Abstract
Objective
To evaluate outcomes and predictors of survival of pediatric thyroid carcinoma, specifically papillary thyroid carcinoma.
Methods
SEER was searched for surgical pediatric cases (≤20 years old) of papillary thyroid carcinoma diagnosed between 1973 and 2011. Demographics, clinical characteristics, and survival outcomes were analyzed using standard statistical methods. All papillary types, including follicular variant, were included.
Results
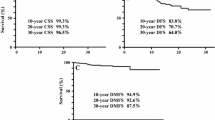
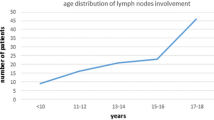
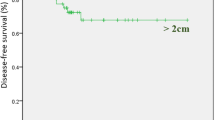
A total of 2504 cases were identified. Overall incidence was 0.483/100,000 persons per year with a significant annual percent change (APC) in occurrence of 2.07 % from baseline (P < 0.05). Mean age at diagnosis was 16 years and highest incidence was found in white, female patients ages 15–19. Patients with tumor sizes <1 cm more likely received lobectomies/isthmusectomies versus subtotal/total thyroidectomies [OR = 3.03 (2.12, 4.32); P < 0.001]. Patients with tumors ≥1 cm and lymph node-positive statuses [OR = 99.0 (12.5, 783); P < 0.001] more likely underwent subtotal/total thyroidectomy compared to lobectomy/isthmusectomy. Tumors ≥1 cm were more likely lymph node-positive [OR = 39.4 (16.6, 93.7); p < 0.001]. Mortality did not differ between procedures. Mean survival was 38.6 years and higher in those with regional disease. Disease-specific 30-year survival ranged from 99 to 100 %, regardless of tumor size or procedure. Lymph node sampling did not affect survival.
Conclusions
The incidence of pediatric papillary thyroid cancer is increasing. Females have a higher incidence, but similar survival to males. Tumors ≥1 cm were likely to be lymph node-positive. Although tumors ≥1 cm were more likely to be resected by subtotal/total thyroidectomy, survival was high and did not differ based on procedure.



Similar content being viewed by others
References
Collini P, Massimino M, Leite SF et al (2006) Papillary thyroid carcinoma of childhood and adolescence: a 30-year experience at the istituto nazionale tumori in milan. Pediatr Blood Cancer 46:300–306
Dinauer CA, Breuer C, Rivkees SA (2008) Differentiated thyroid cancer in children: diagnosis and management. Curr Opin Oncol 20:59–65
Luster M, Lassmann M, Freudenberg LS et al (2007) Thyroid cancer in childhood: management strategy, including dosimetry and long-term results. Hormones 6:269–278
Hogan AR, Zhuge Y, Perez EA et al (2009) Pediatric thyroid carcinoma: incidence and outcomes in 1753 patients. J Surg Res 156:167–172
Hay ID, Gonzalez-Losada T, Reinalda MS et al (2010) Long-term outcome in 215 children and adolescents with papillary thyroid cancer treated during 1940 through 2008. World J Surg 34:1192–1202
Dzepina D (2012) Surgical and pathological characteristics of papillary thyroid cancer in children and adolescents. Int J Pediatr 2012:125389
Grigsby PW, Gal-or A, Michalski JM et al (2002) Childhood and adolescent thyroid carcinoma. Cancer 95:724–729
Diesen DL, Skinner MA (2012) Pediatric thyroid cancer. Semin Pediatr Surg 21:44–50
Zimmerman D, Hay ID, Gough IR et al (1988) Papillary thyroid carcinoma in children and adults: long-term follow-up of 1039 patients conservatively treated at one institution during three decades. Surgery 104:1157–1166
Spinelli C, Bertocchini A, Antonelli A et al (2004) Surgical therapy of the thyroid papillary carcinoma in children: experience with 56 patients < or = 16 years old. J Pediatr Surg 39:1500–1505
La Quaglia MP, Black T, Holcomb GW 3rd et al (2000) Differentiated thyroid cancer: clinical characteristics, treatment, and outcome in patients under 21 years of age who present with distant metastases. A report from the surgical discipline committee of the children’s cancer group. J Pediatr Surg 35:955–959 (discussion 960)
Cady B (1998) Presidential address: beyond risk groups—a new look at differentiated thyroid cancer. Surgery 124:947–957
Bal CS, Padhy AK, Kumar A (2001) Clinical features of differentiated thyroid carcinoma in children and adolescents from a sub-himalayan iodine-deficient endemic zone. Nucl Med Commun 22:881–887
Schlumberger M, Tubiana M, De Vathaire F et al (1986) Long-term results of treatment of 283 patients with lung and bone metastases from differentiated thyroid carcinoma. J Clin Endocrinol Metab 63:960–967
La Quaglia MP, Corbally MT, Heller G et al (1988) Recurrence and morbidity in differentiated thyroid carcinoma in children. Surgery 104:1149–1156
Brink JS, van Heerden JA, McIver B et al (2000) Papillary thyroid cancer with pulmonary metastases in children: long-term prognosis. Surgery 128:881–886 (discussion 886-887)
Perez EA, Gutierrez JC, Koniaris LG et al (2009) Malignant pancreatic tumors: incidence and outcome in 58 pediatric patients. J Pediatr Surg 44:197–203
McAteer JP, Huaco JA, Gow KW (2013) Predictors of survival in pediatric adrenocortical carcinoma: a surveillance, epidemiology, and end results (seer) program study. J Pediatr Surg 48:1025–1031
Gutierrez JC, Fischer AC, Sola JE et al (2007) Markedly improving survival of neuroblastoma: a 30-year analysis of 1,646 patients. Pediatr Surg Int 23:637–646
Yang R, Cheung MC, Zhuge Y et al (2010) Primary solid tumors of the colon and rectum in the pediatric patient: a review of 270 cases. J Surg Res 161:209–216
Allan BJ, Wang B, Davis JS et al (2014) A review of 218 pediatric cases of hepatocellular carcinoma. J Pediatr Surg 49:166–171
Allan BJ, Parikh PP, Diaz S et al (2013) Predictors of survival and incidence of hepatoblastoma in the paediatric population. HPB (Oxford). 15:741–746
Allan BJ, Thorson CM, Davis JS et al (2013) An analysis of 73 cases of pediatric malignant tumors of the thymus. J Surg Res 184:397–403
Davis JS, Allan BJ, Perez EA et al (2013) Primary pediatric cardiac malignancies: the seer experience. Pediatr Surg Int 29:425–429
Kassira N, Pedroso FE, Cheung MC et al (2011) Primary gastrointestinal tract lymphoma in the pediatric patient: review of 265 patients from the seer registry. J Pediatr Surg 46:1956–1964
Young JL Jr, Percy CL, Asire AJ et al (1981) Cancer incidence and mortality in the United States, 1973–77. Natl Cancer Inst Monogr 57:1–187
Harness JK (1997) Childhood thyroid carcinoma. In: Clark OH, Duh Q-Y (eds) Textbook of endocrine surgery. Saunders, Philadelphia pp 75–81
Tucker MA, Jones PH, Boice JD Jr et al (1991) Therapeutic radiation at a young age is linked to secondary thyroid cancer. The late effects study group. Cancer Res 51:2885–2888
Thompson GB, Hay ID (2004) Current strategies for surgical management and adjuvant treatment of childhood papillary thyroid carcinoma. World J Surg 28:1187–1198
Wiersinga WM (2007) Management of thyroid nodules in children and adolescents. Hormones 6:194–199
Harach HR, Williams ED (1995) Childhood thyroid cancer in england and wales. Br J Cancer 72:777–783
Newman KD, Black T, Heller G et al (1998) Differentiated thyroid cancer: determinants of disease progression in patients <21 years of age at diagnosis: a report from the surgical discipline committee of the children’s cancer group. Ann Surg 227:533–541
Collini P, Mattavelli F, Pellegrinelli A et al (2006) Papillary carcinoma of the thyroid gland of childhood and adolescence: morphologic subtypes, biologic behavior and prognosis: a clinicopathologic study of 42 sporadic cases treated at a single institution during a 30-year period. Am J Surg Pathol 30:1420–1426
Mazzaferri EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97:418–428
Massimino M, Collini P, Leite SF et al (2006) Conservative surgical approach for thyroid and lymph-node involvement in papillary thyroid carcinoma of childhood and adolescence. Pediatr Blood Cancer 46:307–313
Farrar WB, Cooperman M, James AG (1980) Surgical management of papillary and follicular carcinoma of the thyroid. Ann Surg 192:701–704
Gemsenjager E, Heitz PU, Martina B (1997) Selective treatment of differentiated thyroid carcinoma. World J Surg 21:546–551
Hay ID, McConahey WM, Goellner JR (2002) Managing patients with papillary thyroid carcinoma: insights gained from the mayo clinic’s experience of treating 2,512 consecutive patients during 1940 through 2000. Trans Am Clin Climatol Assoc 113:241–260
Hay ID, Bergstralh EJ, Goellner JR et al (1993) Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery 114:1050–1057
Hay ID, Thompson GB, Grant CS et al (2002) Papillary thyroid carcinoma managed at the mayo clinic during six decades (1940–1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg 26:879–885
Adam MA, Pura J, Gu L et al (2014) Extent of surgery for papillary thyroid cancer is not associated with survival: an analysis of 61,775 patients. Ann Surg 260:601–605
Nemec JZV, Pohunkova D et al (1986) Some factors influencing the survival of patients with less advanced stages of differentiated thyroid cancer. Endocrinol Exp. 20:85–95
Demidchik Iu E, Kontratovich VA (2003) Repeat surgery for recurrent thyroid cancer in children. Vopr Onkol 49:366–369
Chan AC, Lang BH, Wong KP (2013) The pros and cons of routine central compartment neck dissection for clinically nodal negative (cn0) papillary thyroid cancer. Gland Surg 2:186–195
Schneider DF, Mazeh H, Chen H et al (2013) Lymph node ratio predicts recurrence in papillary thyroid cancer. Oncologist 18:157–162
Landau D, Vini L, A’Hern R et al (2000) Thyroid cancer in children: the royal marsden hospital experience. Eur J Cancer 36:214–220
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Author contributions
JES, JIL, ARH, and EAP contributed to study conception and design. SG, JT, and EAP contributed to acquisition, analysis and interpretation of data. SG, JT, JES, ARH, and EAP contributed to drafting of manuscript. All authors contributed to critical revision of manuscript.
Financial disclosures
No authors have any financial affiliations to disclose.
Rights and permissions
About this article
Cite this article
Golpanian, S., Perez, E.A., Tashiro, J. et al. Pediatric papillary thyroid carcinoma: outcomes and survival predictors in 2504 surgical patients. Pediatr Surg Int 32, 201–208 (2016). https://doi.org/10.1007/s00383-015-3855-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-015-3855-0