Abstract
Objectives
The diffuse intrinsic pontine gliomas (DIPGs) are now defined by the type of histone H3 mutated at lysine 27. We aimed to correlate the multimodal MRI features of DIPGs, H3K27M mutant, with their histological and molecular characteristics.
Methods
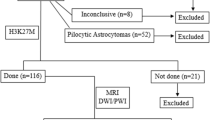
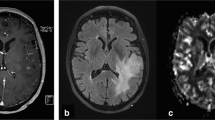
Twenty-seven treatment-naïve children with histopathologically confirmed DIPG H3K27M mutant were prospectively included. MRI performed prior to biopsy included multi-b-value diffusion-weighted imaging, ASL, and dynamic susceptibility contrast (DSC) perfusion imaging. The ADC and cerebral blood flow (CBF) and blood volume (CBV) were measured at the biopsy site. We assessed quantitative histological data, including microvascular density, nuclear density, and H3K27M-positive nuclear density. Gene expression profiling was also assessed in the samples. We compared imaging and histopathological data according to histone subgroup. We correlated MRI quantitative data with histological data and gene expression.
Results
H3.1K27M mutated tumors showed higher ADC values (median 3151 μm2/s vs 1741 μm2/s, p = 0.003), and lower perfusion values (DSC-rCBF median 0.71 vs 1.43, p = 0.002, and DSC-rCBV median 1.00 vs 1.71, p = 0.02) than H3.3K27M ones. They had similar microvascular and nuclear density, but lower H3K27M-positive nuclear density (p = 0.007). The DSC-rCBV was positively correlated to the H3K27M-positive nuclear density (rho = 0.74, p = 0.02). ADC values were not correlated with nuclear density nor perfusion values with microvascular density. The expression of gated channel activity–related genes tended to be inversely correlated with ADC values and positively correlated with DSC perfusion.
Conclusions
H3.1K27M mutated tumors have higher ADC and lower perfusion values than H3.3K27M ones, without direct correlation with microvascular or nuclear density. This may be due to tissular edema possibly related to gated channel activity–related gene expression.
Key Points
• H3.1K27M mutant DIPG had higher apparent diffusion coefficient (p = 0.003), lower α (p = 0.048), and lower relative cerebral blood volume (p = 0.02) than H3.3K27M mutant DIPG at their biopsy sites.
• Biopsy samples obtained within the tumor’s enhancing portion showed higher microvascular density (p = 0.03) than samples obtained outside the tumor’s enhancing portion, but similar H3K27M-positive nuclear density (p = 0.84).
• Relative cerebral blood volume measured at the biopsy site was significantly correlated with H3K27M-positive nuclear density (rho = 0.74, p = 0.02).





Similar content being viewed by others
Abbreviations
- CBF:
-
Cerebral blood flow
- CBV:
-
Cerebral blood volume
- DIPG:
-
Diffuse intrinsic pontine glioma
- DSC:
-
Dynamic susceptibility contrast
- FLAIR:
-
Fluid-attenuated inversion recovery
- WHO:
-
Word Health Organization
References
Puget S, Beccaria K, Blauwblomme T et al (2015) Biopsy in a series of 130 pediatric diffuse intrinsic pontine gliomas. Childs Nerv Syst 31:1773–1780. https://doi.org/10.1007/s00381-015-2832-1
Wu G, Diaz AK, Paugh BS et al (2014) The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat Genet 46:444–450. https://doi.org/10.1038/ng.2938
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Castel D, Philippe C, Calmon R et al (2015) Histone H3F3A and HIST1H3B K27M mutations define two subgroups of diffuse intrinsic pontine gliomas with different prognosis and phenotypes. Acta Neuropathol 130:815–827. https://doi.org/10.1007/s00401-015-1478-0
Lapin DH, Tsoli M, Ziegler DS (2017) Genomic insights into diffuse intrinsic pontine glioma. Front Oncol 7:57. https://doi.org/10.3389/fonc.2017.00057
Castel D, Kergrohen T, Tauziède-Espariat A et al (2020) Histone H3 wild-type DIPG/DMG overexpressing EZHIP extend the spectrum diffuse midline gliomas with PRC2 inhibition beyond H3-K27M mutation. Acta Neuropathol 139:1109–1113. https://doi.org/10.1007/s00401-020-02142-w
Castel D, Grill J, Debily M-A (2016) Histone H3 genotyping refines clinico-radiological diagnostic and prognostic criteria in DIPG. Acta Neuropathol 131:795–796. https://doi.org/10.1007/s00401-016-1568-7
Hoffman LM, Veldhuijzen van Zanten SEM, Colditz N et al (2018) Clinical, radiologic, pathologic, and molecular characteristics of long-term survivors of diffuse intrinsic pontine glioma (DIPG): a collaborative report from the International and European Society for Pediatric Oncology DIPG Registries. J Clin Oncol 36:1963–1972. https://doi.org/10.1200/JCO.2017.75.9308
Taylor KR, Vinci M, Bullock AN, Jones C (2014) ACVR1 mutations in DIPG: lessons learned from FOP. Cancer Res 74:4565–4570. https://doi.org/10.1158/0008-5472.CAN-14-1298
Cohen KJ, Jabado N, Grill J (2017) Diffuse intrinsic pontine gliomas-current management and new biologic insights. Is there a glimmer of hope? Neuro Oncol 19:1025–1034. https://doi.org/10.1093/neuonc/nox021
Piccardo A, Tortora D, Mascelli S et al (2019) Advanced MR imaging and 18F-DOPA PET characteristics of H3K27M-mutant and wild-type pediatric diffuse midline gliomas. Eur J Nucl Med Mol Imaging 46:1685–1694. https://doi.org/10.1007/s00259-019-04333-4
Pan C, Liu J, Tang J et al (2019) A machine learning-based prediction model of H3K27M mutations in brainstem gliomas using conventional MRI and clinical features. Radiother Oncol 130:172–179. https://doi.org/10.1016/j.radonc.2018.07.011
Su X, Chen N, Sun H et al (2020) Automated machine learning based on radiomics features predicts H3 K27M mutation in midline gliomas of the brain. Neuro Oncol 22:393–401. https://doi.org/10.1093/neuonc/noz184
Chen H, Hu W, He H et al (2019) Noninvasive assessment of H3 K27M mutational status in diffuse midline gliomas by using apparent diffusion coefficient measurements. Eur J Radiol 114:152–159. https://doi.org/10.1016/j.ejrad.2019.03.006
Aboian MS, Tong E, Solomon DA et al (2019) Diffusion characteristics of pediatric diffuse midline gliomas with histone H3-K27M mutation using apparent diffusion coefficient histogram analysis. AJNR Am J Neuroradiol 40:1804–1810. https://doi.org/10.3174/ajnr.A6302
Hargrave D, Chuang N, Bouffet E (2008) Conventional MRI cannot predict survival in childhood diffuse intrinsic pontine glioma. J Neurooncol 86:313–319. https://doi.org/10.1007/s11060-007-9473-5
Chen HJ, Panigrahy A, Dhall G et al (2010) Apparent diffusion and fractional anisotropy of diffuse intrinsic brain stem gliomas. AJNR Am J Neuroradiol 31:1879–1885. https://doi.org/10.3174/ajnr.A2179
Hipp SJ, Steffen-Smith E, Hammoud D et al (2011) Predicting outcome of children with diffuse intrinsic pontine gliomas using multiparametric imaging. Neuro Oncol 13:904–909. https://doi.org/10.1093/neuonc/nor076
Poussaint TY, Kocak M, Vajapeyam S et al (2011) MRI as a central component of clinical trials analysis in brainstem glioma: a report from the Pediatric Brain Tumor Consortium (PBTC). Neuro-oncology 13:417–427. https://doi.org/10.1093/neuonc/noq200
Lober RM, Cho Y-J, Tang Y et al (2014) Diffusion-weighted MRI derived apparent diffusion coefficient identifies prognostically distinct subgroups of pediatric diffuse intrinsic pontine glioma. J Neurooncol 117:175–182. https://doi.org/10.1007/s11060-014-1375-8
Conway AE, Reddick WE, Li Y et al (2014) “Occult” post-contrast signal enhancement in pediatric diffuse intrinsic pontine glioma is the MRI marker of angiogenesis? Neuroradiology 56:405–412. https://doi.org/10.1007/s00234-014-1348-9
Jansen MH, Veldhuijzen van Zanten SE, Sanchez Aliaga E et al (2015) Survival prediction model of children with diffuse intrinsic pontine glioma based on clinical and radiological criteria. Neuro-oncology 17:160–166. https://doi.org/10.1093/neuonc/nou104
Poussaint TY, Vajapeyam S, Ricci KI et al (2016) Apparent diffusion coefficient histogram metrics correlate with survival in diffuse intrinsic pontine glioma: a report from the Pediatric Brain Tumor Consortium. Neuro Oncol 18:725–734. https://doi.org/10.1093/neuonc/nov256
Szychot E, Youssef A, Ganeshan B et al (2020) Predicting outcome in childhood diffuse midline gliomas using magnetic resonance imaging based texture analysis. J Neuroradiol. https://doi.org/10.1016/j.neurad.2020.02.005
Vajapeyam S, Brown D, Billups C et al (2020) Advanced ADC histogram, perfusion, and permeability metrics show an association with survival and pseudoprogression in newly diagnosed diffuse intrinsic pontine glioma: a report from the Pediatric Brain Tumor Consortium. AJNR Am J Neuroradiol 41. https://doi.org/10.3174/ajnr.A6499
Jaimes C, Vajapeyam S, Brown D et al (2020) MR imaging correlates for molecular and mutational analyses in children with diffuse intrinsic pontine glioma. AJNR Am J Neuroradiol 41. https://doi.org/10.3174/ajnr.A6546
Harward S, Harrison Farber S, Malinzak M et al (2018) T2-weighted images are superior to other MR image types for the determination of diffuse intrinsic pontine glioma intratumoral heterogeneity. Childs Nerv Syst 34:449–455. https://doi.org/10.1007/s00381-017-3659-8
Harris RJ, Cloughesy TF, Hardy AJ et al (2015) MRI perfusion measurements calculated using advanced deconvolution techniques predict survival in recurrent glioblastoma treated with bevacizumab. J Neurooncol 122:497–505. https://doi.org/10.1007/s11060-015-1755-8
Jenkinson M, Bannister P, Brady M, Smith S (2002) Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage 17:825–841. https://doi.org/10.1016/s1053-8119(02)91132-8
Dangouloff-Ros V, Deroulers C, Foissac F et al (2016) Arterial spin labeling to predict brain tumor grading in children: correlations between histopathologic vascular density and perfusion MR imaging. Radiology 281:553–566. https://doi.org/10.1148/radiol.2016152228
Deroulers C, Dangouloff-Ros V, Badoual M et al (2016) Automatic quantification of the microvascular density on whole slide images, applied to paediatric brain tumours. Diagn Pathol 2. https://doi.org/10.17629/www.diagnosticpathology.eu-2016-2:209
Farnsworth RH, Lackmann M, Achen MG, Stacker SA (2014) Vascular remodeling in cancer. Oncogene 33:3496–3505. https://doi.org/10.1038/onc.2013.304
Camia F, Pisciotta L, Morana G et al (2017) Combined early treatment in hemiplegic attacks related to CACNA1A encephalopathy with brain oedema: blocking the cascade? Cephalalgia 37:1202–1206. https://doi.org/10.1177/0333102416668655
Plessier A, Le Dret L, Varlet P et al (2017) New in vivo avatars of diffuse intrinsic pontine gliomas (DIPG) from stereotactic biopsies performed at diagnosis. Oncotarget 8:52543–52559. https://doi.org/10.18632/oncotarget.15002
Scallan J, Huxley VH, Korthuis RJ (2010) Capillary fluid exchange: regulation, functions, and pathology. In: Colloquium lectures on integrated systems physiology: from molecules to function. Morgan & Claypool Publishers, pp 1–94
Sedlacik J, Winchell A, Kocak M et al (2013) MR imaging assessment of tumor perfusion and 3D segmented volume at baseline, during treatment, and at tumor progression in children with newly diagnosed diffuse intrinsic pontine glioma. AJNR Am J Neuroradiol 34:1450–1455. https://doi.org/10.3174/ajnr.A3421
Calmon R, Puget S, Varlet P et al (2017) Multimodal magnetic resonance imaging of treatment-induced changes to diffuse infiltrating pontine gliomas in children and correlation to patient progression-free survival. Int J Radiat Oncol Biol Phys 99:476–485. https://doi.org/10.1016/j.ijrobp.2017.04.007
Morana G, Tortora D, Staglianò S et al (2018) Pediatric astrocytic tumor grading: comparison between arterial spin labeling and dynamic susceptibility contrast MRI perfusion. Neuroradiology 60:437–446. https://doi.org/10.1007/s00234-018-1992-6
Dangouloff-Ros V, Grevent D, Pagès M et al (2015) Choroid plexus neoplasms: toward a distinction between carcinoma and papilloma using arterial spin-labeling. AJNR Am J Neuroradiol 36:1786–1790. https://doi.org/10.3174/ajnr.A4332
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Nathalie Boddaert.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects (17/27) or cohorts have been previously reported in a molecular analysis study (Castel et al Acta Neuropathol 2015).
Methodology
• prospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calmon, R., Dangouloff-Ros, V., Varlet, P. et al. Radiogenomics of diffuse intrinsic pontine gliomas (DIPGs): correlation of histological and biological characteristics with multimodal MRI features. Eur Radiol 31, 8913–8924 (2021). https://doi.org/10.1007/s00330-021-07991-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07991-x