Abstract
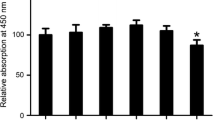
Bone is the most common late metastasis of breast cancer. Bone metastasis causes not only severe bone pain, but also bone-related diseases such as pathological fractures, which are closely related to osteoclasts. The effects of demethoxycurcumin (DMC) on osteoclast biology has not been investigated. In this study, we explored the effects of DMC on MDA-MB-231 cells, MCF-7 cells, and osteoclasts induced by RANKL in vitro, as well as the protective effect on bone destruction of tumor bone metastasis in vivo. DMC showed inhibitory effect on the migration and promotes the apoptosis of MDA-MB-231 and MCF-7 cells. At the same time, DMC inhibited osteoclast maturation and mature osteoclast bone resorption in a dose-dependent manner, and suppressed the expression of osteoclast marker genes TRAP, CTSK, MMP9, V-ATPase-d2 and DC-STAMP significantly. Biochemical data showed that DMC inhibited tumor cells and osteoclasts by inhibiting the early activation of ERK and JNK MAPK pathway. Consistent with the results in vitro, we confirmed that DMC protects bone destruction caused by tumor metastasis in vivo. In short, our study confirmed that DMC could be used as a potential drug for the treatment of tumor bone destruction.







Similar content being viewed by others
References
Torre L et al (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108
Pattarawat P et al (2020) Formulation of a triple combination gemcitabine plus romidepsin + cisplatin regimen to efficaciously and safely control triple-negative breast cancer tumor development. Cancer ChemotherPharmacol 85(1):141–152
Kim S et al (2017) Ipatasertib plus paclitaxel versus placebo plus paclitaxel as first-line therapy for metastatic triple-negative breast cancer (LOTUS): a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol 18(10):1360–1372
Ibrahim M et al (2015) Should de-escalation of bone-targeting agents be standard of care for patients with bone metastases from breast cancer? A systematic review and meta-analysis. Ann OncolOff J EurSoc Med Oncol 26(11):2205–2213
Chen Y, Sosnoski D, Mastro A (2010) Breast cancer metastasis to the bone: mechanisms of bone loss. Breast Cancer Res BCR 12(6):215
Wood S, Westbrook J, Brown J (2014) Omic-profiling in breast cancer metastasis to bone: implications for mechanisms, biomarkers and treatment. Cancer Treat Rev 40(1):139–152
Quayle L, Ottewell P, Holen I (2015) Bone metastasis: molecular mechanisms implicated in tumour cell dormancy in breast and prostate cancer. Curr Cancer Drug Targets 15(6):469–480
Tanaka R et al (2016) Risk factors for developing skeletal-related events in breast cancer patients with bone metastases undergoing treatment with bone-modifying agents. Oncologist 21(4):508–513
Niikura K (2007) Effect of a V-ATPase inhibitor, FR202126, in syngeneic mouse model of experimental bone metastasis. Cancer ChemotherPharmacol 60(4):555–562
Mundy G (2002) Metastasis to bone: causes, consequences and therapeutic opportunities. Nat Rev Cancer 2(8):584–593
Guise T et al (2006) Basic mechanisms responsible for osteolytic and osteoblastic bone metastases. Clin Cancer Res Off J Am Assoc Cancer Res 12:6213s–6216s
Yoneda T, Hiraga T (2005) Crosstalk between cancer cells and bone microenvironment in bone metastasis. Biochem Biophys Res Commun 328(3):679–687
Karsenty G, Olson E (2016) Bone and muscle endocrine functions: unexpected paradigms of inter-organ communication. Cell 164(6):1248–1256
Currey J, Dean M, Shahar R (2017) Revisiting the links between bone remodelling and osteocytes: insights from across phyla. Biol Rev Camb Philos Soc 92(3):1702–1719
Tibullo D et al (2020) Ixazomib improves bone remodeling and counteracts sonic hedgehog signaling inhibition mediated by myeloma cells. Cancers 12(2):323
Ell B et al (2013) Tumor-induced osteoclast miRNA changes as regulators and biomarkers of osteolytic bone metastasis. Cancer Cell 24(4):542–556
Bennett C et al (2018) Senataxin mutations elicit motor neuron degeneration phenotypes and yield TDP-43 mislocalization in ALS4 mice and human patients. ActaNeuropathol 136(3):425–443
Min Y et al (2010) Tie2 signaling regulates osteoclastogenesis and osteolytic bone invasion of breast cancer. Can Res 70(7):2819–2828
Kim B, Koh J (2019) Coupling factors involved in preserving bone balance. Cell Mol Life Sci CMLS 76(7):1243–1253
Yuan F et al (2018) Osteoclast-derived extracellular vesicles: novel regulators of osteoclastogenesis and osteoclast-osteoblasts communication in bone remodeling. Front Physiol 9:628
Cao X (2011) Targeting osteoclast-osteoblast communication. Nat Med 17(11):1344–1346
Teitelbaum S (2000) Bone resorption by osteoclasts. Science (New York, NY) 289(5484):1504–1508
Jacome-Galarza C et al (2019) Developmental origin, functional maintenance and genetic rescue of osteoclasts. Nature 568(7753):541–545
Yahara Y et al (2020) Erythromyeloid progenitors give rise to a population of osteoclasts that contribute to bone homeostasis and repair. Nat Cell Biol 22(1):49–59
Mensah K, Ritchlin C, Schwarz E (2010) RANKL induces heterogeneous DC-STAMP(lo) and DC-STAMP(hi) osteoclast precursors of which the DC-STAMP(lo) precursors are the master fusogens. J Cell Physiol 223(1):76–83
Boyce B (2013) Advances in the regulation of osteoclasts and osteoclast functions. J Dent Res 92(10):860–867
Ikebuchi Y et al (2018) Coupling of bone resorption and formation by RANKL reverse signalling. Nature 561(7722):195–200
Jules J et al (2015) The IVVY motif and tumor necrosis factor receptor-associated factor (TRAF) sites in the cytoplasmic domain of the receptor activator of nuclear factor κB (RANK) cooperate to induce osteoclastogenesis. J BiolChem 290(39):23738–23750
Boyle W, Simonet W, Lacey D (2003) Osteoclast differentiation and activation. Nature 423(6937):337–342
Li X et al (2002) p38 MAPK-mediated signals are required for inducing osteoclast differentiation but not for osteoclast function. Endocrinology 143(8):3105–3113
Hatamipour M et al (2018) Demethoxycurcumin: a naturally occurring curcumin analogue with antitumor properties. J Cell Physiol 233(12):9247–9260
Hatamipour M et al (2019) Demethoxycurcumin: a naturally occurring curcumin analogue for treating non-cancerous diseases. J Cell Physiol 234(11):19320–19330
Arshad L et al (2017) An overview of structure–activity relationship studies of curcumin analogs as antioxidant and anti-inflammatory agents. Fut Med Chem 9(6):605–626
Ramkumar M et al (2018) Demethoxycurcumin, a natural derivative of curcumin abrogates rotenone-induced dopamine depletion and motor deficits by its antioxidative and anti-inflammatory properties in Parkinsonian Rats. Pharmacog Mag 14(53):9–16
Dos Santos P et al (2019) The nanoencapsulation of curcuminoids extracted from Curcuma longa L. and an evaluation of their cytotoxic, enzymatic, antioxidant and anti-inflammatory activities. Food Funct 10(2):573–582
Srirod S, Tewtrakul S (2019) Anti-inflammatory and wound healing effects of cream containing Curcuma mangga extract. J Ethnopharmacol 238:111828
Ahmed T, Gilani A (2014) Therapeutic potential of turmeric in Alzheimer’s disease: curcumin or curcuminoids? Phytother Res PTR 28(4):517–525
Du Z, Sha X (2017) Demethoxycurcumin inhibited human epithelia ovarian cancer cells’ growth via up-regulating miR-551a. TumourBiol J Intern SocOncodevelopBiol Med 39(3):1010428317694302
Lin C et al (2018) viaDemethoxycurcumin suppresses migration and invasion of human cervical cancer hela cells inhibition of NF-κB pathways. Anticancer Res 38(5):2761–2769
Anbarasu K, Jayanthi S (2018) Identification of curcumin derivatives as human LMTK3 inhibitors for breast cancer: a docking, dynamics, and MM/PBSA approach. 3 Biotech 8(5):228
Sterling J et al (2011) Advances in the biology of bone metastasis: how the skeleton affects tumor behavior. Bone 48(1):6–15
Fecher L, Amaravadi R, Flaherty K (2008) The MAPK pathway in melanoma. CurrOpinOncol 20(2):183–189
Wang L et al (2019) Curcumin derivative WZ35 inhibits tumor cell growth via ROS-YAP-JNK signaling pathway in breast cancer. J ExpClin Cancer Res CR 38(1):460
Yao Y et al (2012) HGFK1 inhibits bone metastasis in breast cancer through the TAK1/p38 MAPK signaling pathway. Cancer Gene Ther 19(9):601–608
Guise T (2000) Molecular mechanisms of osteolytic bone metastases. Cancer 88:2892–2898
Roodman G, Dougall W (2008) RANK ligand as a therapeutic target for bone metastases and multiple myeloma. Cancer Treat Rev 34(1):92–101
Nakashima T et al (2011) Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med 17(10):1231–1234
Hayder M et al (2011) A phosphorus-based dendrimer targets inflammation and osteoclastogenesis in experimental arthritis. SciTransl Med 3(81):81ra35
Wuerzberger-Davis S et al (2011) Nuclear export of the NF-κB inhibitor IκBα is required for proper B cell and secondary lymphoid tissue formation. Immunity 34(2):188–200
Li C et al (2011) Maslinic acid suppresses osteoclastogenesis and prevents ovariectomy-induced bone loss by regulating RANKL-mediated NF-κB and MAPK signaling pathways. J Bone Mineral Res Off J Am Soc Bone Mineral Res 26(3):644–656
Huang S et al (2017) Tunicamycin potentiates paclitaxel-induced apoptosis through inhibition of PI3K/AKT and MAPK pathways in breast cancer. CancerChemotherPharmacol 80(4):685–696
Acknowledgements
This project is supported by grants from Science and Technology Project of Suzhou Science and Technology Bureau (sys2018091, SS2019070), and Key Project of Jiangsu Science and Technology Development Program of Traditional Chinese Medicine (ZD201910).
Author information
Authors and Affiliations
Contributions
Conceptualization: XS, XS and QM. Data curation: XS and XS. Formal analysis: XS, HC, GL and JW. Funding acquisition: QM and YL. Investigation: HC and PY. Methodology: BL, CZ and JW. Project administration: BL and YL. Resources: YQ, QM and YL. Software: YQ and CZ. Supervision: QM, YL and LS. Validation: QM and YL. Visualization: GL and PY. Writing—original draft: XS and XS. Writing—review and editing: XS, XS, QM and YL.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaofeng Shen and Xiaochen Sun are co-first authors.
Rights and permissions
About this article
Cite this article
Shen, X., Sun, X., Chen, H. et al. Demethoxycucumin protects MDA-MB-231 cells induced bone destruction through JNK and ERK pathways inhibition. Cancer Chemother Pharmacol 87, 487–499 (2021). https://doi.org/10.1007/s00280-020-04198-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-020-04198-7