncological reasons to the detriment of the remaining elective procedures for benign conditions. The pandemic may have caused a delay in enterostomy closure, especially in cases of patients who are candidates for adjuvant chemotherapy, with a prolonged deterioration in quality of life, an increase in number of enterostomies that will never be closed, and increased associated health care costs for the management of this new patient cohort. In this regard, a same-admission ileostomy closure strategy in selected patients [18, 26] can contribute on the one hand to reducing the burden on hospitals caused by new hospitalizations due to the presence of ileostomy-related complications, and on the other hand to guarantee a better quality of life for the patient. Also, ghost ileostomy may be a safe and cost-effective method in patients who underwent LAR with low or medium risk factors for AL [61].
A recent meta-analysis with TSA provided “firm evidence the early closure of ileostomy reduced the incidence of small bowel obstruction and post-operative ileus and required less total operative time, but increased the incidence of surgical site infections compared with late closure of ileostomy” [22]. Though in keeping with the results of the meta-analysis by Cheng et al., our TSA was not able to reach any firm conclusion on either of the two scenarios according to different RRR: the one that represented a conservative and more realistic intervention effect and the one that represented a sensitivity analysis where an RRR of 25% was chosen to represent an optimistic intervention effect for all outcomes.
The current literature has substantial limitations, especially concerning multiple studies with small sample sizes, as highlighted in our TSA. In contrast to other systematic reviews and meta-analyses that provided more optimistic conclusions about the feasibility, efficacy, and safety of early closure of defunctioning ileostomies in selected patients without taking into account the high risk of imprecision and all the risks of drawing firm evidence based on small sample sizes [23], we are more conservative with our conclusions. Even though our results do affirm the view that early ileostomy closure is a valid option, they should be interpreted with caution. In fact, according to the GRADE criteria, the overall quality of evidence was moderate to low for outcomes classified as “critical” in the preplanned analysis.
Further limitations of the present meta-analysis relate to relatively high inter-study heterogeneity for some of the analysed outcomes that required exploration of potential sources. The timing of intervention differed substantially in the study by Bausys et al. [31], where the median time to early ileostomy closure after LAR was 34 days and more than 3 weeks later than the studies by Alves et al. and Lasithiotakis et al. [18, 26]. In the study by Bausys et al. which was prematurely terminated due to a high rate of post-operative morbidity in the early closure group, the authors argue that the high complication rate could be due to a greater technical difficulty of ileostomy closure at day 30, when adhesions have formed, and the inflammatory phase of cicatrisation is still active.
In order to address heterogeneity, we performed several subgroup analyses for very early ileostomy closure and two different sensitivity analyses. Sensitivity analyses excluding studies with some bias concerns according to the ROB-2 evaluation found similar outcomes between the two groups in terms of post-operative morbidity, leak of rectal anastomosis, and unplanned reoperation. Finally, although the concept of late anastomotic leak is still a matter of debate [5, 62], delayed leak of the colorectal anastomosis may occur after the eighth post-operative day despite a negative contrast enema examination or endoscopy. For this reason, we have investigated this specific outcome by excluding the studies by Alves et al. [18] and Lasithiotakis et al. [26] in which the ileostomy was closed between the 7th and the 8th post-operative days in the early closure group, with the result that no difference was found between the two groups in terms of colorectal anastomotic leak.
Several large randomised trials have assessed the outcomes of laparoscopic colectomy compared to conventional open surgery [63,64,65,66]. The widespread implementation of laparoscopic surgery in colorectal cancer has been associated with improved postoperative clinical outcomes, including lower blood loss and less postoperative pain, as well as fewer abdominal wall complications, without negatively affecting the oncological outcomes. Conversely, robust evidence on minimally invasive LAR remains lacking [67,68,69]. Appropriately in light of this, another potential limitation of our study is the lack of information on the type of surgical approach used for the rectal resection. This might have an impact on the results because, after minimal access surgery, it can be expected that adhesions around the ileostomy are less even in the early period after surgery.
This meta-analysis also has significant strengths. It only included RCTs, increasing the likelihood that estimated effects favouring early ileostomy closure for selected patients with an uneventful recovery from the rectal resection may be investigated safely in the future.
Besides the high risk of imprecision, our results should be interpreted with caution, as the patients randomized to early ileostomy closure were selected based on a set of strict criteria where the patients have a low prevalence of coexisting morbidity and have an uneventful post-operative course after rectal resection. Unfortunately, despite the completeness of the analysis, numerous doubts remain, which will be clarified by future studies with a high level of evidence. Should it be decided to transfer our results into daily clinical practice, maximum attention should be paid to carefully select patients, both regarding the general clinical status and the effective healing of the colorectal anastomosis.
Conclusions
Findings of this meta-analysis with TSA indicate that a narrow window of chance for early closure might exist between the 8th and the 14th post-operative days following LAR.
Preliminary results suggest that very early closure in selected patients is feasible in the absence of radiological or endoscopic signs of anastomotic insufficiency, and may confer some advantages compared with delayed closure after 2 months. The results of our TSA should be interpreted with caution, especially in terms of leak of the colorectal anastomosis, post-operative morbidity, and unplanned reoperations. Therefore, future research should be conducted in the context of randomized controlled trials to determine the effectiveness of early ileostomy closure definitively.
Trial sequential analysis of A post-operative morbidity (scenario 2): trial sequential analysis of EC vs DC for post-operative morbidity. The diversity adjusted information size (DARIS) was calculated based on a control event proportion of 29.7%, a relative risk reduction (RRR) of 25%, an alpha (a) of 0.05, a beta (b) of 0.20, and diversity D of 55.85. B Unplanned reoperation (scenario 2): trial sequential analysis of EC vs DC for unplanned reoperation. The diversity adjusted information size (DARIS) was calculated based on a control event proportion of 4%, a relative risk reduction (RRR) of 25%, an alpha (a) of 0.05, a beta (b) of 0.20, and diversity D of 0
Data availability
Template data collection forms, data extracted from included studies, data used for all meta-analyses and trial sequential analysis, and any other materials used in the present research are available on request from the corresponding author (MP).
References
Hughes DL, Cornish J, Morris C, LARRIS Trial Management Group (2017) Functional outcome following rectal surgery-predisposing factors for low anterior resection syndrome. Int J Colorectal Dis 32:691–697. https://doi.org/10.1007/s00384-017-2765-0
Heald RJ (1995) Total mesorectal excision is optimal surgery for rectal cancer: a Scandinavian consensus. Br J Surg 82:1297–1299. https://doi.org/10.1002/bjs.1800821002
Podda M, Di Saverio S, Davies RJ, Atzeni J, Balestra F, Virdis F, Reccia I, Jayant K, Agresta F, Pisanu A (2020) Prophylactic intra-abdominal drainage following colorectal anastomoses. A systematic review and meta-analysis of randomised controlled trials. Am J Surg 219:164–174. https://doi.org/10.1016/j.amjsurg.2019.05.006
Snijders HS, Wouters MW, van Leersum NJ, Kolfschoten NE, Henneman D, de Vries AC, Tollenaar RA, Bonsing BA (2012) Meta-analysis of the risk for anastomotic leakage, the postoperative mortality caused by leakage in relation to the overall postoperative mortality. Eur J Surg Oncol 38:1013–1019. https://doi.org/10.1016/j.ejso.2012.07.111
Sparreboom CL, van Groningen JT, Lingsma HF, Wouters MWJM, Menon AG, Kleinrensink GJ, Jeekel J, Lange JF, Audit DC, group, (2018) Different risk factors for early and late colorectal anastomotic leakage in a nationwide audit. Dis Colon Rectum 61:1258–1266. https://doi.org/10.1097/DCR.0000000000001202
Marusch F, Koch A, Schmidt U, Geibetaler S, Dralle H, Saeger HD, Wolff S, Nestler G, Pross M, Gastinger I, Lippert H (2002) Value of a protective stoma in low anterior resections for rectal cancer. Dis Colon Rectum 45:1164–1171. https://doi.org/10.1007/s10350-004-6384-9
Tan WS, Tang CL, Shi L, Eu KW (2009) Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg 96:462–472. https://doi.org/10.1002/bjs.6594
Montedori A, Cirocchi R, Farinella E, Sciannameo F, Abraha I (2010) Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev 12(5):CD006878. https://doi.org/10.1002/14651858.CD006878.pub2
Lu ZR, Rajendran N, Lynch AC, Heriot AG, Warrier SK (2016) Anastomotic leaks after restorative resections for rectal cancer compromise cancer outcomes and survival. Dis Colon Rectum 59:236–244. https://doi.org/10.1097/DCR.0000000000000554
Park JS, Choi GS, Kim SH, Kim HR, Kim NK, Lee KY, Kang SB, Kim JY, Lee KY, Kim BC, Bae BN, Son GM, Lee SI, Kang H (2013) Multicenter analysis of risk factors for anastomotic leakage after laparoscopic rectal cancer excision: the Korean laparoscopic colorectal surgery study group. Ann Surg 257:665–671. https://doi.org/10.1097/SLA.0b013e31827b8ed9
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M (1998) Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg 85:338–355. https://doi.org/10.1046/j.1365-2168.1998.00615.x
Mäkelä JT, Kiviniemi H, Laitinen S (2003) Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis. Dis Colon Rectum 46:653–660. https://doi.org/10.1007/s10350-004-6627-9
Hallböök O, Matthiessen P, Leinsköld T, Nyström PO, Sjödahl R (2002) Safety of the temporary loop ileostomy. Colorectal Dis 4:361–364. https://doi.org/10.1046/j.1463-1318.2002.00398.x
Gessler B, Haglind E, Angenete E (2014) A temporary loop ileostomy affects renal function. Int J Colorectal Dis 29:1131–1135. https://doi.org/10.1007/s00384-014-1949-0
Peltrini R, Imperatore N, Altieri G, Castiglioni S, Di Nuzzo MM, Grimaldi L, D’Ambra M, Lionetti R, Bracale U, Corcione F (2021) Prevention of incisional hernia at the site of stoma closure with different reinforcing mesh types: a systematic review and meta-analysis. Hernia 25:639–648. https://doi.org/10.1007/s10029-021-02393-w
Beck-Kaltenbach N, Voigt K, Rumstadt B (2011) Renal impairment caused by temporary loop ileostomy. Int J Colorectal Dis 26:623–626. https://doi.org/10.1007/s00384-010-1086-3
Robertson I, Leung E, Hughes D, Spiers M, Donnelly L, Mackenzie I, Macdonald A (2005) Prospective analysis of stoma-related complications. Colorectal Dis 7:279–285. https://doi.org/10.1111/j.1463-1318.2005.00785.x
Alves A, Panis Y, Lelong B, Dousset B, Benoist S, Vicaut E (2008) Randomized clinical trial of early versus delayed temporary stoma closure after proctectomy. Br J Surg 95:693–698. https://doi.org/10.1002/bjs.6212
Bakx R, Busch OR, van Geldere D, Bemelman WA, Slors JF, van Lanschot JJ (2003) Feasibility of early closure of loop ileostomies: a pilot study. Dis Colon Rectum 46:1680–1684. https://doi.org/10.1007/BF02660775
Menegaux F, Jordi-Galais P, Turrin N, Chigot JP (2002) Closure of small bowel stomas on postoperative day 10. Eur J Surg 168:713–715. https://doi.org/10.1080/00000000000000008
Clausen FB, Dohrn N, Hölmich ER, Klein M, Gögenur I (2021) Safety of early ileostomy closure: a systematic review and meta-analysis of randomised controlled trials. Int J Colorectal Dis 36:203–212. https://doi.org/10.1007/s00384-020-03761-1
Cheng Z, Dong S, Bi D, Wang Y, Dai Y, Zhang X (2021) Early versus late preventive ileostomy closure following colorectal surgery: systematic review and meta-analysis with trial sequential analysis of randomized controlled trials. Dis Colon Rectum 64:128–137. https://doi.org/10.1097/DCR.0000000000001839
Menahem B, Lubrano J, Vallois A, Alves A (2018) Early closure of defunctioning loop ileostomy: is it beneficial for the patient? A meta-analysis. World J Surg 42:3171–3178. https://doi.org/10.1007/s00268-018-4603-0
Ng ZQ, Levitt M, Platell C (2020) The feasibility and safety of early ileostomy reversal: a systematic review and meta-analysis. ANZ J Surg 90:1580–1587. https://doi.org/10.1111/ans.16079
Wang L, Chen X, Liao C, Wu Q, Luo H, Yi F, Wei Y, Zhang W (2021) Early versus late closure of temporary ileostomy after rectal cancer surgery: a meta-analysis. Surg Today 51:463–471. https://doi.org/10.1007/s00595-020-02115-2
Lasithiotakis K, Aghahoseini A, Alexander D (2016) Is early reversal of defunctioning ileostomy a shorter, easier and less expensive operation? World J Surg 40:1737–1740. https://doi.org/10.1007/s00268-016-3448-7
Danielsen AK, Park J, Jansen JE, Bock D, Skullman S, Wedin A, Marinez AC, Haglind E, Angenete E, Rosenberg J (2017) Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg 265:284–290. https://doi.org/10.1097/SLA.0000000000001829
Gallyamov EA, Agapov MA, Lutsevich OE, Kubyshkin VA, Kakotkin VV, Tolstykh MP (2019) Early ileostomy closure in patients with rectal cancer. Primary results of the randomised controlled multicenter trial. Khirurgiia (Mosk) 6:35–40. English, Russian https://doi.org/10.17116/hirurgia201906135
Kłęk S, Pisarska M, Milian-Ciesielska K, Cegielny T, Choruz R, Sałówka J, Szybinski P, Pędziwiatr M (2018) Early closure of the protective ileostomy after rectal resection should become part of the Enhanced Recovery After Surgery (ERAS) protocol: a randomized, prospective, two-center clinical trial. Wideochir Inne Tech Maloinwazyjne 13:435–441. https://doi.org/10.5114/wiitm.2018.79574
Elsner AT, Brosi P, Walensi M, Uhlmann M, Egger B, Glaser C, Maurer CA (2021) Closure of temporary ileostomy 2 versus 12 weeks after rectal resection for cancer: a word of caution from a prospective, randomized controlled multicenter trial. Dis Colon Rectum 64:1398–1406. https://doi.org/10.1097/DCR.0000000000002182
Bausys A, Kuliavas J, Dulskas A, Kryzauskas M, Pauza K, Kilius A, Rudinskaite G, Sangaila E, Bausys R, Stratilatovas E (2019) Early versus standard closure of temporary ileostomy in patients with rectal cancer: a randomised controlled trial. J Surg Oncol 120:294–299. https://doi.org/10.1002/jso.25488
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406. https://doi.org/10.1016/j.jclinepi.2010.07.015
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors) (2021) Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane. Available from www.training.cochrane.org/handbook
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. https://doi.org/10.1136/bmj.j4008
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Büchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147:339–351. https://doi.org/10.1016/j.surg.2009.10.012
Shabbir J, Britton DC (2010) Stoma complications: a literature overview. Colorectal Dis 12:958–964. https://doi.org/10.1111/j.1463-1318.2009.02006.x
Review Manager Web (RevMan Web). Version (1.22.0). The Cochrane Collaboration, (October 2020). Available at https://revman.cochrane.org/
DerSimonian R, Laird N (2015) Meta-analysis in clinical trials revisited. Contemp Clin Trials 45(Pt A):139–145. https://doi.org/10.1016/j.cct.2015.09.002
Wetterslev J, Thorlund K, Brok J, Gluud C (2008) Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 61:64–75. https://doi.org/10.1016/j.jclinepi.2007.03.013
O’Brien PC, Fleming TR (1979) A multiple testing procedure for clinical trials. Biometrics 35:549–556
Thorlund K, Devereaux PJ, Wetterslev J, Guyatt G, Ioannidis JP, Thabane L, Gluud LL, Als-Nielsen B, Gluud C (2009) Can trial sequential monitoring boundaries reduce spurious inferences from meta-analyses? Int J Epidemiol 38:276–286. https://doi.org/10.1093/ije/dyn179
Brok J, Thorlund K, Wetterslev J, Gluud C (2009) Apparently conclusive meta-analyses may be inconclusive–trial sequential analysis adjustment of random error risk due to repetitive testing of accumulating data in apparently conclusive neonatal meta-analyses. Int J Epidemiol 38:287–298. https://doi.org/10.1093/ije/dyn188
Farag S, Rehman S, Sains P, Baig MK, Sajid MS (2017) Early vs delayed closure of loop defunctioning ileostomy in patients undergoing distal colorectal resections: an integrated systematic review and meta-analysis of published randomised controlled trials. Colorectal Dis 19:1050–1057. https://doi.org/10.1111/codi.13922
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, Emberson JR, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
GRADEpro GDT (2020) GRADEpro Guideline Development Tool [Software]. McMaster University, 2020 (developed by Evidence Prime, Inc.). Available from https://gradepro.org/
Schünemann H, Brożek J, Guyatt G, Oxman A, (editors) (2013) GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group. Available from https://guidelinedevelopment.org/handbook
Park J, Danielsen AK, Angenete E, Bock D, Marinez AC, Haglind E, Jansen JE, Skullman S, Wedin A, Rosenberg J (2018) Quality of life in a randomised trial of early closure of temporary ileostomy after rectal resection for cancer (EASY trial). Br J Surg 105:244–251. https://doi.org/10.1002/bjs.10680
Park J, Angenete E, Bock D, Correa-Marinez A, Danielsen AK, Gehrman J, Haglind E, Jansen JE, Skullman S, Wedin A, Rosenberg J (2020) Cost analysis in a randomised trial of early closure of a temporary ileostomy after rectal resection for cancer (EASY trial). Surg Endosc 34:69–76. https://doi.org/10.1007/s00464-019-06732-y
Keane C, Park J, Öberg S, Wedin A, Bock D, O’Grady G, Bissett I, Rosenberg J, Angenete E (2019) Functional outcomes from a randomised trial of early closure of temporary ileostomy after rectal excision for cancer. Br J Surg 106:645–652. https://doi.org/10.1002/bjs.11092
Dulskas A, Petrauskas V, Kuliavas J, Bickaite K, Kairys M, Pauza K, Kilius A, Sangaila E, Bausys R, Stratilatovas E (2021) Quality of life and bowel function following early closure of a temporary ileostomy in patients with rectal cancer: a report from a single-center randomized controlled trial. J Clin Med 10:768. https://doi.org/10.3390/jcm10040768
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
Ferrara F, Parini D, Bondurri A, Veltri M, Barbierato M, Pata F, Cattaneo F, Tafuri A, Forni C, Roveron G, Rizzo G, Multidisciplinary Italian Study group for STOmas (MISSTO) (2019) Italian guidelines for the surgical management of enteral stomas in adults. Tech Coloproctol 23:1037–1056. https://doi.org/10.1007/s10151-019-02099-3
Espin Basany E, Solís-Peña A, Pellino G, Kreisler E, Fraccalvieri D, Muinelo-Lorenzo M, Maseda-Díaz O, García-González JM, Santamaría-Olabarrieta M, Codina-Cazador A, Biondo S (2020) Preoperative oral antibiotics and surgical-site infections in colon surgery (ORALEV): a multicentre, single-blind, pragmatic, randomised controlled trial. Lancet Gastroenterol Hepatol 5:729–738. https://doi.org/10.1016/S2468-1253(20)30075-3
Spence RT, Hirpara DH, Doshi S, Quereshy FA, Chadi SA (2021) Anastomotic leak after colorectal surgery: does timing affect failure to rescue? Surg Endosc. https://doi.org/10.1007/s00464-020-08270-4. Epub ahead of print
Tang CL, Seow-Choen F, Fook-Chong S, Eu KW (2003) Bioresorbable adhesion barrier facilitates early closure of the defunctioning ileostomy after rectal excision: a prospective, randomised trial. Dis Colon Rectum 46:1200–1207. https://doi.org/10.1007/s10350-004-6716-9
Keane C, Fearnhead NS, Bordeianou LG, Christensen P, Basany EE, Laurberg S, Mellgren A, Messick C, Orangio GR, Verjee A, Wing K, Bissett I, LARS International Collaborative Group (2020) International Consensus Definition of Low Anterior Resection Syndrome. Dis Colon Rectum 63:274–284. https://doi.org/10.1097/DCR.0000000000001583
Vogel I, Reeves N, Tanis PJ, Bemelman WA, Torkington J, Hompes R, Cornish JA (2021) Impact of a defunctioning ileostomy and time to stoma closure on bowel function after low anterior resection for rectal cancer: a systematic review and meta-analysis. Tech Coloproctol 25:751–760. https://doi.org/10.1007/s10151-021-02436-5
Coimbra R, Edwards S, Kurihara H, Bass GA, Balogh ZJ, Tilsed J, Faccincani R, Carlucci M, Martínez Casas I, Gaarder C, Tabuenca A, Coimbra BC, Marzi I (2020) European Society of Trauma and Emergency Surgery (ESTES) recommendations for trauma and emergency surgery preparation during times of COVID-19 infection. Eur J Trauma Emerg Surg 46:505–510. https://doi.org/10.1007/s00068-020-01364-7
Francis N, Dort J, Cho E, Feldman L, Keller D, Lim R, Mikami D, Phillips E, Spaniolas K, Tsuda S, Wasco K, Arulampalam T, Sheraz M, Morales S, Pietrabissa A, Asbun H, Pryor A (2020) SAGES and EAES recommendations for minimally invasive surgery during COVID-19 pandemic. Surg Endosc 34:2327–2331. https://doi.org/10.1007/s00464-020-07565-w
Zenger S, Gurbuz B, Can U, Balik E, Yalti T, Bugra D (2021) Comparative study between ghost ileostomy and defunctioning ileostomy in terms of morbidity and cost-effectiveness in low anterior resection for rectal cancer. Langenbecks Arch Surg 406:339–347. https://doi.org/10.1007/s00423-021-02089-w
Morks AN, Ploeg RJ, Sijbrand Hofker H, Wiggers T, Havenga K (2013) Late anastomotic leakage in colorectal surgery: a significant problem. Colorectal Dis 15:e271–e275. https://doi.org/10.1111/codi.12167
Clinical Outcomes of Surgical Therapy Study Group, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059. https://doi.org/10.1056/NEJMoa032651
Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, Pique JM (2008) The long-term results of a randomised clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg 248:1–7. https://doi.org/10.1097/SLA.0b013e31816a9d65
Colon Cancer Laparoscopic or Open Resection Study Group, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52. https://doi.org/10.1016/S1470-2045(08)70310-3
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM, MRC CLASICC trial group (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726. https://doi.org/10.1016/S0140-6736(05)66545-2
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PW, Nelson H (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355. https://doi.org/10.1001/jama.2015.10529
Zhou ZG, Hu M, Li Y, Lei WZ, Yu YY, Cheng Z, Li L, Shu Y, Wang TC (2004) Laparoscopic versus open total mesorectal excision with anal sphincter preservation for low rectal cancer. Surg Endosc 18:1211–1215. https://doi.org/10.1007/s00464-003-9170-1
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N, Tilney H, Gudgeon M, Bianchi PP, Edlin R, Hulme C, Brown J (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318:1569–1580. https://doi.org/10.1001/jama.2017.7219
Author information
Authors and Affiliations
Contributions
MP: study conception and design, literature search, acquisition, interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. FC: study conception and design, literature search, acquisition, interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. CG: interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. GC: interpretation and analysis of data (trial sequential analysis); drafting and critically revising the article for important intellectual content; and final approval of the version to be published. MSJW: interpretation and analysis of data; drafting and critically revising the article for important intellectual content; editing and revising the English for the final version to be published; and final approval of the version to be published. MS: interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. DP: interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. FC: interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. RP: interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. UB: interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. AP: study conception and design, literature search, acquisition, interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published.
Corresponding author
Ethics declarations
Ethical approval
No ethical approval was required for this article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
384_2022_4106_MOESM1_ESM.tiff
Supplementary file1 (Suppl. Digit. Content. Fig.1. Funnel plots. A Morbidity B Leak of rectal anastomosis C Unplanned reoperation D Operative time E Clavien-Dindo III-IV complication F Post-operative small bowel obstruction G Wound complication H Post-operative intra-abdominal abscess I Stoma-related complication TIFF 144 KB)
384_2022_4106_MOESM4_ESM.doc
Supplementary file4 (Suppl. Digit. Content. Table 3. Clinical Outcomes of patients following early and delayed ileostomy closure DOC 36 KB)
384_2022_4106_MOESM5_ESM.doc
Supplementary file5 (Suppl. Digit. Content. Table 4. Morbidity Outcomes of patients following early and delayed ileostomy closure DOC 34 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Podda, M., Coccolini, F., Gerardi, C. et al. Early versus delayed defunctioning ileostomy closure after low anterior resection for rectal cancer: a meta-analysis and trial sequential analysis of safety and functional outcomes. Int J Colorectal Dis 37, 737–756 (2022). https://doi.org/10.1007/s00384-022-04106-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04106-w