Abstract
Objective
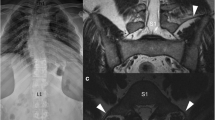
To evaluate the value of psoas muscle proximal insertion for correct numbering of the lumbar vertebrae in MRI, in particular in case of lumbosacral transitional vertebra (LSTV).
Methods
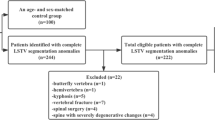
Two radiologists assessed 477 MRI scans of the lumbar spine with a sagittal localizer sequence on the whole spine for numbering vertebrae caudally from C2. Proximal insertion of the psoas was determined as the most proximal vertebra with psoas over half of its body on coronal T2 STIR sequence. The last lumbar vertebra was named considering both its number and the presence or absence of LSTV according to Castellvi classification. These same parameters were also assessed on 207 PET-CT scans of another cohort including the whole spine.
Results
Proximal insertion of the psoas was L1 in 94.1% of cases: 98.5% in case of modal anatomy, 81.4% in case of LSTV, and 51.7% in case of missing or supernumerary lumbar vertebra without LSTV. There was no statistically significant difference between MRI and CT data. The inter-reader agreement for determination of psoas proximal insertion was excellent (kappa = 0.96).
Conclusion
Proximal insertion of the psoas muscle is a helpful marker for correct numbering of the lumbar vertebrae in MRI and to detect a complete lumbosacral segmentation anomaly.
Key Points
• Proximal insertion of the psoas muscle can be easily identified on a coronal T2 STIR sequence.
• Psoas proximal insertion on the spine almost always designates the first lumbar vertebra and is helpful to accurately number all lumbar vertebrae, especially in case of lumbosacral transitional vertebra.
• Conversely, when psoas muscle does not insert five lumbar bodies above the apparent lumbosacral joint, the probability of variation in the number of lumbar vertebrae is high.




Similar content being viewed by others
Abbreviations
- HU:
-
Hounsfield units
- LSTV:
-
Lumbosacral transitional vertebra
- MRI:
-
Magnetic resonance imaging
- PACS:
-
Picture archiving and communication system
- PET-CT:
-
Positron emission tomography-computed tomography
- STIR:
-
Short tau inversion recovery
- TE:
-
Echo time
- TI:
-
Inversion time
- TR:
-
Repetition time
References
Malanga GA, Cooke PM (2004) Segmental anomaly leading to wrong level disc surgery in cauda equina syndrome. Pain Physician 7:107–110
Konin GP, Walz DM (2010) Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol 31:1778–1786
Paik NC, Lim CS, Jang HS (2013) Numeric and morphological verification of lumbosacral segments in 8280 consecutive patients. Spine (Phila Pa 1976) 38:E573–E578
Castellvi AE, Goldstein LA, Chan DP (1984) Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 9:493–495
Apazidis A, Ricart PA, Diefenbach CM, Spivak JM (2011) The prevalence of transitional vertebrae in the lumbar spine. Spine J 11:858–862
Hughes RJ, Saifuddin A (2004) Imaging of lumbosacral transitional vertebrae. Clin Radiol 59:984–991
Paik NC, Lim CS, Jang HS (2012) Numbering of vertebrae on MRI using a PACS cross-referencing tool. Acta Radiol 53:785–789
Akbar JJ, Weiss KL, Saafir MA, Weiss JL (2010) Rapid MRI detection of vertebral numeric variation. AJR Am J Roentgenol 195:465–466
Lee CH, Seo BK, Choi YC et al (2005) Using MRI to evaluate anatomic significance of aortic bifurcation, right renal artery, and conus medullaris when locating lumbar vertebral segments. AJR Am J Roentgenol 182:1295–1300
Tokgoz N, Ucar M, Erdogan AB, Kilic K, Ozcan C (2014) Are spinal or paraspinal anatomic markers helpful for vertebral numbering and diagnosing lumbosacral transitional vertebrae? Korean J Radiol 15:258–266
Farshad-Amacker NA, Aichmair A, Herzog RJ, Farshad M (2015) Merits of different anatomical landmarks for correct numbering of the lumbar vertebrae in lumbosacral transitional anomalies. Eur Spine J 24:600–608
Carrino JA, Campbell PD Jr, Lin DC et al (2011) Effect of spinal segment variants on numbering vertebral levels at lumbar MR imaging. Radiology 259:196–202
Nakajima A, Usui A, Hosokai Y et al (2014) The prevalence of morphological changes in the thoracolumbar spine on whole-spine computed tomographic images. Insights Imaging 5:77–83
Farshad-Amacker NA, Lurie B, Herzog RJ, Farshad M (2014) Is the iliolumbar ligament a reliable identifier of the L5 vertebra in lumbosacral transitional anomalies? Eur Radiol 24:2623–2630
O’Driscoll CM, Irwin A, Saifuddin A (1996) Variations in morphology of the lumbosacral junction on sagittal MRI: correlation with plain radiography. Skeletal Radiol 25:225–230
Wigh RE (1980) The thoracolumbar and lumbosacral transitional junctions. Spine (Phila Pa 1976) 5:215–222
Kershenovich A, Macias OM, Syed F, Davenport C, Moore GJ, Lock JH (2016) Conus medullaris level in vertebral columns with lumbosacral transitional vertebra. Neurosurgery 78:62–70
Lee CH, Seo BK, Choi YC et al (2004) Using MRI to evaluate anatomic significance of aortic bifurcation, right renal artery, and conus medullaris when locating lumbar vertebral segments. AJR Am J Roentgenol 182:1295–1300
Lee CH, Park CM, Kim KA et al (2007) Identification and prediction of transitional vertebrae on imaging studies: anatomical significance of paraspinal structures. Clin Anat 20:905–914
Hanson EH, Mishra RK, Chang DS et al (2010) Sagittal whole-spine magnetic resonance imaging in 750 consecutive outpatients: accurate determination of the number of lumbar vertebral bodies: clinical article. J Neurosurg Spine 12:47–55
Farshad-Amacker NA, Lurie B, Herzog RJ, Farshad M (2014) Interreader and intermodality reliability of standard anteroposterior radiograph and magnetic resonance imaging in detection and classification of lumbosacral transitional vertebra. Spine J 14:1470–1475
Hsieh CY, Vanderford JD, Moreau SR, Prong T (2000) Lumbosacral transitional segments: classification, prevalence, and effect on disk height. J Manipulative Physiol Ther 23:483–489
Tertti MO, Salminen JJ, Paajanen HE, Terho PH, Kormano MJ (1991) Low-back pain and disk degeneration in children: a case-control MR imaging study. Radiology 180:503–507
Gray H (1918) Anatomy of the human body. Lea and Febiger, Philadelphia
Le Double AF (1897) Treaty about variations of the human muscular system [in French]. Schleicher Frères, Paris
Laporte C, Albert JD, Duvauferrier R, Bertaud V, Gouillou M, Guillin R (2014) MRI investigation of radiating pain in the lower limbs: value of an additional sequence dedicated to the lumbosacral plexus and pelvic girdle. AJR Am J Roentgenol 203:1280–1285
Tureli D, Ekinci G, Baltacioglu F (2014) Is any landmark reliable in vertebral enumeration? A study of 3.0-Tesla lumbar MRI comparing skeletal, neural, and vascular markers. Clin Imaging 38:792–796
Acknowledgments
The authors thank Philippe Bruyant for his help with manuscript revision.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Garetier Marc.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Prospective and retrospective
• Observational
• Performed at one institution
Rights and permissions
About this article
Cite this article
Ropars, F., Mesrar, J., Ognard, J. et al. Psoas proximal insertion as a simple and reliable landmark for numbering lumbar vertebrae on MRI of the lumbar spine. Eur Radiol 29, 2608–2615 (2019). https://doi.org/10.1007/s00330-018-5798-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5798-z