Abstract
Objectives
To evaluate quantitative parameters to identify the anatomic variation lumbosacral transitional vertebrae (LSTV) and compare them with the landmarks commonly used at present.
Methods
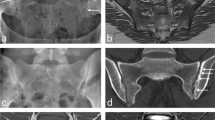
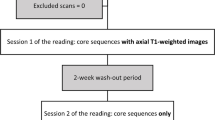
A total of 2,845 PET/CT scans were reviewed, and the patients with 23 and 25 presacral vertebrae were included. The quantitative parameters, including the anterior-edge vertebral angle (AVA) of the lowest lumbar-type vertebra, the ratio of the length of the inferior endplate to that of the superior endplate (RISE) of the uppermost sacral-type vertebra and the lumbosacral intervertebral disc angle (LSIVDA), and the anatomical landmarks, including the iliac crest tangent (ICT) level, the iliolumbar ligament (ILL) origin level and psoas proximal insertion, were all evaluated to determine their ability to identify LSTV.
Results
The values of AVA and RISE were significantly different between the LSTV group and the control group, and between subgroups of LSTV. The cutoff value for AVA was 73.0°, with an accuracy, sensitivity, and specificity of 91.1%, 77.5%, and 88.3%, and that for RISE was 0.79, with an accuracy, sensitivity, and specificity of 90.3%, 77.5%, and 94.2%, while that for LSIVDA was 14.15°, with an accuracy, sensitivity, and specificity of 75.9%, 65.7%, and 78.3%, to differentiate L5 sacralization from S1 lumbarization. For differentiating the controls from LSTV, the accuracy, sensitivity, and specificity of the ICT level and proximal psoas insertion were 78.0%, 70.2%, and 95.0%, versus 71.7%, 61.7%, and 94.0%.
Conclusions
Compared with the anatomical landmarks, the quantitative measurements at the lumbosacral junction, including AVA and RISE, may be more helpful for differentiating subgroups of LSTV especially if only lumbar spine imaging is available.
Key Points
• The quantitative parameters, the anterior-edge vertebral angle (AVA) of the lowest lumbar-type vertebra and the ratio of the length of the inferior endplate to that of the superior endplate (RISE) of the uppermost sacral-type vertebra, are more helpful for distinguishing L5 sacralization from S1 lumbarization than the previously proposed anatomic landmarks.
• AVA and RISE represent relevant changes in the curvature at the lumbosacral region and the shape of the transitional vertebral body, respectively.
• AVA and RISE are easily assessed, with high intra- and inter-reader reliability.





Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the ROC curve
- AVA:
-
Anterior-edge vertebral angle
- CI:
-
Confidence interval
- ICCs:
-
Intra-class correlation coefficients
- ICT:
-
Iliac crest tangent
- ILL:
-
Iliolumbar ligament
- LSIVDA:
-
Lumbosacral intervertebral disc angle
- LSTV:
-
Lumbosacral transitional vertebrae
- MPR:
-
Multiplanar reconstruction
- OR:
-
Odds ratios
- PET/CT:
-
Positron emission tomography combined with computerized tomography
- PSM:
-
Propensity score matching
- PSV:
-
Presacral vertebrae
- RISE:
-
Ratio of the length of the inferior endplate to that of the superior endplate
- ROC:
-
Receiver operating characteristic
- VR:
-
Volume-rendered
References
Jancuska JM, Spivak JM, Bendo JA (2015) A review of symptomatic lumbosacral transitional vertebrae: Bertolotti’s syndrome. Int J Spine Surg 9:42
Konin GP, Walz DM (2010) Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol 31:1778–1786
Lian J, Levine N, Cho W (2018) A review of lumbosacral transitional vertebrae and associated vertebral numeration. Eur Spine J 27:995–1004
Apazidis A, Ricart PA, Diefenbach CM, Spivak JM (2011) The prevalence of transitional vertebrae in the lumbar spine. Spine J 11:858–862
Bron JL, van Royen BJ, Wuisman PIJM (2007) The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg 73:687–695
Nardo L, Alizai H, Virayavanich W et al (2012) Lumbosacral transitional vertebrae: association with low back pain. Radiology 265:497–503
Paik NC, Lim CS, Jang HS (2013) Numeric and morphological verification of lumbosacral segments in 8280 consecutive patients. Spine (Phila Pa 1976) 38:E573–E578
Tang M, Yang X-f, Yang S-w et al (2014) Lumbosacral transitional vertebra in a population-based study of 5860 individuals: prevalence and relationship to low back pain. Eur J Radiol 83:1679–1682
Tucker BJ, Weinberg DS, Liu RW (2019) Lumbosacral transitional vertebrae: a cadaveric investigation of prevalence and relation to lumbar degenerative disease. Clin Spine Surg 32:E330–E334
Bertolotti M (1917) Contributo alla conoscenza dei vizi di differenziazione regionale del rachide con speciale riguardo all assimilazione sacrale della v. lombare. Radiol Med (Torino) 4:113–144
Apaydin M, Uluc ME, Sezgin G (2019) Lumbosacral transitional vertebra in the young men population with low back pain: anatomical considerations and degenerations (transitional vertebra types in the young men population with low back pain). Radiol Med 124:375–381
Hanhivaara J, Määttä JH, Niinimäki J, Nevalainen MT (2020) Lumbosacral transitional vertebrae are associated with lumbar degeneration: retrospective evaluation of 3855 consecutive abdominal CT scans. Eur Radiol 30:3409–3416
Bahadir Ulger FE, Illeez OG (2020) The effect of lumbosacral transitional vertebrae (LSTV) on paraspinal muscle volume in patients with low back pain. Acad Radiol 27:944–950
Aihara T, Takahashi K, Ogasawara A, Itadera E, Ono Y, Moriya H (2005) Intervertebral disc degeneration associated with lumbosacral transitional vertebrae: a clinical and anatomical study. J Bone Joint Surg Br 87:687–691
Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimäki H (2004) Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine (Phila Pa 1976) 29:200–205
Porter NA, Lalam RK, Tins BJ, Tyrrell PNM, Singh J, Cassar-Pullicino VN (2014) Prevalence of extraforaminal nerve root compression below lumbosacral transitional vertebrae. Skeletal Radiol 43:55–60
Kanematsu R, Hanakita J, Takahashi T, Minami M, Tomita Y, Honda F (2020) Extraforaminal entrapment of the fifth lumbar spinal nerve by nearthrosis in patients with lumbosacral transitional vertebrae. Eur Spine J 29:2215–2221
Shibayama M, Ito F, Miura Y, Nakamura S, Ikeda S, Fujiwara K (2011) Unsuspected reason for sciatica in Bertolotti’s syndrome. J Bone Joint Surg Br 93:705–707
Akbar JJ, Weiss KL, Saafir MA, Weiss JL (2010) Rapid MRI detection of vertebral numeric variation. AJR Am J Roentgenol 195:465–466
Mody MG, Nourbakhsh A, Stahl DL, Gibbs M, Alfawareh M, Garges KJ (2008) The prevalence of wrong level surgery among spine surgeons. Spine (Phila Pa 1976) 33:194–198
Hughes RJ, Saifuddin A (2006) Numbering of lumbosacral transitional vertebrae on MRI: role of the iliolumbar ligaments. AJR Am J Roentgenol 187:W59–W65
Peckham ME, Hutchins TA, Stilwill SE et al (2017) Localizing the L5 vertebra using nerve morphology on MRI: an accurate and reliable technique. AJNR Am J Neuroradiol 38:2008–2014
Ropars F, Mesrar J, Ognard J, Querellou S, Rousset J, Garetier M (2019) Psoas proximal insertion as a simple and reliable landmark for numbering lumbar vertebrae on MRI of the lumbar spine. Eur Radiol 29:2608–2615
Albano D, Messina C, Gambino A et al (2020) Segmented lordotic angles to assess lumbosacral transitional vertebra on EOS. Eur Spine J 29:2470–2476
Josiah DT, Boo S, Tarabishy A, Bhatia S (2017) Anatomical differences in patients with lumbosacral transitional vertebrae and implications for minimally invasive spine surgery. J Neurosurg Spine 26:137–143
Haffer H, Becker L, Putzier M et al (2021) Changes of fixed anatomical spinopelvic parameter in patients with lumbosacral transitional vertebrae: a matched pair analysis. Diagnostics (Basel) 11:59
Khalsa AS, Mundis GM Jr et al (2018) Variability in assessing spinopelvic parameters with lumbosacral transitional vertebrae: inter- and intraobserver reliability among spine surgeons. Spine (Phila Pa 1976) 43:813–816
Carrino JA, Campbell PD Jr et al (2011) Effect of spinal segment variants on numbering vertebral levels at lumbar MR imaging. Radiology 259:196–202
Farshad-Amacker NA, Aichmair A, Herzog RJ, Farshad M (2015) Merits of different anatomical landmarks for correct numbering of the lumbar vertebrae in lumbosacral transitional anomalies. Eur Spine J 24:600–608
Carapuço M, Nóvoa A, Bobola N, Mallo M (2005) Hox genes specify vertebral types in the presomitic mesoderm. Genes Dev 19:2116–2121
Thawait GK, Chhabra A, Carrino JA (2012) Spine segmentation and enumeration and normal variants. Radiol Clin North Am 50:587–598
Mahato NK (2010) Morphological traits in sacra associated with complete and partial lumbarization of first sacral segment. Spine J 10:910–915
Abola MV, Teplensky JR, Cooperman DR, Bauer JM, Liu RW (2019) Pelvic incidence in spines with 4 and 6 lumbar vertebrae. Global Spine J 9:708–712
Price R, Okamoto M, Le Huec JC, Hasegawa K (2016) Normative spino-pelvic parameters in patients with the lumbarization of S1 compared to a normal asymptomatic population. Eur Spine J 25:3694–3698
Yokoyama K, Kawanishi M, Yamada M et al (2016) Spinopelvic alignment and sagittal balance of asymptomatic adults with 6 lumbar vertebrae. Eur Spine J 25:3583–3588
Mahato NK (2011) Disc spaces, vertebral dimensions, and angle values at the lumbar region: a radioanatomical perspective in spines with L5-S1 transitions: clinical article. J Neurosurg Spine 15:371–379
Mahato NK (2013) Pars inter-articularis and laminar morphology of the terminal lumbar vertebra in lumbosacral transitional variations. N Am J Med Sci 5:357–361
Mahato NK (2011) Facet dimensions, orientation, and symmetry at L5-S1 junction in lumbosacral transitional States. Spine (Phila Pa 1976) 36:E569–E573
Mahato NK (2011) Pedicular anatomy of the first sacral segment in transitional variations of the lumbo-sacral junction. Spine (Phila Pa 1976) 36:E1187–E1192
Wellik DM, Capecchi MR (2003) Hox10 and Hox11 genes are required to globally pattern the mammalian skeleton. Science 301:363–367
Zhou PL, Moon JY, Tishelman JC et al (2018) Interpretation of spinal radiographic parameters in patients with transitional lumbosacral vertebrae. Spine Deform 6(5):587–592
Castellvi AE, Goldstein LA, Chan DP (1984) Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 9:493–495
French HD, Somasundaram AJ, Schaefer NR, Laherty RW (2014) Lumbosacral transitional vertebrae and its prevalence in the Australian population. Global Spine J 4:229–232
Tins BJ, Balain B (2016) Incidence of numerical variants and transitional lumbosacral vertebrae on whole-spine MRI. Insights Imaging 7:199–203
Elster AD (1989) Bertolotti’s syndrome revisited. Transitional vertebrae of the lumbar spine. Spine (Phila Pa 1976) 14:1373–1377
Gay RE, Ilharreborde B, Zhao K, Zhao C, An K-N (2006) Sagittal plane motion in the human lumbar spine: comparison of the in vitro quasistatic neutral zone and dynamic motion parameters. Clin Biomech (Bristol, Avon) 21:914–919
Yilgor C, Sogunmez N, Boissiere L et al (2017) Global Alignment and Proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99:1661–1672
Gündüz N, Durukan G, Eser MB, Aslan A, Kabaalioğlu A (2019) Role of iliac crest tangent in correct numbering of lumbosacral transitional vertebrae. Turk J Med Sci 49:184–189
Tokgoz N, Ucar M, Erdogan AB, Kilic K, Ozcan C (2014) Are spinal or paraspinal anatomic markers helpful for vertebral numbering and diagnosing lumbosacral transitional vertebrae? Korean J Radiol 15(2):258–266
Lee CH, Seo BK, Choi YC et al (2004) Using MRI to evaluate anatomic significance of aortic bifurcation, right renal artery, and conus medullaris when locating lumbar vertebral segments. AJR Am J Roentgenol 182(5):1295–1300
Tureli D, Ekinci G, Baltacioglu F (2014) Is any landmark reliable in vertebral enumeration? A study of 3.0-Tesla lumbar MRI comparing skeletal, neural, and vascular markers. Clin Imaging 38:792–796
Kershenovich A, Macias OM, Syed F, Davenport C, Moore GJ, Lock JH (2016) Conus medullaris level in vertebral columns with lumbosacral transitional vertebra. Neurosurgery 78:62–70
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Haitao Yang.
Conflict of interest
The authors declare no competing interests.
Statistics and biometry
The scientific guarantor of this publication has knowledge of statistics and we have consulted the specific statistical expertise for the investigation.
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Case-control study
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, S., Du, L., Liu, X. et al. Quantitative measurements at the lumbosacral junction are more reliable parameters for identifying and numbering lumbosacral transitional vertebrae. Eur Radiol 32, 5650–5658 (2022). https://doi.org/10.1007/s00330-022-08613-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08613-w