Abstract
Objectives
To investigate the specific strengths of MRI and PET components in 68Ga-PSMA-11 PET/MRI for staging of patients with biochemically recurrent prostate cancer (PCa).
Methods
Patients with biochemical recurrence of PCa and contrast-enhanced whole-body 68Ga-PSMA-11 PET/MRI including a dedicated pelvic multiparametric MRI were included in this retrospective study. Imaging datasets of MRI and PET were evaluated separately regarding local PCa recurrence (Tr), pelvic lymph node metastases (N1), distant lymph node metastases (M1a), bone metastases (M1b), and soft tissue metastases (M1c) according to PROMISE version 1. Data evaluation was performed patient- and region-/lesion-based. Cox regression revealed a PSA of 1.69 ng/mL as a cut-off for subgroup analysis. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were evaluated for each image component. Differences in staging accuracy were assessed using the Wilcoxon and McNemar test.
Results
Altogether 102 patients (mean aged 68 ± 8 years, median PSA 1.33 ng/mL) were included. PCa was found in 70/102 (68%) patients. Accuracy of MRI in the detection of Tr, N1, M + , M1a, and M1b was 100%, 79%, 90%, 97%, and 95% for PSA < 1.69 ng/mL and 100%, 87%, 87%, 91%, and 96% for PSA > 1.69 ng/mL. Accuracy of 68Ga-PSMA-11 PET was 93%, 97%, 93%, 98%, and 100% for PSA < 1.69 ng/mL and 87%, 91%, 96%, 100%, and 96% for PSA > 1.69 ng/mL.
Conclusions
Combined assessment of 68Ga-PSMA-11 PET/MRI improves tumor localization in men with biochemical recurrence. The MRI detected local recurrence of PCa more often whereas 68 Ga-PSMA-11 PET detected lymph node metastases more often, especially for PSA < 1.69 ng/mL.
Clinical relevance statement
This study gives a scientific baseline to improve the understanding and reading of 68Ga-PSMA-11 PET/MRI imaging in patients with biochemically recurrent PCa by showing the specific strength of each imaging component.
Key Points
• Combining the individual modality strengths of 68Ga-PSMA-11 PET/MRI improves tumor localization in men with biochemical recurrence of prostate cancer.
• MRI component of 68 Ga-PSMA-11 PET/MRI shows its strength in detecting local recurrence of prostate cancer, especially at PSA < 1.69 ng/mL.
• 68 Ga-PSMA-11 PET component shows its strength in detecting local and distant lymph node metastases, especially at PSA < 1.69 ng/mL.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Both 68 Ga-PSMA PET and multiparametric MRI play an increasing role in the work-up of prostate cancer (PCa) [1]. After curative therapy with radical prostatectomy (RP) or radiotherapy (RT), recurrence occurs in approximately 20 to 40% of cases, depending on the individual PCa risk category [2, 3]. Follow-up by measuring prostate-specific antigen (PSA) levels is crucial to detect recurrence as soon as possible. At least two PSA levels of 0.2 ng/mL or higher after RP or an increase in PSA of at least 2 ng/mL above the nadir after RT is defined as a biochemical recurrence of PCa [4]. Imaging plays a major role in localizing recurrent disease manifestations and paves the way for further salvage treatment [5, 6]. Therapy options range from curative concepts (e.g., in case of local recurrence) to stereotactic radiation therapy (e.g., in case of distant oligometastasis) and palliation. Therefore, metabolic imaging using prostate-specific membrane antigen (PSMA) PET/CT is taking an increasing role providing both, higher sensitivity and specificity compared to conventional imaging [7,8,9]. Nonetheless, due to tracer accumulation in the bladder and reduced soft tissue contrast, especially the identification of local recurrence in an early stage can be challenging by Ga-PSMA PET and/or CT while being crucial for therapy decisions [10]. Multiparametric magnetic-resonance-imaging (mpMRI) shows a high soft tissue contrast that might visualize local PCa recurrence more precisely, even in very small lesions [10, 11]. However, MRI is not the modality of choice for detecting small lymph node metastases due to reduced sensitivity and specificity [12, 13]. PET/MRI scanners might be advantageous with a dedicated, body region-focused and multiparametric MRI protocol in combination with a fast whole-body PET protocol (68 Ga-PSMA) [14]. Current 68 Ga-PSMA PET/MRI studies have primarily taken a competing approach to 68 Ga-PSMA PET/CT as well as CT, MRI, or bone scintigraphy, rather than evaluating the complementary information arising from the PSMA-PET and MRI component [15, 16]. Therefore, the aim of this study was to investigate the specific impact of each imaging component at 68 Ga-PSMA PET/MRI for staging patients with biochemical PCa recurrence.
Material and methods
Patients
The institutional review board (study number 11–4822-BO) approved this study and it was performed in accordance with the Declaration of Helsinki [17]. A general written informed consent form was obtained from all patients undergoing PET/MRI for staging to cover possible further analysis.
This retrospective study included patients with biochemical recurrence of PCa after RP and RT between 01/2015 and 09/2021 at the Department of Nuclear Medicine and Department of Diagnostic and Interventional Radiology (University-Hospital-Essen). All patients underwent a contrast-enhanced whole-body 68Ga-PSMA-11 PET/MRI. The minimum requirement for the inclusion of the patients was the presence of at least one T2-weighted (T2w) sequence, one T1w post-contrast sequence, and one PET reconstruction that included the prostate fossa. Furthermore, only patients were included with additional recorded patient characteristics including age-, PSA level at the time of scan, and choice of initial curative treatment. Patients suffering from other second malignancies were excluded from the retrospective data collection.
Whole-body/multiparametric pelvic PET/MRI
All 68Ga-PSMA-11 PET/MRI examinations were performed on an integrated 3-Tesla PET/MRI system (Biograph mMR, Siemens Healthcare GmbH) with an average delay of 130 ± 61 min after 68Ga-PSMA-11 injection. The total mean activity was 111 ± 35 MBq. The field of view of 68GaPSMA-11 PET/MRI examinations was chosen from the skull base to the mid-thigh except for 12/102 patients who underwent a single pelvic PET/MRI. 68Ga-PSMA-11 PET/MRI was performed using a high-channel surface coil. First, simultaneous PET and 3D-Dixon-VIBE sequences for MRI-based scatter correction were performed (acquisition time 2 min per bed position using static frames). PET was reconstructed using iterative reconstruction (3 iterations, 21 subsets) and a Gaussian filter (4 mm). A standardized whole-body MRI protocol was performed for 90/102 as visualized in Table 1. The following MR sequences were acquired for the whole body protocol: (i) axial 3D Dixon VIBE pre- and post-contrast imaging and (ii) diffusion-weighted sequences (including high b values, b = 0, 1000, 1500, 2000), and the following MR sequences were acquired for prostate imaging: (i) high-resolution T2-weighted fast spin-echo (TSE) sequences (axial, coronal, and sagittal planes), (ii) diffusion-weighted sequences (including high b values, b = 0, 50, 1000, 1500, 2000), and (iii) dynamic (after RT) or single (after RP) T1w-contrast-enhanced imaging (VIBE sequence). Depending on a steady improvement of the staging algorithm during the long inclusion period and due to occasional premature examination stops, variations in quality and completeness of the acquired mpMRI / whole-body MRI and PET sequences were present.
Image analysis
Using the dedicated imaging processing software OsiriX (Pixmeo SARL), imaging datasets of the 68Ga-PSMA-11 PET/MRI examination were analyzed by board-certified radiologists and nuclear medicine physicians with experience in reading multiparametric prostate MRI and hybrid imaging and PSMA PET. Readers were aware of the biochemical recurrence of PCa and individual PSA levels but blinded to patient identification data and prior- or follow-up examinations. Blinded to the 68Ga-PSMA-11 PET images, MRI whole-body sequences as well as the MRI sequences of the prostate fossa were evaluated by a uro-radiological specialist with more than 12 years of experience. Independently from that and blinded to all MRI sequences, the 68Ga-PSMA-11 PET images were evaluated by the hybrid imaging specialist with more than five years of experience. An image quality score (QUAL score) was determined for the MRI component and a 5-point Likert score for the PET component of each 68Ga-PSMA-11 PET/MRI examination to address variances in image quality (Table 2) [18]. According to the PI-QUAL score that was developed and well established in treatment-naive patients undergoing prostate cancer detection, a QUAL score was defined for this study in patients with biochemical recurrence of PCa after therapy [18]. The QUAL score was used in the same approach. A QUAL score of five was defined as a fully acquired MRI of the prostate fossa according to the mentioned sequences (see Table 1) with an optimal diagnostic quality. The presence of at least one optimal T1 weighted post-contrast sequence including the prostate fossa was considered as the presence of the contrast-enhanced prostate sequence, even in the absence of dynamic contrast-enhanced imaging. 68Ga-PSMA-11 PET image quality was subjectively rated depending on clinical experience according to a well-established 5-point Likert score ranging from one (non-diagnostic) to five (excellent quality) as already used and experienced in several other studies [19, 20].
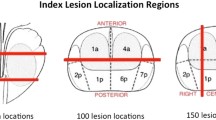
Localization and conspicuity were evaluated on both, MRI and PET components with respect to (i) local recurrence of PCa (Tr); (ii) pelvic lymph node metastases (N1) and amount (nodal amount; NA); (iii) distant lymph node metastases above the aortic bifurcation (M1a); (iv) bone metastases summing up all categories of bone metastases (M1b); and (v) parenchymal lesions (M1c) according to the PROMISE guidelines (version 1.0) [21]. Readers used a binary nomenclature to distinguish between malignant vs. benign to ensure better comparability. Deviating from the accepted PROMISE classification, the local recurrence of PCa was divided into Tr (local recurrence) and T0 (no local recurrence). Distant metastases (M1a, M1b, M1c) were also concluded to be M + (all distant metastases including bone metastases) [21]. For local- and distant soft-tissue recurrence of PCa, lesions with intermediate intensity on T2w imaging, accentuated contrast enhancement at T1w post-contrast sequence, high signal on diffusion-weighted imaging (DWI), and a low signal on the corresponding apparent diffusion coefficient (ADC) map (indication diffusion disorder) were suspicious for malignancy [15]. Local recurrence of PCa was measured at T1w post-contrast sequence (length x width in mm). In lymph nodes, typical pelvic location, short axis diameter exceeding 10 mm, or short axis diameter between 4 and 10 mm with a spherical configuration in typical localization and/or (suspicious) contrast enhancement were regarded as suspicious for malignancy [22]. Low signal intensity on T1w and high signal intensity on T2w imaging as well as contrast enhancement and diffusion disorder were consistent with bone metastases [15]. For lesion characterization on PET, visually increased focal 68Ga-PSMA-11 uptake in comparison to the background tissue was considered indicative of malignancy [23]. SUVmax of the index lesion was measured by using a spherical volume of interest.
Reference standard
For accurate lesion characterization in both modalities, the MRI and 68Ga-PSMA-11 PET images were evaluated in a separate consensus reading by both scientifically and clinically highly experienced readers to build an expert reference standard. Changes in previous data evaluation of each reader was not allowed. To improve expert-based reference standard, follow-up- and prior cross-sectional imaging was taken into account. Furthermore, if available clinical information was included from the readers to complete the modified reference standard according to previous publications on PET/MRI [24,25,26].
Statistical analysis
SPSS Statistics 26 (IBM Inc.) was used for statistical analysis. PSA-based subgroup analysis after cut-off evaluation using Cox regression (PSA < / > 1.69 ng/mL) was performed. Further subgroup analysis of RP-only patients and non-subgroup comparison was performed as visualized in the supplementary material. Subgroup analysis of RT-only patients was waived due to low, statistically non-suitable sample size. Data analysis was performed patient-based and region-/lesion-based. Descriptive analysis was performed and data are presented as mean ± SD, median, and interquartile range (IQR). Sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy were calculated for MRI and PET lesion-based evaluation including confidence intervals (CI) at 95%, except for the M1c stage due to the low number of cases. The Wilcoxon test was chosen for the evaluation of differences in tumor stage between MRI and 68 Ga-PSMA-11 PET. The McNemar test was used for binary group comparison at region-/lesion-based analysis except for the M1c stage according to the low number of cases. p values < 0.05 were considered to be statistically significant.
Results
In total n = 102 patients (mean age: 68 ± 8 years; range 51–83 years) with biochemical recurrence of PCa (median PSA: 1.33 ng/mL) were included in this retrospective study. Radical prostatectomy was performed in 92/102 (90%) patients (median PSA: 1.0 ng/mL) and 10/102 (10%) patients (median PSA: 3.85 ng/mL) received primary radiotherapy. MRI QUAL score revealed a median of 3 (IQR: 1) and PET 5-point Likert scale revealed a median of 4 (IQR: 1). A total of n = 38 patients had a MRI QUAL score below 3 and a total of n = 2 patients had a PET 5-point Likert scale below 3. According to the cut-off value of PSA 1.69 ng/ml for further subgroup analysis, 58/102 (57%) patients had a PSA value < 1.69 ng/mL, and 44/102 (43%) patients had a PSA value > 1.69 ng/mL.
Patient-based analysis
Altogether 27/58 (47%) patients (PSA < 1.69 ng/mL) and 43/44 (98%) patients (PSA > 1.69 ng/mL) had a recurrence of PCa according to the reference standard. In the subgroup of PSA < 1.69 ng/mL MRI identified 17/27 (63%) patients correct with five patients rated false positive (5/31, 16%), and 68Ga-PSMA-11 PET identified 24/27 (89%) patients correct with two patients rated false positive (2/31, 6%). Subgroup analysis of patients with PSA > 1.69 ng/mL revealed 39/43 (90%) patients correctly identified at MRI with one patient rated false positive and 37/43 (86%) patients correctly identified at 68Ga-PSMA-11 PET with one patient rated false positive.
According to the reference standard, all patients were subdivided into seven adapted PROMISE stages as visualized in Fig. 1 for PSA < 1.69 ng/mL and Fig. 2 for PSA > 1.69 ng/mL. Due to missing upper abdomen and chest imaging, determining the PROMISE stage was limited in 12 of the total 102 patients of the cohort. Correct tumor stage for PSA < 1.69 ng/mL subgroup was determined by MRI in 38/58 (66%) patients and by 68Ga-PSMA-11 PET in 50/58 (86%) patients and for PSA > 1.69 ng/mL subgroup in 29/44 (66%) patients (MRI) and 31/44 (70%) patients (68Ga-PSMA-11 PET). There were no significant differences between both imaging components (p > 0.05). Further PROMISE stage subgroup analysis of patients after RP and non-subgroup analysis is provided in the supplementary material without significant differences between both imaging components (p > 0.05).
Region- and lesion-based analysis
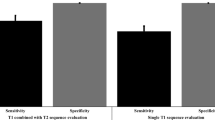
A statistical overview of PSA subgroup analysis is given in Tables 3 and 4. There were no significant differences in staging between MRI and 68Ga-PSMA-11 PET (p > 0.05). Further subgroup analysis of patients after RP and non-subgroup analysis also revealed no significant staging differences as visualized in the supplementary material. Sensitivity, specificity, PPV, NPV, and diagnostic accuracy for Tr, N1, M1 + , M1a, and M1b at PSA subgroup analysis are given in Table 5.
Local recurrence (Tr stage)
In PSA < 1.69 ng/mL subgroup 4/58 (7%) patients and in PSA > 1.69 ng/mL subgroup 17/44 (39%) patients had local recurrence according to the reference standard. MRI identified all Tr stages (see Tables 3 and 4). The mean size of local recurrence was 14 ± 4 (PSA < 1.69 ng/mL) and 19 ± 8 (PSA > 1.69 ng/mL). Missed local recurrence at 68Ga-PSMA-11 PET evaluation revealed a maximal diameter of 10 ± 1 mm (PSA < 1.69 ng/mL) and 21 ± 9 (PSA > 1.69 ng/mL). An example is visualized in Fig. 3.
Local recurrence of PCa arising from the vesico-urinary anastomosis. No suspicious uptake is visible in the 68Ga-PSMA-11 PET component (left A-B: MIP corona, axial dataset) due to tracer accumulation in the bladder. Dashed line in MIP corona (A) indicates axial PET layer (B). MpMRI depicts tumor relapse (right C-F, white arrow: T1w post contrast, T2w-TSE; DWI, ADC)
Pelvic lymph node metastases (N stage)
In the PSA < 1.69 ng/mL subgroup and the PSA > 1.69 ng/mL subgroup, 23/58 (40%) and 24/44 (55%) patients, respectively, had pelvic lymph node recurrence according to the reference standard. There was a total of 50 lymph node metastases in patients with PSA < 1.69 ng/mL and a total of 36 lymph node metastases in patients with PSA > 1.69 ng/mL. In MRI 20/50 (40%) lymph node metastases were identified by MRI whereas three were rated false positive for PSA < 1.69 ng/mL and 30/50 (60%) lymph node metastases for PSA > 1.69 ng/mL whereas two were rated false positive. Missed lymph node metastases at MRI evaluation revealed a maximal diameter of 3 mm ± 1 mm (PSA < 1.69 ng/mL) and 5 mm ± 2 mm (PSA > 1.69 ng/mL). Based on the 68Ga-PSMA-11 PET 34/50 (68%) lymph node metastases were identified for PSA < 1.69 ng/mL whereas one was rated false positive and 41/50 (82%) lymph node metastases were identified for PSA > 1.69 ng/mL whereas two were rated false positive. For an example, see Fig. 4. There is no CI overlap between MRI and 68Ga-PSMA-11 PET sensitivity in the PSA < 1.69 ng/mL subgroup (see Table 5).
Pelvic lymph node recurrence of PCa parailiacal right. Lymph node metastases are detected by tracer accumulation (SUVmax: 9.3) at 68Ga-PSMA-11 PET (left A-B, white arrow: MIP oblique, axial dataset). Dashed line in MIP corona (A) indicates axial PET layer (B). Unsuspicious lymph node appearance at mpMRI (right C-E, white arrow: T1w post contrast, ADC, DWI)
Detailed results of N stage subgroup analysis as well as further analysis of the M1 + stage, M1a stage, the M1b stage, and M1c stage are given in Tables 3 and 4 with no significant differences in staging between both imaging components (p > 0.05). A patient with the M1a stage is exemplified in Fig. 5 and a patient with the M1b stage is exemplified in Fig. 6.
Distant lymph node recurrence of PCa. Cervical (A) and retroperitoneal (C) lymph node metastases detectable by strong tracer accumulation (SUVmax: 60.3) at 68Ga-PSMA-11 PET (left A-C, white arrow: MIP corona, axial datasets). Dashed line in MIP corona (B) indicates axial PET layer (A, B). No pathological rating cervical (D) and retroperitoneal (E) at mpMRI (right, white arrow: T1w post contrast)
Bone metastases of PCa at os pubis right. Tracer accumulation (SUVmax: 10.9) was misinterpreted as lymph node metastases at 68Ga-PSMA-11 PET (left A-B, white arrow: MIP oblique, axial dataset). Dashed line in MIP oblique (A) indicates axial PET layer (B). Correct rating at mpMRI (right C-F, white arrow: T1w post contrast, T2w- TSE, DWI, ADC)
Discussion
According to both subgroups but especially for patients with lower PSA values, patient-based evaluation showed a general superiority of 68Ga-PSMA-11 PET component in identifying the localization of PCa recurrence. Nonetheless, the MRI component was superior in the detection of local recurrence (Tr stage). This trend was also existent in RP subgroup analysis and non-subgroup analysis. There were no significant statistical differences between both imaging components in patient-based evaluation. Region- and lesion-based analysis also revealed no statistically significant differences between both imaging components in detecting Tr, N1, M1 + , M1a, M1b, and M1c stage. Especially for patients with PSA values < 1.69 ng/mL the 68Ga-PSMA-11 PET component detected N1 stage more reliably (no CI overlap) than the MRI component.
MpMRI was highly sensitive in detecting local PCa recurrence and detected all local tumor relapses in both subgroups. This underlines the current literature highlighting the high value of MRI in detecting local recurrence based on its very good spatial resolution, soft tissue contrast, and the possibility of a dedicated dynamic contrast-enhanced (DCE) sequence [10, 11, 27,28,29,30]. Detection of a small local PCa recurrence can be challenging in 68Ga-PSMA-11 PET, especially as curative prostatectomy is usually associated with postoperative bladder descent into the prostatic fossa and most recurrences of PCa are localized at the vesico-urethral anastomosis. This region is often masked in PET images by tracer accumulation into the bladder (hot bladder), especially by using a 68 Ga-PSMA tracer [10, 15]. Therefore, local tumor relapse was missed in 50% (PSA < 1.69 ng/mL) and 29% (PSA > 1.69 ng/mL) of the patients in our study. The use of 18F-PSMA tracers might solve this problem due to its non-urinary excretion as highlighted by Giesel and colleagues but is also accompanied by a larger amount of false positive bone lesions and higher inter-reader variability [31].
Publications highlighted repeatedly the benefit of 68Ga-PSMA PET in the detection of pelvic lymph node metastases compared to conventional imaging like CT or MRI [11, 29]. This is in line with the results of this study, and especially for patients with PSA values below 1.69 ng/mL reporting accuracy of 79% for mpMRI and 97% for 68Ga-PSMA-11 PET. Although there were no significant differences in staging between these two imaging components at group comparison, the borderline overlap of the CI for accuracy and no overlap for sensitivity indicates a clinically relevant difference in staging potential that might be not significant due to the limited number of patients. The superior detection rate is explainable by the high prevalence of pelvic lymph node metastases not reaching a pathologic threshold of 10 mm diameter (short-axis), especially in lower PSA values [22, 32, 33]. At our data evaluation, missed lymph node metastases at MRI revealed a maximum diameter (short-axis) of 3–5 ± 1–2 mm according to the PSA subgroup. Even though Valentin et al (2022) promote that in typical localizations and with a round-shaped appearance metastasis up to 4 mm could be detected [22], lymph node metastases with a short axis diameter below 10 mm are challenging to identify at mpMRI. Especially in these very small and therefore early lymph node metastases, the accumulation of prostate-specific tracer enables their detection.
Detection of distant metastases showed non-significant but better performance of the 68 Ga-PSMA-11 PET component. However, similar to the localization of pelvic recurrences, the strength of each available imaging component was further evaluated separately for lymph nodes and bone metastases. Consistent with the detection of pelvic lymph node metastases, the 68 Ga-PSMA-11 PET slightly outperformed MRI component in detecting distant lymph node metastases (M1a) in this study for both subgroups, reporting accuracy of 97% and 91% for mpMRI (PSA < / > 1.69 ng/mL) as well as 98% and 100% for 68 Ga-PSMA-11 PET (PSA < / > 1.69 ng/mL). Some studies revealed that early stages of bone metastases can be detected more easily at MRI by changes in signal intensities at MRI due to growing malignant cell clusters in bone marrow [34, 35]. However, there are prospective data that prove the superiority of PSMA PET over MRI for M1b staging, taking into account that only diffusion-weighted imaging of MRI was used for comparison [36]. While the superiority of MRI could be visualized for patients with PSA values > 1.69 ng/mL, the reduced sensitivity of the 68Ga-PSMA-11 PET component visualized in the PSA subgroup with PSA values < 1.69 ng/mL could be caused by misinterpretation of small bone lesions due to the missing anatomical information by evaluating single PET datasets. Thus, bone metastases might be misinterpreted as lymph node metastases due to their close anatomical location to the pelvic bone. The higher MRI false-positive rate in our study makes it difficult to assume a clear superiority of MRI regarding bone metastases. It should be mentioned, that the reference standard is only based on PET/MRI examinations that were evaluated on an expert level in consensus and potential existing cross-sectional imaging. Thus, due to missing long time follow-up, the reference standard has its weakness, especially with a focus on bone metastases and the underestimation of false-positive bone findings at MRI might be possible.
Based on these data, our study comprises two main messages that we believe to be important: First, 68 Ga-PSMA-11 PET/MRI is an excellent synergistic imaging modality in the setting of biochemical PCa recurrence, as both imaging components have their specific strengths. Second, as running a PET/MR system still comes at markedly higher costs compared to PET/CT and has limited availabilities, additional mpMRI of the pelvis is highly important after therapy, especially in cases where PET/CT showed no lesion of local recurrence. Generally, a combination of both modalities (PET/CT and mpMRI) seems to be favorable for patient management and is more easily assessable in clinical routine [37, 38]. This is also highlighted in the study of Sonni et al (2021), which presented a comparable performance of combined PET/CT and mpMRI to 68 Ga-PSMA-11 PET/MRI in the detection and intraprostatic localization of prostate cancer [38]. Especially in PSMA negativity of prostate cancer (approximately 10%), the multiparametric dataset and high soft tissue contrast of MRI are beneficial for detecting the recurrence of prostate cancer [39, 40]. In general, we would like to emphasize here that a high level of expertise in the evaluation of mpMRI of the prostate is key to its valuable use [41].
This study has some limitations. First, due to evolving image quality in mpMRI in the last decade, some of the included datasets have limited image quality (QUAL 3), bearing the problem that especially the ability to detect pelvic lymph node metastases by MRI might be underestimated. Furthermore, patients with RP did not undergo a contrast dynamic of the prostate fossa in the period of data acquisition, which was considered in the given QUAL score. Second, due to the retrospective design, we only had information about recurrence by PSA levels and no information about the risk category of initial PCa. Thus, a group comparison of risk categories was not possible at all. Third, the reference standard is limited due to missing long time follow-up. Due to the reduced number of patients included in this study, we describe non-significant results according to our data evaluation. Nevertheless, we can visualize trends according to the different subgroups. It should be mentioned, that this kind of PET/MRI data of patients with prostate cancer recurrence are rare. Further larger and possible multicenter studies are needed which might bring our results to a significant level.
Concluding, the MRI component shows its strength in detecting local recurrence of PCa whereas 68 Ga-PSMA-11 PET component shows its strength in detecting lymph node metastases, especially for patients with PSA < 1.69 ng/mL without significant statistical staging differences. Nonetheless, the results support the combination of both imaging components for disease localization at PCa recurrence.
Abbreviations
- 68 Ga:
-
68Gallium
- ADC:
-
Apparent diffusion coefficient
- DWI:
-
Diffusion-weighted imaging
- mpMRI :
-
Multiparametric magnetic-resonance-imaging
- NPV:
-
Negative predictive value
- PCa:
-
Prostate cancer
- PET/MRI:
-
Positron-emission tomography/magnetic resonance imaging
- PPV:
-
Positive predictive value
- PROMISE:
-
Prostate cancer molecular imaging standardized evaluation
- PSA:
-
Prostate-specific antigen
- PSMA:
-
Prostate-specific membrane antigen
- QUAL:
-
MRI imaging quality score
- RP:
-
Radical prostatectomy
- RT:
-
Radiotherapy
References
EAU Guidelines Office. EAU-Guidelines. Edn. presented at the EAU Annual Congress Amsterdam 2022. ISBN 978–94–92671–16–5.
Suardi N, Porter CR, Reuther AM et al (2008) A nomogram predicting long-term biochemical recurrence after radical prostatectomy. Cancer 112:1254–1263
Chun FKH, Graefen M, Zacharias M et al (2006) Anatomic radical retropubic prostatectomy—long-term recurrence-free survival rates for localized prostate cancer. World J Urol 24:273–280
Cookson MS, Aus G, Burnett AL et al (2007) Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American Urological Association Prostate Guidelines for Localized Prostate Cancer Update Panel report and recommendations for a standard in the reporting of surgical outcomes. J Urol 177:540–545
De Visschere PJL, Standaert C, Fütterer JJ et al (2019) A systematic review on the role of imaging in early recurrent prostate cancer. Eur Urol Oncol 2:47–76
Ekmekcioglu Ö, Busstra M, Klass ND, Verzijlbergen F (2019) Bridging the imaging gap: PSMA PET/CT has a high impact on treatment planning in prostate cancer patients with biochemical recurrence—a narrative review of the literature. J Nucl Med 60:1394–1398
Fendler WP, Calais J, Eiber M et al (2019) Assessment of 68Ga-PSMA-11 PET accuracy in Localizing Recurrent Prostate Cancer: A Prospective Single-Arm Clinical Trial. JAMA Oncol 5:856–863
Fendler WP, Eiber M, Beheshti M et al (2023) PSMA PET/CT: joint EANM procedure guideline/SNMMI procedure standard for prostate cancer imaging 2.0. Eur J Nucl Med Mol Imaging 50(5):1466–1486. https://doi.org/10.1007/s00259-022-06089-w
Hope TA, Eiber M, Armstrong WR et al (2021) Diagnostic accuracy of 68Ga-PSMA-11 PET for pelvic nodal metastasis detection prior to radical prostatectomy and pelvic lymph node dissection: a multicenter prospective phase 3 imaging trial. JAMA Oncol 7:1635–1642
Freitag MT, Radtke JP, Afshar-Oromieh A et al (2017) Local recurrence of prostate cancer after radical prostatectomy is at risk to be missed in 68Ga-PSMA-11-PET of PET/CT and PET/MRI: comparison with mpMRI integrated in simultaneous PET/MRI. Eur J Nucl Med Mol Imaging 44:776–787
Achard V, Lamanna G, Denis A et al (2019) Recurrent prostate cancer after radical prostatectomy: restaging performance of 18F-choline hybrid PET/MRI. Med Oncol 36:67
Wieder H, Beer A, Holzapfel K et al (2017) 11C-choline PET/CT and whole-body MRI including diffusion-weighted imaging for patients with recurrent prostate cancer. Oncotarget 8:66516–66527
Barchetti F, Stagnitti A, Megna V et al (2016) Unenhanced whole-body MRI versus PET-CT for the detection of prostate cancer metastases after primary treatment. Eur Rev Med Pharmacol Sci 20:3770–3776
Schwenzer NF, Pfannenberg C, Reischl G, Werner MK, Schmidt H (2012) Einsatz von MR/PET in der onkologischen Bildgebung. Rofo 184:780–787
Zhang-Yin J, Montravers F, Montagne S, Hennequin C, Renard-Penna R (2022) Diagnosis of early biochemical recurrence after radical prostatectomy or radiation therapy in patients with prostate cancer: state of the art. Diagn Interv Imaging 103:191–199
Evangelista L, Zattoni F, Cassarino G et al (2021) PET/MRI in prostate cancer: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging 48:859–873
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194
Giganti F, Allen C, Emberton M, Moore CM, Kasivisvanathan V (2020) Prostate Imaging Quality (PI-QUAL): a new quality control scoring system for multiparametric magnetic resonance imaging of the prostate from the PRECISION trial. Eur Urol Oncol 3:615–619
Kirchner J, O’Donoghue JA, Becker AS, Ulaner GA (2021) Improved image reconstruction of 89Zr-immunoPET studies using a Bayesian penalized likelihood reconstruction algorithm. EJNMMI Physics 8:6
Jannusch K, Lindemann ME, Bruckmann NM et al (2023) Towards a fast PET/MRI protocol for breastcancer imaging: maintaining diagnostic confidence while reducing PET and MRI acquisition times. Eur Radiol 33(9):6179–6188. https://doi.org/10.1007/s00330-023-09580-6
Eiber M, Herrmann K, Calais J et al (2018) Prostate Cancer Molecular Imaging Standardized Evaluation (PROMISE): proposed miTNM classification for the interpretation of PSMA-ligand PET/CT. J Nucl Med 59:469–478
Valentin B, Arsov C, Ullrich T et al (2022) Comparison of 3 T mpMRI and pelvic CT examinations for detection of lymph node metastases in patients with prostate cancer. Eur J Radiol 147:110110
Beiderwellen K, Grueneisen J, Ruhlmann V et al (2015) [18F]FDG PET/MRI vs. PET/CT for whole-body staging in patients with recurrent malignancies of the female pelvis: initial results. Eur J Nucl Med Mol Imaging 42:56–65
Kirchner J, Deuschl C, Schweiger B et al (2017) Imaging children suffering from lymphoma: an evaluation of different 18F-FDG PET/MRI protocols compared to whole-body DW-MRI. Eur J Nucl Med Mol Imaging 44:1742–1750
Sawicki LM, Grueneisen J, Schaarschmidt BM et al (2016) Evaluation of 18F-FDG PET/MRI, 18F-FDG PET/CT, MRI, and CT in whole-body staging of recurrent breast cancer. Eur J Radiol 85:459–465
Buchbender C, Hartung-Knemeyer V, Beiderwellen K et al (2013) Diffusion-weighted imaging as part of hybrid PET/MRI protocols for whole-body cancer staging: does it benefit lesion detection? Eur J Radiol 82:877–882
Cornford P, van den Bergh RC, Briers E et al (2021) EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer. Part II—2020 update: treatment of relapsing and metastatic prostate cancer. Eur Urol 79:263–282
Panebianco V, Barchetti F, Musio D et al (2014) Advanced imaging for the early diagnosis of local recurrence prostate cancer after radical prostatectomy. Biomed Res Int 2014:827265
Radzina M, Tirane M, Roznere L et al (2020) Accuracy of (68)Ga-PSMA-11 PET/CT and multiparametric MRI for the detection of local tumor and lymph node metastases in early biochemical recurrence of prostate cancer. Am J Nucl Med Mol Imaging 10:106–118
Glemser PA, Rotkopf LT, Ziener CH et al (2022) Hybrid imaging with [68Ga]PSMA-11 PET-CT and PET-MRI in biochemically recurrent prostate cancer. Cancer Imaging 22:53
Giesel FL, Hadaschik B, Cardinale J et al (2017) F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. Eur J Nucl Med Mol Imaging 44:678–688
Schilham MGM, Zamecnik P, Privé BM et al (2021) Head-to-head comparison of 68Ga-prostate-specific membrane antigen PET/CT and ferumoxtran-10–enhanced MRI for the diagnosis of lymph node metastases in prostate cancer patients. J Nucl Med 62:1258–1263
Hövels AM, Heesakkers RAM, Adang EM et al (2008) The diagnostic accuracy of CT and MRI in the staging of pelvic lymph nodes in patients with prostate cancer: a meta-analysis. Clin Radiol 63:387–395
Freitag MT, Radtke JP, Hadaschik BA et al (2016) Comparison of hybrid 68Ga-PSMA PET/MRI and 68Ga-PSMA PET/CT in the evaluation of lymph node and bone metastases of prostate cancer. Eur J Nucl Med Mol Imaging 43:70–83
Rajarubendra N, Bolton D, Lawrentschuk N (2010) Diagnosis of Bone Metastases in Urological Malignancies—An Update. Urology 76:782–790
Zacho HD, Nielsen JB, Afshar-Oromieh A et al (2018) Prospective comparison of (68)Ga-PSMA PET/CT, (18)F-sodium fluoride PET/CT and diffusion weighted-MRI at for the detection of bone metastases in biochemically recurrent prostate cancer. Eur J Nucl Med Mol Imaging 45:1884–1897
de Galiza Barbosa F, Queiroz MA, Nunes RF, Marin JFG, Buchpiguel CA, Cerri GG (2018) Clinical perspectives of PSMA PET/MRI for prostate cancer. Clinics (Sao Paulo) 73(suppl 1):e586s. https://doi.org/10.6061/clinics/2018/e586s
Sonni I, Felker ER, Lenis AT et al (2022) Head-to-head comparison of (68)Ga-PSMA-11 PET/CT and mpMRI with a histopathology gold standard in the detection, intraprostatic localization, and determination of local extension of primary prostate cancer: results from a prospective single-center imaging trial. J Nucl Med 63:847–854
Ferraro DA, Rüschoff JH, Muehlematter UJ et al (2020) Immunohistochemical PSMA expression patterns of primary prostate cancer tissue are associated with the detection rate of biochemical recurrence with (68)Ga-PSMA-11-PET. Theranostics 10:6082–6094
Yaxley JW, Raveenthiran S, Nouhaud FX et al (2019) Risk of metastatic disease on (68) gallium-prostate-specific membrane antigen positron emission tomography/computed tomography scan for primary staging of 1253 men at the diagnosis of prostate cancer. BJU Int 124:401–407
de Rooij M, Israël B, Tummers M et al (2020) ESUR/ESUI consensus statements on multi-parametric MRI for the detection of clinically significant prostate cancer: quality requirements for image acquisition, interpretation and radiologists’ training. Eur Radiol 30:5404–5416
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Kai Jannusch.
Conflict of interest
Boris Hadaschik reports personal fees and non-financial support from ABX, Amgen, AAA/Novartis, Bayer, BMS, Janssen, Lightpoint Medical, Inc, MSD, and Pfizer, grants from German Research Foundation, all outside the submitted work.
Wolfgang P. Fendler reports fees from SOFIE Bioscience (research funding), Janssen (consultant, speaker), Calyx (consultant, image review), Bayer (consultant, speaker, research funding), Novartis (speaker), and Telix (speaker) outside of the submitted work.
The other authors have no relevant financial or non-financial interests to disclose.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all patients in this study.
Ethical approval
Institutional Review Board approval was obtained (University of Duisburg-Essen (study number 11–4822-BO)).
Study subjects or cohorts overlap
No study subjects or cohorts have been previously reported.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jannusch, K., Bruckmann, N.M., Morawitz, J. et al. Recurrent prostate cancer: combined role for MRI and PSMA-PET in 68Ga-PSMA-11 PET/MRI. Eur Radiol 34, 4789–4800 (2024). https://doi.org/10.1007/s00330-023-10442-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10442-4