Abstract
Introduction
The quantification and analysis of adverse events is essential to benchmark surgical outcomes and establish a foundation for quality improvement interventions. We developed a hybrid electronic medical record (HEMR) system for the accurate collection and integration of data into a structured morbidity and mortality (M&M) meeting.
Methodology
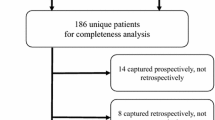
The HEMR system was implemented on January 1, 2013. It included a mechanism to capture and classify adverse events using the ICD-10 coding system. This was achieved by both prospective reporting by clients and by retrospective sentinel-event-trawling performed by administrators.
Results
From January 1, 2013 to March 20, 2014, 6,217 patients were admitted within the tertiary surgical service of Greys Hospital. A total of 1,314 (21.1 %) adverse events and 315 (5.1 %) deaths were recorded. The adverse events were divided into 875 “pathology-related” morbidities and 439 “error-related” morbidities. Pathology-related morbidities included 725 systemic complications and 150 operative complications. Error-related morbidities included 257 cognitive errors, 158 (2.5 %) iatrogenic injuries, and 24 (1.3 %) missed injuries. Error accounted for 439 (33 %) of the total number of adverse events. A total of 938 (71.4 %) adverse events were captured prospectively, whereas the remaining 376 (28.6 %) were captured retrospectively. The ICD-10 coding system was found to have some limitations in its classification of adverse events.
Conclusions
The HEMR system has provided the necessary platform within our service to benchmark the incidence of adverse events. The use of the international ICD-10 coding system has identified some limitations in its ability to classify and categorise adverse events in surgery.



Similar content being viewed by others
References
Kohn LT, Corrigan JM, Donaldson MS (eds) (2000) To err is human Building a safer health system. National Academy Press, Washington, DC
Reason J (1995) Understanding adverse events: human factors. Qual Health Care 4:80–89
Reason J (2000) Human error: models and management. BMJ 320:768–770
Chang A, Schyve PM, Croteau RJ, O’Leary DS, Loeb JM (2005) The JCAHO patient safety event taxonomy: a standardized terminology and classification schema for near misses and adverse events. Int J Qual Health Care 17(2):95–105
Bilimoria KY, Kmiecik TE, DaRosa DA, Halverson A, Eskandari MK, Bell RH Jr, Soper NJ, Wayne JD (2009) Development of an online morbidity, mortality, and near-miss reporting system to identify patterns of adverse events in surgical patients. Arch Surg 144(4):305–311
Laing GL, Bruce JL, Skinner DL, Allorto NL, Clarke DL, Aldous C (2013) Development, implementation and evaluation of a hybrid electronic medical record system specifically designed for a developing world surgical service. World J Surg Dec 31. [Epub ahead of print] PMID: 24378554 [PubMed - as supplied by publisher]
Leape LL (1994) Error in medicine. JAMA 272(23):1851–1857
Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV (2006) Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg 244(3):371–380
Clarke DL, Gouveia J, Thomson SR et al (2008) Applying modern error theory to the problem of missed injuries in trauma. World J Surg 32(6):1176–1182. doi:10.1007/s00268-008-9543-7
Clarke DL, Furlong H, Laing GL, Aldous C, Thomson SR (2013) Using a structured morbidity and mortality meeting to understand the contribution of human error to adverse surgical events in a South African regional hospital. S Afr J Surg 51(4):122–126. doi:10.7196/sajs.1537
Pierluissi E, Fischer MA, Campbell AR, Landefeld CS (2003) Discussion of medical errors in morbidity and mortality conferences. JAMA 290(21):2838–2842
Mainz J (2003) Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care 15(6):523–530
Mainz J (2004) Quality indicators: essential for quality improvement. Int J Qual Health Care 16:1–2
Mayer EK, Chow A, Vale JA et al (2009) Appraising the quality of care in surgery. World J Surg 33(8):1584–1593. doi:10.1007/s00268-009-0065-8
Laing GL, Skinner DL, Bruce JL, Aldous C, Oosthuizen GV, Clarke DL (2014) Understanding the burden and outcome of trauma care drives a new trauma systems model. World J Surg 38:1699–1706. doi:10.1007/s00268-014-2448-8 Jan 22. [Epub ahead of print]
MediBank incorporates TraumaBank. A letter from the desk of the president of the Trauma Society of South Africa (Professor Ken Boffard). www.medibank.co.za/letterkentssa.pdf
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Laing, G., Bruce, J., Skinner, D. et al. Using a Hybrid Electronic Medical Record System for the Surveillance of Adverse Surgical Events and Human Error in A Developing World Surgical Service. World J Surg 39, 70–79 (2015). https://doi.org/10.1007/s00268-014-2766-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2766-x






