Abstract
Objectives
To investigate the effect of the phantom-based correction method for standardizing myocardial native T1 and extracellular volume fraction (ECV) in healthy subjects.
Methods
Seventy-one healthy asymptomatic adult (≥ 20 years) volunteers of five different age groups (34 men and 37 women, 45.5 ± 15.5 years) were prospectively enrolled in three academic hospitals. Cardiac MRI including Modified Look - Locker Inversion recovery T1 mapping sequence was performed using a 3-Tesla system with a different type of scanner for each hospital. Native T1 and ECV were measured in the short-axis T1 map and analyzed for mean values of the 16 entire segments. The myocardial T1 value of each subject was corrected based on the site-specific equation derived from the T1 Mapping and ECV Standardization phantom. The global native T1 and ECV were compared between institutions before and after phantom-based correction, and the variation in native T1 and ECV among institutions was assessed using a coefficient of variation (CoV).
Results
The global native T1 value significantly differed between the institutions (1198.7 ± 32.1 ms, institution A; 1217.7 ± 39.9 ms, institution B; 1232.7 ± 31.1 ms, institution C; p = 0.002), but the mean ECV did not (26.6–27.5%, p = 0.355). After phantom-based correction, the global native T1 and ECV were 1289.7 ± 32.4 ms and 25.0 ± 2.7%, respectively, and CoV for native T1 between the three institutions decreased from 3.0 to 2.5%. The corrected native T1 value did not significantly differ between institutions (1284.5 ± 31.5 ms, institution A; 1296.5 ± 39.1 ms, institution B; 1291.3 ± 29.3 ms, institution C; p = 0.440), and neither did the ECV (24.4–25.9%, p = 0.078).
Conclusions
The phantom-based correction method can provide standardized reference T1 values in healthy subjects.
Key Points
• After phantom-based correction, the global native T1 of 16 entire myocardial segments on 3-T cardiac MRI is 1289.4 ± 32.4 ms, and the extracellular volume fraction was 25.0 ± 2.7% for healthy subjects.
• After phantom - based correction was applied, the differences in the global native T1 among institutions became insignificant, and the CoV also decreased from 3.0 to 2.5%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial tissue characterization by T1 mapping and estimation of native T1 and extracellular volume (ECV) by cardiac magnetic resonance imaging (CMR) are important for diagnosing and predicting the prognosis of various cardiovascular diseases [1,2,3]. Assessment of the presence and extent of myocardial abnormalities such as interstitial fibrosis using CMR may provide a surrogate endpoint in clinical trials [4]. However, the application of T1 mapping in multi-institutional, large-scale clinical trials is currently limited because the accuracy and precision of T1 mapping values, especially those of the native T1, vary depending on multiple factors [5,6,7,8]. For example, imaging sequence, field strength, temperature, manufacturer-specific hardware design of the CMR system, and even installation sites of CMR can affect estimated values from T1 mapping and normal reference ranges.
Therefore, the consensus statement from the society of cardiovascular magnetic resonance recommends that a local reference range from healthy controls or patients without other signs or history of myocardial disease should be primarily used for native T1 mapping [1]. However, even site-specific T1 measurement values cannot allow direct comparison and integration of results between different sites or CMR systems. To date, several methods have been adopted to standardize the analysis and reporting of T1 and ECV, such as the use of a phantom-based quality assurance system [9], z-score normalization [10], and clustered structuring [11]. However, none of these methods has been accepted as a sole strategy for the standardization of T1 mapping in a clinical setting. Recently, phantom-based quality assurance has been suggested for standardized myocardial T1 measurement [12, 13]. Consistent T1/T2 relaxation time can be obtained for each tube of T1 Mapping and ECV Standardization (T1MES) phantom if chemical stability and temperature dependence are guaranteed. Therefore, we hypothesized that correction of T1 and ECV from T1 mapping sequences of healthy human subjects based on the T1 from a standardized phantom might reduce variation of measurements.
Therefore, we aimed to investigate the effect of the phantom-based correction method for standardizing myocardial T1 measurement in healthy subjects from multiple institutions and provide standardized reference values of myocardial native T1 and ECV.
Materials and methods
Study population
This prospective study was approved by the institutional review boards of the participating hospitals. Subjects were enrolled after obtaining written informed consent to participate in this study. From December 2019 to April 2021, healthy asymptomatic adult ( ≥ 20 years) volunteers of five different age groups (20–29 years, 30–39 years, 40–49 years, 50–59 years, and 60–79 years) were prospectively enrolled in three academic hospitals (Fig. 1). The target number of subjects was 14 (7 males and 7 females) per age group, which was determined by referencing the number of healthy subjects in similar researches (9–11 subjects per age group) [14, 15]. Prior to inclusion and CMR, all subjects underwent a clinical examination for symptoms of cardiovascular disease and assessment of medical history and cardiovascular risk factors, such as smoking, hypertension (systolic and diastolic blood pressure > 90mmHg/90 mmHg with home - based remedies or drug treatment), hyperlipidemia, atrial fibrillation, diabetes mellitus, obesity (BMI > 30 kg/m2), and family history of cardiovascular disease (acute coronary syndrome or coronary revascularization in first - degree relatives < 65 years old). For screening, all subjects underwent ECG and blood sampling with measurement of estimated glomerular filtration rate (eGFR, Modification of Diet in Renal Disease formula), hematocrit, cholesterol, and N-terminal pro - brain natriuretic peptide prior to inclusion. Exclusion criteria were (1) any evidence of heart disease as indicated by clinical history or physical examination, (2) presence of abnormal ECG or hyperlipidemia (total cholesterol > 240 mg/dL) on screening, (3) pregnancy, (4) contraindications to CMR or expectation of having degraded CMR image quality (ferrometallic cerebral aneurysm clips, pacemaker or implantable defibrillator, or severe claustrophobia), or contraindications to injection of gadolinium-based contrast agent (renal insufficiency with eGFR < 45 mL/min/1.73m2), and (5) diabetes. After 96 healthy Korean subjects were screened, 20 subjects were excluded due to screening failure (15 with hyperlipidemia, 2 with abnormal ECG, 2 with hypertension, and 1 who did not meet the age criteria), and 5 subjects withdrew their informed consents after study participation. The final population consisted of 71 participants (34 males, mean age 45.5 ± 15.5 years; 29 subjects from institution A, 16 subjects from institution B, and 26 subjects from institution C), with 14 subjects (7 males and 7 females) per age group between 20–29 and 50–59 years and 15 subjects (6 males and 9 females) in the age group of 60–79 years.
CMR acquisition for healthy human subjects
At all three participating institutions, CMR was performed using a 3-Tesla (T) system (Siemens 3T Prismafit for Institution A, Siemens 3T Verio for Institution B, and Siemens 3T SKYRA for Institution C). The CMR acquisition parameters for cine imaging and T1 mapping are described in Supplementary Material. To assess left ventricular (LV) myocardial function and mass, short-axis images of the LV were acquired using a cine balanced steady-state free precession (bSSFP) sequence [16]. Three short-axis Modified Look-Locker Inversion-recovery (MOLLI) images at the base, mid-cavity, and apex were acquired for native T1 mapping [16, 17]. Then, a total dose of 0.1 mmol/kg gadolinium agent (Uniray, gadoterate meglumine, Dongkook Pharmaceutical Co., Ltd.) was injected. Ten minutes after contrast injection, post-contrast MOLLI T1 mapping was acquired for T1 determination in an identical location as for native T1 mapping.
Image acquisition for T1 mapping and ECV standardization phantom
We developed a novel method using the T1MES phantom. The process of image acquisition and T1 correction based on phantom are shown in Fig. 2. The T1MES phantom was scanned at each institution within a month in December 2019, when the clinical study started. The phantom was employed to measure the error in T1 measurement in three institutions with the MOLLI T1 mapping protocol based on the default MOLLI protocol provided by the CMR manufacturer (Siemens Healthineers) with adjustment of field of view and without other voluntary modification of scan parameters.
Diagram for the T1 map correction process. A T1 map was scanned with a T1MES phantom. The T1 value of the T1MES phantom provided by the manufacturer was considered as ground-truth T1, and the correction function was calculated based on the polynomial regression between the acquired T1 value and the ground-truth T1 value. The correction function was applied to the T1 maps of healthy human subjects to reduce the variation in T1 measurement. T1MES, T1 Mapping and ECV Standardization
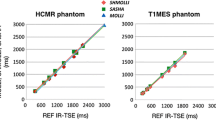
To measure the gold-standard T1 (T1GS) of the T1MES phantom in each institution, the inversion-recovery prepared turbo spin-echo [9] and the MOLLI sequence were used (Supplementary Table 1). Other scan considerations, such as setting the position in the iso-center, shim volume, and simulation ECG, were according to the instruction of the T1MES manual [18]. The ground-truth T1 (T1GT) of this T1MES phantom was regarded as the T1 described in the manual by the manufacturer.
Phantom-based T1 correction
To reduce the variation in the T1, three correction methods were considered (Supplementary Table 2). First, a gold-standard T1-based correction function (GC) was calculated by multiple polynomial regression with T1GS and T1GT of the T1MES phantom. Second, a MOLLI T1-based correction function (MC) was calculated with the T1 on MOLLI (T1ML) and T1GT. Last, an internal reference T1-based correction function (IC) was calculated with the T1ML and the T1GS. In particular, the MC and IC methods were subdivided according to whether the RR interval (RRI) of the subject was considered. When the RRI of each subject was considered (adaptive RRI), the correction function was calculated using a T1ML with an RRI close to the RRI of the subject (Supplementary Table 3). Otherwise, a T1ML with an RRI of 900 ms (static RRI) was used (Supplementary Table 4).
First-, second-, and third-order correction equations were applied to each correction method as follows:
where T1u is the uncorrected T1, T1c is the corrected T1, and a, b, c, and d are coefficients of the correction function according to each correction method (Supplementary Table 3 and 4). We chose the equation that showed the lowest coefficient of variation (CoV, standard deviation/mean) after correction.
CMR analysis
CMR images were anonymized and analyzed independently by two experienced observers (Y.J.S. and B.W.C., cardiac radiologists with 8 and 21 years of CMR experience, respectively) who were blinded to the clinical data. Cine imaging and T1 map images were analyzed using commercial software (cvi42 image analysis software, Circle Cardiovascular Imaging Inc.) (Supplementary Methods).
On cine bSSFP images, the endocardial and epicardial contours of the LV were semi-automatically drawn with manual adjustments when needed. LV end-diastolic volume (EDV) and end-systolic volume (ESV) were calculated using the modified Simpson method and were indexed to body surface area. LV ejection fraction was calculated as (EDV-ESV)/EDV.
Native and post-contrast T1 map images were generated by fitting pixels to the equation s(t) = a – b exp. (t/T1*), and T1 = T1*((b/a−1), where a and b are constants, t is time, and s(t) is the signal intensity at time t. On T1 map images, endocardial and epicardial contouring of the LV was performed semi-automatically, and manual adjustments were applied when needed. Native and post-contrast blood T1 times were measured on a region of interest drawn in the center of the blood pool. Native and post-contrast T1 values were measured in 16 AHA segments in the short-axis view of LV [19]. The myocardial ECV was calculated using the following equation [20]:
Native T1 and ECV fraction were analyzed as the mean of the 16 entire segments (global) and mid septum, after the exclusion of segments with image artifacts (e.g., off-resonance or partial volume artifact) that caused significant deterioration in T1 measurement.
Statistical analysis
Statistical analyses were performed using MedCalc for Windows version 19.1.0.0 (MedCalc Software) and R (version 4.0.2, R Foundation). Continuous variables are expressed as the mean ± standard deviation or median with 25th to 75th percentile, and categorical variables are shown as counts and percentages. Categorical variables were compared using the χ2 or Fischer’s exact test. Continuous variables were compared among groups using ANOVA for normally distributed data and the Kruskal-Wallis test for non-normally distributed data. T1 mapping results were excluded from the analysis if measured T1 values were estimated as outliers by the Tukey method [21, 22]. Variations in native T1 and ECV fraction among institutions were compared before and after phantom-based correction using a CoV. Inter-observer reproducibility of T1 times and ECV was assessed using an intraclass correlation coefficient. A probability value less than 0.05 was considered statistically significant, and a Bonferroni-adjusted post hoc probability value of less than 0.02 was considered statistically significant for comparison between the three institutions.
Results
Study population
The baseline characteristics of the 71 subjects are shown in Table 1. No subject had a history of stroke, chronic obstructive pulmonary disease, or sleep apnea syndrome or presented hemochromatosis or anemia on the blood test.
The CMR examination was successfully completed in all subjects, but 2 patients (a 54-year-old male in institution A and a 29-year-old female in institution B) were excluded from the analysis of T1 mapping because their measured T1 values were estimated as outliers due to image artifacts. All participants had normal LV function on cine imaging (Supplementary Table 5). Artifacts precluded analysis of native T1 in 67 segments of 25 subjects and 83 segments of 35 subjects in post-contrast T1 maps, resulting in missing ECV in 111 segments of 41 subjects. Inter-observer agreement of measurements on T1 map was excellent for both native T1 and ECV (intraclass correlation coefficient 0.993 [95% confidence interval 0.989–0.996] and 0.998 [95% confidence interval 0.997–0.999]), respectively).
Normal T1 values before and after phantom-based correction
The MC2 method (second-order correction equation with MC method) with static RRI was used for the correction of native and post-contrast T1 map images because the method showed the greatest decrease in the CoV of native T1 map in healthy human subjects among various correction methods (Fig. 3). Correction equations for myocardial native T1 and post-contrast T1 map for each institution are provided in Table 2.
CoV of the native T1 map using various correction methods. The MC2S (MOLLI T1 map-based second-degree correction function with static 900 ms RR interval) method had the lowest CoV compared to other correction methods on the (A) entire myocardial segments and (B) mid septum. The CoV decreased from 3.0 to 2.5% on the entire myocardial segments and from 2.96 to 2.48% on the mid septum (red arrow). CoV, coefficient of variation; MOLLI, Modified Look-Locker Inversion-recovery
The mean global native T1 and ECV fraction in 69 subjects are shown in Table 3. Mean RRI during the acquisition of native T1 and post T1 mapping sequences was 918.8 ± 144.1 ms (range 659.0–1261.3 ms) and 922.3 ± 129.7 ms (range 714.3–1247.5 ms), respectively. Before the phantom-based correction, the global native T1 was significantly different between the three institutions (1198.7 ± 32.1 ms for institution A, 1217.7 ± 39.9 ms for institution B, and 1232.7 ± 31.1 ms for institution C; p = 0.002), but ECV was not significantly different between the institutions (26.6 ± 1.8% for institution A, 27.5 ± 3.6% for institution B, and 27.4 ± 2.5% for institution C; p = 0.355). After phantom-based correction, the global native T1 was not significantly different between the three institutions (1284.5 ± 31.5 ms for institution A, 1296.5 ± 39.1 ms for institution B, and 1291.3 ± 29.3 ms for institution C; p = 0.440), and ECV was also not significantly different between the institutions (24.4 ± 2.2% for institution A, 25.9 ± 3.7% for institution B, and 25.4 ± 2.6% for institution C; p = 0.078). The mean of the corrected native T1 and ECV in 69 subjects were 1289.4 ± 32.4 ms and 25.0 ± 2.7%, respectively. After phantom-based correction, the CoV for the native T1 between the three institutions decreased from 3.0 to 2.5%.
In the measurement of the mid septum, native T1 was significantly different between the three institutions (1210.7 ± 35.0 ms for institution A, 1227.1 ± 34.8 ms for institution B, and 1244.2 ± 31.5 ms for institution C; p = 0.004) before phantom-based correction, but ECV was not significantly different between the institutions (26.7 ± 1.9% for institution A, 27.4 ± 3.1% for institution B, and 27.8 ± 2.5% for institution C; p = 0.079). After phantom-based correction, the mean native T1 of the mid septum was not significantly different between the three institutions (1296.2 ± 34.2 ms for institution A, 1305.6 ± 33.9 ms for institution B, and 1302.1 ± 29.7 ms for institution C; p = 0.498), and ECV was also not significantly different between the institutions (24.2 ± 1.9% for institution A, 25.6 ± 3.1% for institution B, and 25.8 ± 2.7% for institution C; p = 0.056). After phantom-based correction, the CoV for the native T1 between the three institutions decreased from 3.0 to 2.6%.
Discussion
Our study demonstrates that the phantom-based T1 correction method can reduce the inter-institutional variation in native T1 and ECV measurements on myocardial T1 mapping. After phantom-based correction, the global native T1 on 3-T CMR is 1289.4 ± 32.4 ms, and the ECV was 25.0 ± 2.7% for healthy Korean subjects.
Previous studies have reported normal reference ranges of native T1 and ECV in healthy subjects on CMR obtained at individual institutions using 1.5-T [23,24,25,26,27] or 3-T scanners [14, 27, 28]. Due to the variety of factors affecting the T1 measurements, the published normal reference ranges of native T1 are heterogeneous among studies [6, 7]. Therefore, it is difficult to benchmark those values across different institutions. Moreover, the variations in measurements have hindered multi-institutional studies for myocardial T1 mapping, and such multi-institutional studies can be conducted only when all the institutions in the study have a uniform imaging setup with the same type of scanner and pulse sequence [2, 27].
Compared to previous studies regarding the reference T1 on CMR, our study has two main strengths. First, we reported the myocardial T1 in healthy Korean subjects with a sufficient sample size (n = 71). As ethnicity may affect the myocardial T1 and ECV similarly as it affects the LV volume and mass [29], defining normal reference ranges in the Korean population will help develop future studies to investigate CMR T1 mapping. Although some previous studies have reported native T1 and ECV in healthy volunteers in Korea [30,31,32,33], the studies conducted thus far comprised relatively small control groups (n < 30) for comparison against patients with cardiovascular disease. Second, this is a multi-institutional study conducted in three different institutions with different scanner types and provides standardized normal native T1 and ECV by using the phantom-based correction method. After phantom-based correction was applied, the differences in the mean native T1 among institutions became insignificant, and the CoV also decreased. Our results suggest that the phantom-based correction method is effective for the standardization of myocardial T1 achieved by reducing measurement variation.
We suggest that the phantom-based T1 correction method can reduce the variation in T1 measurement. Since the T1MES phantom program was established [9], repeatability of T1 measurement using the T1MES phantom has been demonstrated across centers with different field strengths, sequences, and scanners [12], and the T1MES phantom has been found to be useful for quality assurance in a multi-center setting. We employed this well-established phantom for the correction of the myocardial T1. For this purpose, we considered three types of correction methods (systemic, reference, and internal) with combinations of heart rate condition (static or adaptive RRI) and degree of correction equations (first-, second-, and third-degree equations). After several preliminary examinations, we concluded that the phantom-based T1 correction is feasible, and the MC method with a second-degree equation and static RRI was the most suitable for T1 correction because this method reduced variation among measurements made in the three participating institutions to the greatest extent. We expect that values obtained from different institutions might be interchangeable if our method would be validated in other sites with CMR scanners from different vendors.
Our study has several limitations. First, we included subjects from three institutions with different types of CMR scanners, but all of them were 3-T scanners from the same vendor and used the same MOLLI sequence. It is necessary to validate our findings using scanners of other vendors, pulse sequences, and 1.5-T to expand the application of our method. Second, it is unclear whether T1 variations among institutions originate from inter-subject variations or other factors, such as the CMR scanner, because different individuals were included from each institution. To validate our methods and exclude the effect of inter-subject variation, acquiring T1 in the same subject with scanners from multiple vendors and based on pulse sequences are needed. Finally, the time interval of blood sampling for hematocrit measurement between CMR acquisition was longer than 1 day in 57.7% (41 of 71) subjects, which might have diminished the reliability of ECV calculation [1]. However, some studies suggested that hematocrit measured on a different day from CMR could be useful for ECV calculation without a significant difference in the calculated value [34]. We assumed that our results for ECV may not have significantly deviated from those obtained if the hematocrit had been measured on the same day as CMR.
In conclusion, the standardized reference value of myocardial native T1 and ECV in healthy Korean subjects can be provided using the phantom-based correction method as it reduces variation in T1 measurement. Our phantom-based correction method may allow standardization of myocardial T1, which can facilitate the application of T1 mapping in multi-institutional, large-scale clinical trials.
Abbreviations
- CMR:
-
Cardiac magnetic resonance imaging
- CoV:
-
Coefficient of variation
- ECG:
-
Electrocardiogram
- ECV:
-
Extracellular volume
- eGFR:
-
Estimated glomerular filtration rate
- LV:
-
Left ventricular
- MOLLI:
-
Modified Look-Locker Inversion-recovery
- RRI:
-
RR interval
- T1MES:
-
T1 Mapping and ECV Standardization
References
Messroghli DR, Moon JC, Ferreira VM et al (2017) Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson 19:75
Everett RJ, Treibel TA, Fukui M et al (2020) Extracellular myocardial volume in patients with aortic stenosis. J Am Coll Cardiol 75:304–316
Treibel TA, Fridman Y, Bering P et al (2020) Extracellular volume associates with outcomes more strongly than native or post-contrast myocardial T1. JACC Cardiovasc Imaging 13:44–54
Lewis GA, Dodd S, Naish JH, Selvanayagam JB, Dweck MR, Miller CA (2019) Considerations for clinical trials targeting the myocardial interstitium. JACC Cardiovasc Imaging 12:2319–2331
Kellman P, Hansen MS (2014) T1-mapping in the heart: accuracy and precision. J Cardiovasc Magn Reson 16:2
Vo HQ, Marwick TH, Negishi K (2020) Pooled summary of native T1 value and extracellular volume with MOLLI variant sequences in normal subjects and patients with cardiovascular disease. Int J Cardiovasc Imaging 36:325–336
Gottbrecht M, Kramer CM, Salerno M (2019) Native T1 and extracellular volume measurements by cardiac MRI in healthy adults: a meta-analysis. Radiology 290:317–326
Roujol S, Weingärtner S, Foppa M et al (2014) Accuracy, precision, and reproducibility of four T1 mapping sequences: a head-to-head comparison of MOLLI, ShMOLLI, SASHA, and SAPPHIRE. Radiology 272:683–689
Captur G, Gatehouse P, Keenan KE et al (2016) A medical device-grade T1 and ECV phantom for global T1 mapping quality assurance-the T1 Mapping and ECV Standardization in cardiovascular magnetic resonance (T1MES) program. J Cardiovasc Magn Reson 18:58
Kranzusch R, Aus dem Siepen F, Wiesemann S et al (2020) Z-score mapping for standardized analysis and reporting of cardiovascular magnetic resonance modified Look-Locker inversion recovery (MOLLI) T1 data: Normal behavior and validation in patients with amyloidosis. J Cardiovasc Magn Reson 22:6
Popescu IA, Werys K, Zhang Q et al (2020) Standardization of T1-mapping in cardiovascular magnetic resonance using clustered structuring for benchmarking normal ranges. Int J Cardiol 326:220–225
Captur G, Bhandari A, Brühl R et al (2020) T(1) mapping performance and measurement repeatability: results from the multi-national T(1) mapping standardization phantom program (T1MES). J Cardiovasc Magn Reson 22:31
Zhang Q, Werys K, Popescu IA et al (2021) Quality assurance of quantitative cardiac T1-mapping in multicenter clinical trials - a T1 phantom program from the hypertrophic cardiomyopathy registry (HCMR) study. Int J Cardiol 330:251–258
Roy C, Slimani A, de Meester C et al (2017) Age and sex corrected normal reference values of T1, T2 T2* and ECV in healthy subjects at 3T CMR. J Cardiovasc Magn Reson 19:72
Dong Y, Yang D, Han Y et al (2018) Age and gender impact the measurement of myocardial interstitial fibrosis in a healthy adult chinese population: a cardiac magnetic resonance study. Front Physiol 9:140
Jo Y, Kim J, Park CH et al (2019) Guideline for cardiovascular magnetic resonance imaging from the Korean Society of Cardiovascular imaging-Part 1: Standardized protocol. Korean J Radiol 20:1313–1333
Kim PK, Hong YJ, Im DJ et al (2017) Myocardial T1 and T2 mapping: techniques and clinical applications. Korean J Radiol 18:113–131
Captur G GP, Pang W, Royet C, Moon J (2015) T1MES user manual. Available via https://redcaphh.ccloudservices.net/surveys/?s=dRcYg3HGz5. Accessed 4 January 2022
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542
Arheden H, Saeed M, Higgins CB et al (1999) Measurement of the distribution volume of gadopentetate dimeglumine at echo-planar MR imaging to quantify myocardial infarction: comparison with 99mTc-DTPA autoradiography in rats. Radiology 211:698–708
Tukey JW (1977) Exploratory data analysis. Addison-Wesley
Higgins DM, Keeble C, Juli C, Dawson DK, Waterton JC (2019) Reference range determination for imaging biomarkers: Myocardial T1. J Magn Reson Imaging 50:771–778
Piechnik SK, Ferreira VM, Lewandowski AJ et al (2013) Normal variation of magnetic resonance T1 relaxation times in the human population at 1.5 T using ShMOLLI. J Cardiovasc Magn Reson 15:13
Reiter U, Reiter G, Dorr K, Greiser A, Maderthaner R, Fuchsjager M (2014) Normal diastolic and systolic myocardial T1 values at 1.5-T MR imaging: correlations and blood normalization. Radiology 271:365–372
Liu JM, Liu A, Leal J et al (2017) Measurement of myocardial native T1 in cardiovascular diseases and norm in 1291 subjects. J Cardiovasc Magn Reson 19:74
Rosmini S, Bulluck H, Captur G et al (2018) Myocardial native T1 and extracellular volume with healthy ageing and gender. Eur Heart J Cardiovasc Imaging 19:615–621
Dabir D, Child N, Kalra A et al (2014) Reference values for healthy human myocardium using a T1 mapping methodology: results from the International T1 Multicenter cardiovascular magnetic resonance study. J Cardiovasc Magn Reson 16:69
von Knobelsdorff-Brenkenhoff F, Prothmann M, Dieringer MA et al (2013) Myocardial T1 and T2 mapping at 3 T: reference values, influencing factors and implications. J Cardiovasc Magn Reson 15:53
Natori S, Lai S, Finn JP et al (2006) Cardiovascular function in multi-ethnic study of atherosclerosis: normal values by age, sex, and ethnicity. AJR Am J Roentgenol 186:S357–S365
Youn JC, Hong YJ, Lee HJ et al (2017) Contrast-enhanced T1 mapping-based extracellular volume fraction independently predicts clinical outcome in patients with non-ischemic dilated cardiomyopathy: a prospective cohort study. Eur Radiol 27:3924–3933
Hwang IC, Kim HK, Park JB et al (2020) Aortic valve replacement-induced changes in native T1 are related to prognosis in severe aortic stenosis: T1 mapping cardiac magnetic resonance imaging study. Eur Heart J Cardiovasc Imaging 21:653–663
Hong YJ, Park CH, Kim YJ et al (2015) Extracellular volume fraction in dilated cardiomyopathy patients without obvious late gadolinium enhancement: comparison with healthy control subjects. Int J Cardiovasc Imaging 31(Suppl 1):115–122
Lee E, Kim PK, Choi BW, Jung JI (2020) Phantom-validated reference values of myocardial mapping and extracellular volume at 3T in healthy Koreans. Investig Magn Reson Imaging 24:141–153
Su MY, Huang YS, Niisato E et al (2020) Is a timely assessment of the hematocrit necessary for cardiovascular magnetic resonance-derived extracellular volume measurements? J Cardiovasc Magn Reson 22:77
Funding
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Ministry of Science and ICT (NRF-2018M3A9H6081483), by the DongKook Life Science. Co., Ltd, Republic of Korea, and Technology Development Program (S3033533) funded by the Ministry of SMEs and Startups (MSS, Korea).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is BWC.
Conflict of interest
Two authors (Pan Ki Kim and Byoung Wook Choi) are founders of Phantomics, Inc. (Seoul, Korea) and one author (Jinho Park) is an employee of the same company, but the company did not support this study. Other authors declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• experimental
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 56 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Suh, Y.J., Kim, P.K., Park, J. et al. Phantom-based correction for standardization of myocardial native T1 and extracellular volume fraction in healthy subjects at 3-Tesla cardiac magnetic resonance imaging. Eur Radiol 32, 8122–8130 (2022). https://doi.org/10.1007/s00330-022-08936-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08936-8