Abstract
Background
qSOFA has been proposed as a prognostic tool in patients with sepsis. This study set out to assess the sensitivity of several scores, namely: the pre-ICU qSOFA, the qSOFA with lactate (qSOFA L), SIRS score, qSOFA + SIRS score (qSIRS) and qSIRS with lactate (qSIRS L) in predicting in-hospital mortality in patients with surgical sepsis as well as the sensitivity of these scores in predicting high-grade sepsis. The secondary aim was to determine which of these scores is best suited to predict high-grade surgical sepsis.
Methods
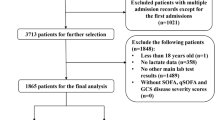
This was a retrospective cohort study that was conducted between December 2012 and August 2017 in a public metropolitan surgical service. Data from patients aged > 13 years, who were admitted to the hospital and who had an emergency surgical procedure for source control were retrieved from a prospectively maintained hybrid electronic database. The qSOFA, qSOFA plus lactate (qSOFA L), SIRS and qSOFA + SIRS (qSIRS), as well as the qSIRS plus lactate (qSIRS L), were calculated for each patient. A lactate level that was greater than 2mmol/L was deemed to be a positive finding. Any score ≥2 was deemed to be a positive score. The outcome measure was in-hospital mortality. The prognostic value of qSOFA, qSOFA L, SIRS, qSIRS and qSIRS L was studied. Receiver operating characteristic analyses were performed to determine the area under the curve (AUC), sensitivity, specificity and positive and negative likelihood ratios for positive qSOFA, qSOFA L, SIRS, qSIRS, and qSIRS L. Contingency tables were used to calculate the sensitivity, specificity, PPV and NPV for predicting severe or high-grade surgical sepsis.
Results
There were a total number of 1884 patients in the sample group of whom 855 were female (45.4%). The median patient age was 36 years (IQR 23–56). A total of 1489 patients (79%) were deemed to have high-grade sepsis based on an advanced EGS AAST grading, whilst 395 patients (21%) had low-grade sepsis. A total of 71 patients died (3.8%). Of these patients who died, 67 (94.4%) had high-grade sepsis and 4 (5.6%) had low-grade sepsis. The mortality rate in the high-grade sepsis group was 4.5%, whilst the mortality rate in the low-grade sepsis group was 1%. The scores with the greatest accuracy in predicting mortality were qSIRS (AUROC 0.731, 95% CI 0.68–0.78), followed by SIRS (AUROC 0.70, 95% CI 0.65–0.75). The qSOFA and qSOFA L were the least accurate in predicting mortality (AUROC 0.684, 95% CI 0.63–0.74 for both). The addition of lactate had no significant effect on the accuracy of the five scores in predicting mortality. Patients with a qSOFA ≥ 2 have an increased risk of dying (OR 5.8), as do patients with a SIRS score ≥2 (OR 2.7). qSIRS L had the highest sensitivity (69%) in predicting the presence of high-grade surgical sepsis, followed by qSIRS (65.5% sensitivity). qSOFA showed a very low sensitivity of only 4.5% and a high specificity of 99.2%. The addition of lactate to the score marginally improved the sensitivity. Lactate of 2mmol/L or more was also an independent predictor of high-grade sepsis.
Conclusion
The qSIRS score is most accurate in predicting mortality in surgical sepsis. The qSOFA score is inferior to both the SIRS and the qSIRS scores in predicting mortality. The qSIRS score with the addition of lactate to the qSIRS score made it the most sensitive score in predicting high-grade surgical sepsis.

Similar content being viewed by others
Abbreviations
- AAST:
-
American Association for the Surgery of Trauma
- AUC:
-
Area under the curve
- AUROC:
-
Area under the receiver operating characteristic curve
- CI:
-
Confidence interval
- ED:
-
Emergency Department
- EGS:
-
Emergency general surgery
- HIC:
-
High-income country
- HEMR:
-
Hybrid Electronic Medical Registry
- HGS:
-
High-grade sepsis
- ICU:
-
Intensive care unit
- KZN:
-
KwaZulu-Natal
- LGS:
-
Low-grade sepsis
- LMIC(s):
-
Low-and-middle-income country (countries)
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- qSOFA:
-
quick Sequential Organ Failure Assessment
- qSOFAL:
-
quick Sequential Organ Failure Assessment plus lactate
- qSIRS:
-
quick Sequential Organ Failure Assessment + systemic inflammatory response syndrome
- qSIRSL:
-
quick Sequential Organ Failure Assessment + systemic inflammatory response syndrome + lactate
- ROC:
-
Receiver operating characteristic curve
- SIRS:
-
Systemic inflammatory response syndrome
- SOFA:
-
Sequential Organ Failure Assessment
- WCC:
-
White cell count
References
Moore L, Moore F (2012) Epidemiology of Sepsis in Surgical Patients. Surg Clin N Am 92:1425–1443. https://doi.org/10.1016/j.suc.2012.08.009
Singer M, Deutschman CS, Seymour CW et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315:801–810
Sartelli M, Kluger Y, Ansaloni L et al (2018) Raising concerns about Sepsis-3 definitions. World J Emerg Surg 13:6. https://doi.org/10.1186/s13017-018-0165-6
Moore LJ, Moore FA (2011) Early diagnosis and evidence-based care of surgical sepsis. J Intensive Care Med 28(2):107–117
Cohen J, Vincent JL, Adhikari NKJ et al (2015) Sepsis: a roadmap for future research. Lancet Infect Dis 15:581–614
Otu A, Elston J, Nsutebu E (2015) Sepsis in Africa: practical steps to stem the tide. Pan Afr Med J 21:323. https://doi.org/10.11604/pamj.2015.21.323.6462
Vincent JL, Marshall JC, Namendys-Silva SA et al (2014) Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med 2:380–386
Riviello E, Sugira V, Twagvirumugabe T (2015) Sepsis research and the poorest of the poor. Lancet Infect Dis 15(5):501–503. https://doi.org/10.1016/S1473-3099(15)70148-9Epub 2015 Apr 19
Becker JU, Theodosis C, Jacob ST et al (2009) Surviving sepsis in low-income and middle-income countries: new directions for care and research. Lancet Infect Dis 9(9):577–582. https://doi.org/10.1016/S1473-3099(09)70135-5
Tupchong K, Koyfman A, Foran M (2015) Sepsis, severe sepsis and septic shock: a review of the literature. Afr J Emerg Med 5:127–135. https://doi.org/10.1016/j/afjem.2014.05.004
Baeleni I, Jochberger S, Laimer T et al (2011) Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Critical Care 15: R10. http://ccforum.com/content/15/1/R10
Riviello ED (2014) Improving outcomes for severe sepsis in Africa: one step closer. Crit Care Med 42(11):2439–2440. https://doi.org/10.1097/CCM.0000000000000591
Buys D, Kim H, Smalley M et al (2017) Characteristics of poverty in upper middle income countries http://www.lafollette.wisc.edu/outreach-public-service/workshops-in-public-affairspublications@lafollette.wisc.edu. Accessed Dec 2018
Green SL, Kong VY, Clarke DL et al (2017) The spectrum and outcome of surgical sepsis in Pietermaritzburg, South Africa. S Afr Med J 107(2):134–136. https://doi.org/10.7196/SAMJ.2017.v107i2.11339
Green S, Kong VY, Odendaal J et al (2017) The effect of HIV status on clinical outcomes of surgical sepsis in KwaZulu-Natal Province. S Afr Med J 107(8):702–705. https://doi.org/10.7196/SAMJ.2017.v107i8.12045
Green S, Kong VY, Laing GL et al (2017) The effect of stage of HIV disease as determined by CD4 count on clinical outcomes of surgical sepsis in South Africa. Ann R Coll Surg Engl 99(6):459–463. https://doi.org/10.1308/rcsann.2017.0057
Dare AJ, Onajin-Obembe B (2018) A snapshot of surgical outcomes and needs in Africa. Lancet 391:1553–1554
Olugunde R, Maruthappu M, Shanmugarajah K, Shalhoub J (2014) Surgical care in low- and middle-income countries: Burden and barriers. Int J Surg 12:858–863. https://doi.org/10.1016/j.ijsu.2014.07.0091
Bhagwanjee S, Scribante J (2007) National audit of critical care resources in South Africa – unit and bed distribution. SAMJ 97(12):1311–1314
Kaukonen KM, Bailey M, Pilcher D et al (2015) Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med 372:1629–1638. https://doi.org/10.1056/NEJMoa1415236
Adhikari NKJ, Rubenfeld GD (2018) qSOFA for Patients with Sepsis in Low-and-Middle Income countries. JAMA 319(21):2175–2176. https://doi.org/10.1001/jama.2018.6413
Statistics South Africa (2017) Mid-year population estimates 2017 https://www.statssa.gov.za/publications/P0302/P03022017.pdf. Accessed 29 Oct 2018
Laing GL, Bruce JL, Aldous C et al (2013) The design, construction and implementation of a computerized trauma registry in a developing South African metropolitan trauma service. Injury 45:3–8
Laing GL, Bruce JL, Skinner DL et al (2014) Development, implementation, and evaluation of a hybrid electronic medical record system specifically designed for a developing world surgical service. World J Surg 38:1388–1397. https://doi.org/10.1007/s00268-013-2438-2
Laing G, Bruce J, Skinner D et al (2015) Using a hybrid electronic medical record system for the surveillance of adverse surgical events and human error in a developing world surgical service. World J Surg 39:70–79. https://doi.org/10.1007/s00268-014-2766-x
Bone RC, Balk RA, Cerra FB et al (1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
American Association For The Surgery Of Trauma (AAST) Emergency General Surgery Anatomic Grading Scales: Data Dictionaries for AAST Grading System for EGS Conditions http://www.aast.org/emergency-general-surgery-anatomic-grading-scales
Tominaga GT, Staugenmayer KL, Shafi S et al (2016) The American Association for the Surgery of Trauma grading scale for 16 emergency general surgical conditions: Disease-specific criteria characterizing anatomic severity grading. J Trauma Acute Care Surg 81(3):593–601. https://doi.org/10.1097/TA.0000000000001127
Williams JM, Greenslade JH, McKenzie JV et al (2017) SIRS, qSOFA and organ dysfunction: insights from a prospective database of emergency department patients with infection. Chest 151:586–596
Giamarellos-Bourboulis EJ, Tsaganos T, Tsangaris I et al (2017) Validation of the new Sepsis-3 definitions: proposal for improvement in early risk identification. Clin Microbiol Infect 23:104–109
Churpek MM, Zadravecz FJ, Winslow C et al (2015) Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med 192:958–964
Fernando SM, Tran A, Taljaard M, et al (2018) Prognostic accuracy of the quick sequential organ failure assessment for mortality in patients with suspected infection: a systematic review and meta-analysis. Ann Intern Med
Jiang J, Yang J, Mei J, Jin Y, Lu Y (2018) Head-to-head comparison of qSOFA and SIRS criteria in predicting the mortality of infected patients in the emergency department: a meta-analysis. Scand J Trauma Resusc Emerg Med 26(1):56. https://doi.org/10.1186/s13049-018-0527-9
Ronson SLL, Leung LY, Brabrand M et al (2019) qSOFA is a poor predictor of short-term mortality in all patients: a systemic review of 410,000 patients. J Clin Med 8:61
Song JU, Sin CK, Park HK, Shim SR, Lee (2018) Performance of the quick Sequential (sepsis-related) Organ Failure Assessment score as a prognostic tool in infected patients outside the intensive care unit: a systematic review and meta-analysis. J Crit Care 22(1):28. https://doi.org/10.1186/s13054-018-1952-x
Maitra S, Som A, Bhattacharjee S (2018) Accuracy of quick Sequential Organ Failure Assessment (qSOFA) score and systemic inflammatory response syndrome (SIRS) criteria for predicting mortality in hospitalized patients with suspected infection: a meta-analysis of observational studies. Clin Microbiol Infect. https://doi.org/10.1016/j.cmi.2018.03.032
Ramar K, Gajic O (2013) Early recognition and treatment of severe sepsis. Am J Respir Crit Care Med 188:7–8
Ghanem-Zoubi NO, Vadi M, Laor A et al (2011) Assessment of disease-severity scoring systems for patients with sepsis in general medicine departments. Crit Care 15:R95
Otto MA (2016) Combine qSOFA and SIRS for best sepsis score. Chest https://www.mdedge.com/chestphysician/article/117835/infectious-diseases/combine-qsofa-and-sirs-best-sepsis-score. Accessed Feb 2019
Aluisio AR, Garbern S, Wiskel T et al (2018) Mortality outcomes based on ED qSOFA score and HIV status in a developing low income country. Am J Emerg Med 36(11):2010–2019. https://doi.org/10.1016/j.ajem.2018.03.014
Rudd KE, Seymour CW, Aluisio AR et al (2018) Association of the quick sequential (sepsis-related) organ failure assessment (qSOFA) Score with excess hospital mortality in adults with suspected infection in low- and middle-income countries. JAMA 319(21):2202–2211. https://doi.org/10.1001/jama.2018.6229
Rose J, Weiser TG, Hider P et al (2015) Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health 3(52):S13–S20
Knowlton LM, Banguti P, Chackungal S et al (2017) A geospatial evaluation of timely access to surgical care in seven countries. Bull World Health Organ 95:437–444. https://doi.org/10.2471/BLT.16.175885
Acknowledgements
None.
Funding
The authors received no funds for this study.
Author information
Authors and Affiliations
Contributions
SLG assumes overall responsibility for study concept, manuscript content and compilation. DLC contributed towards study design and towards manuscript content. MTDS is responsible for statistical analyses of data. CC contributed towards data review and analysis. MTDS, JB and WB are responsible for database maintenance. GL is responsible for design of the database. VK is responsible for supervision of the research. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval to maintain this database and to conduct this study has been granted by the Biomedical Research Ethics Committee (BREC) of the University of KwaZulu-Natal (BE221/13; BE 207/09; BE660/18 substudy of BCA221/13).
Consent for publication
Obtained through the University of KwaZulu-Natal Biomedical Research Ethics Committee (BE221/13; BE 207/09; BE660/18 substudy of BCA221/13).
Availability of data and material
All data and material are available on request from the corresponding author.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Green, S.L., Smith, M.T.D., Cairns, C. et al. The Combined SIRS + qSOFA (qSIRS) Score is More Accurate Than qSOFA Alone in Predicting Mortality in Patients with Surgical Sepsis in an LMIC Emergency Department. World J Surg 44, 21–29 (2020). https://doi.org/10.1007/s00268-019-05181-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05181-x