Abstract
Background
The usefulness of the quick Sequential (Sepsis-related) Organ Failure Assessment (qSOFA) score in providing bedside criteria for early prediction of poor outcomes in patients with suspected infection remains controversial. We investigated the prognostic performance of a positive qSOFA score outside the intensive care unit (ICU) compared with positive systemic inflammatory response syndrome (SIRS) criteria.
Methods
A systematic literature search was performed using MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials. Data were pooled on the basis of sensitivity, specificity, and diagnostic OR. Overall test performance was summarized using a hierarchical summary ROC and the AUC. Meta-regression analysis was used to identify potential sources of bias.
Results
We identified 23 studies with a total of 146,551 patients. When predicting in-hospital mortality in our meta-analysis, we identified pooled sensitivities of 0.51 for a positive qSOFA score and 0.86 for positive SIRS criteria, as well as pooled specificities of 0.83 for a positive qSOFA score and 0.29 for positive SIRS criteria. Discrimination for in-hospital mortality had similar AUCs between the two tools (0.74 vs. 0.71; P = 0.816). Using meta-regression analysis, an overall mortality rate ≥ 10% and timing of qSOFA score measurement could be significant sources of heterogeneity. For predicting acute organ dysfunction, although the AUC for a positive qSOFA score was higher than that for positive SIRS criteria (0.87 vs. 0.76; P < 0.001), the pooled sensitivity of positive qSOFA score was very low (0.47). In addition, a positive qSOFA score tended to be inferior to positive SIRS criteria in predicting ICU admission (0.63 vs. 0.78; P = 0.121).
Conclusions
A positive qSOFA score had high specificity outside the ICU in early detection of in-hospital mortality, acute organ dysfunction, and ICU admission, but low sensitivity may have limitations as a predictive tool for adverse outcomes. Because between-study heterogeneity was highly represented among the studies, our results should be interpreted with caution.
Similar content being viewed by others
Background
Sepsis is defined as life-threatening organ dysfunction that is caused by a dysregulated host response to infection [1]. It is a common cause of admission to the intensive care unit (ICU) and can lead to multiple organ dysfunction syndrome and death [2]. It is essential to differentiate sepsis from an uncomplicated infection because sepsis is associated with poorer outcomes [3]. Early recognition of sepsis can improve outcomes of these patients through corresponding interventions, which include adequately administering fluids and appropriate antibiotics [3]. However, because sepsis is a complex, heterogeneous disease, it is often difficult for clinicians to promptly identify patients with sepsis.
There are no gold standard tests or diagnostic criteria to detect patients with sepsis. For more than two decades, the systemic inflammatory response syndrome (SIRS) criteria have been used in the diagnosis of sepsis [4, 5]. Researchers in several studies have reported controversies regarding the applicability of SIRS, and the SIRS criteria have also been criticized as a sepsis screening tool because of inadequate specificity and sensitivity [4, 5]. In 2016, the Society of Critical Care Medicine (SCCM)/European Society of Intensive Care Med (ESICM) task force released the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) as a new definition for sepsis [1]. The consensus definition replaced the SIRS criteria with the Sequential (Sepsis-related) Organ Failure Assessment (SOFA) score [1]. In addition, the quick SOFA (qSOFA) score was introduced as a bedside criterion to facilitate the identification of patients with suspected infection who are likely to have poor outcomes [1]. Data published shortly after the establishment of Sepsis-3 demonstrated that the predictive validity of qSOFA for in-hospital mortality was statistically greater than either the original SOFA or SIRS criteria in encounters with suspected infection outside the ICU [6]. Researchers in several studies have examined the predictive performance of the qSOFA score for in-hospital mortality in these patients. These studies have generated conflicting evidence, and it is currently unclear whether the qSOFA score has prognostic value for unfavorable outcomes in patients with a suspected infection.
There have been no published meta-analyses of the predictive performance of the qSOFA score. The aim of the present study was to evaluate the prognostic value of a positive qSOFA score compared with positive SIRS criteria for early identification of in-hospital mortality in patients with suspected infection outside the ICU. We also compared the discriminatory capacity between positive qSOFA score and positive SIRS criteria in predicting acute organ dysfunction and ICU admission.
Methods
Data sources and search strategy
This meta-analysis is reported in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses statement [7]. The study protocol was registered with the PROSPERO International Prospective Register of Systematic Reviews (http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017074766). To identify potentially relevant articles, we conducted a comprehensive search of three electronic databases (MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials) up to July 1, 2017. We also performed a manual search of the references listed in relevant review articles. The detailed study protocol and search strategies are provided in Additional file 1. Because this study was a systematic review of published articles, neither informed consent nor ethics approval was required.
Inclusion criteria
We included a study in our analysis if it met the following criteria:
-
1.
The study targeted patients with suspected or confirmed infection outside the ICU.
-
2.
The study evaluated the qSOFA score as a predictive tool for predicting in-hospital mortality, acute organ dysfunction, or ICU admission.
-
3.
The study provided sufficient data to calculate absolute numbers of true-positive, false-positive, false-negative, and true-negative results.
Studies published as full-length articles or letters in peer-reviewed English-language journals were eligible.
Data extraction, definitions, and outcomes
JUS and JL independently extracted potentially relevant studies and reviewed each study according to the predefined criteria for eligibility. We extracted data from the selected studies. Any disagreement in the process of study selection or data extraction was resolved by discussion. A predefined form was used to extract data from each study. Extracted information included details of patient demographics, the study design, and objectives.
The qSOFA score consists of three clinical variables: altered mentation, systolic blood pressure < 100 mmHg, and respiratory rate > 22 breaths/minute [1]. The score ranges from 0 to 3, and a positive qSOFA score is defined as 2 or more points [1]. The SIRS criteria were defined as a respiratory rate > 20 breaths/minute or partial pressure of carbon dioxide < 32 mmHg, a body temperature > 38 °C or < 36 °C, a heart rate > 90 beats/minute, and a white blood cell count > 12,000/mm3 or < 4000/mm3, or > 10% bands [8]. A positive SIRS criterion was also defined as ≥ 2 points [8]. Acute organ dysfunction was defined as an acute 2-point increase in the SOFA score following the proposed Sepsis-3 definitions [1]. In case of studies using the Sepsis-2 definitions, the development of severe sepsis (two or more SIRS signs plus one additional sign of organ failure) was considered as acute organ dysfunction [8, 9]. Outside the ICU included out-of-hospital, emergency department (ED), or general hospital ward settings.
The primary outcome was in-hospital mortality. For trials in which researchers did not investigate in-hospital mortality, we used the 28- or, 30-day mortality instead [10]. In addition, we extracted the data for SIRS from the published materials for qSOFA, and a positive qSOFA score was used to assess the prognostic performance by comparing it with positive SIRS criteria. The secondary outcome was acute organ dysfunction and ICU admission.
Quality assessment
As recommended by the Cochrane Collaboration, we used the Quality Assessment of Diagnostic Accuracy Studies (QUADAS)-2 tool to assess the risk of bias in diagnostic test accuracy [11]. A detailed quality assessment is provided in Additional file 1.
Data synthesis and statistical analysis
The data were presented as mean values for continuous variables and as frequencies (percent) for categorical variables. For diagnostic meta-analysis, we extracted the number of patients with a true-positive, false-positive, false-negative, and true-negative test result either directly or through a recalculation that was based on the reported measures of accuracy in combination with the prevalence and sample size in the included study. We calculated the pooled sensitivity and specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), diagnostic OR (DOR), and AUC as point estimates with 95% CI [12]. We also constructed hierarchical summary ROC (HSROC) curves to overcome some limitations of the traditional summary ROC curve procedure [13], which was closely related to a bivariate random effects meta-analysis [13]. Between-study statistical heterogeneity was assessed using theI2 statistic and Cochran’s Q test [14]. Heterogeneity was assessed using I2 statistics on a scale of 0–100%. If I2 was > 50%, a random-effects model was used; otherwise, a fixed-effects model was used [14]. An I2 > 50% indicated a substantial level of between-study heterogeneity. In cases of substantial heterogeneity, analysis via meta-regression was performed to identify potential sources of bias [15]. If potential sources were found, additional meta-regression was conducted using a generalization of Moses-Littenberg linear models. The model was weighted by the inverse of the variance or study size [16]. Publication bias was evaluated using the Deek test for funnel plot asymmetry [17]. A P value < 0.05 was considered statistically significant. All analyses were performed using Meta-DiSc software (version 1.4; http://www.hrc.es/investigacion/metadisc_en.htm) and Stata statistical software (version 14.2; StataCorp LP, College Station, TX, USA).
Results
Study search
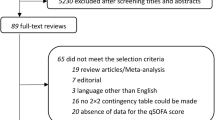
The flowchart in Fig. 1 shows the literature search process. A total of 11,360 published articles were initially identified (3709 articles from MEDLINE, 6758 articles from Embase, and 893 articles from the Cochrane Library). After removing duplicate articles, we screened 8493 potentially eligible articles. Of these articles, 8430 were excluded on the basis of title and abstract. A total of 63 articles underwent full-text review. Forty-one articles were excluded for the reasons presented in Fig. 1. Finally, a total of 23 articles met our inclusion criteria [6, 18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. All studies were published between 2016 and 2017. Features of the included studies are shown in Table 1. The number of patients in each trial ranged from 151 to 66,522, and the overall mortality rate in each study ranged from 2.8% to 33.0%. Researchers in 20 studies reported the discriminatory capacity of the qSOFA score for predicting mortality [6, 18,19,20,21,22, 24,25,26,27,28,29,30,31,32, 34, 36,37,38,39]. In 11 studies, investigators compared the accuracy of positive qSOFA score and positive SIRS criteria for predicting mortality [6, 18, 19, 21, 22, 24,25,26, 28, 37, 39]. The QUADAS assessment is summarized in Additional file 2. Overall, the quality of the studies was deemed satisfactory. However, the QUADAS tool showed that unclear blinding during interpretation of results and lack of reporting for uninterpretable results may be potential sources of bias. Withdrawals from some studies were not clearly explained, which could also have resulted in bias. The funnel plots and regression tests indicated no significant publication bias (see Additional file 3).
Diagnostic accuracy for in-hospital mortality using positive qSOFA scores and SIRS criteria
In the pooled estimates, patients with positive qSOFA scores and SIRS criteria were associated with in-hospital mortality of 12.9% (3847 of 29,709 patients) and 5.8% (3906 of 67,225 patients), respectively. Using the combined data from the included studies, in Fig. 2 we show the pooled sensitivity and specificity of positive qSOFA scores for in-hospital mortality. The pooled sensitivity and specificity for positive qSOFA scores were 0.51 (95% CI, 0.39–0.62) and 0.83 (95% CI, 0.74–0.89), respectively. The PLR, NLR, and pooled DOR were 3.00 (95% CI, 2.39–3.77), 0.60 (95% CI, 0.50–0.70), and 5.04 (95% CI, 4.09–6.23), respectively. The pooled sensitivity and specificity for positive SIRS criteria were 0.86 (95% CI, 0.79–0.92) and 0.29 (95% CI, 0.17–0.45), respectively. The PLR, NLR, and the pooled DOR were 1.22 (95% CI, 1.06–1.39), 0.46 (95% CI, 0.39–0.56), and 2.59 (95% CI, 1.98–3.38), respectively (see Additional file 4). Figure 3a and b show HSROC curves for both tools in predicting in-hospital mortality. The AUC was 0.74 (95% CI, 0.70–0.78) for positive qSOFA scores and 0.71 (95% CI, 0.67–0.75) for positive SIRS criteria. In a comparison of the prognostic performance of the two methods for in-hospital mortality, no significant differences were observed between the AUCs (P = 0.816).
Hierarchical summary ROC (SROC) curves for (a) positive quick Sequential (Sepsis-related) Organ Failure Assessment (qSOFA) scores and (b) positive systemic inflammatory response syndrome (SIRS) criteria for predicting in-hospital mortality, and for (c) positive qSOFA scores and (d) positive SIRS criteria for early detection of acute organ dysfunction in patients with infection outside the intensive care unit. SENS Sensitivity; SPEC, Specificity
In addition, we retrieved data regarding prognostic performance according to the qSOFA score at other cutoff values from three studies [21, 30, 34]. In pooled estimates, when qSOFA was ≥ 1 point, the sensitivity, specificity, and AUC of positive qSOFA scores for in-hospital mortality were 0.93 (95% CI, 0.92–0.94), 0.13 (95% CI, 0.12–0.13), and 0.78 (95% CI, 0.72–0.84), respectively. In the cases with a cutoff value of 3 points, the sensitivity, specificity, and AUC of positive qSOFA scores were 0.17 (95% CI, 0.16–0.19), 0.96 (95% CI, 0.96–0.96), and 0.95 (95% CI, 0.88–1.00), respectively.
Meta-regression for positive qSOFA scores in predicting in-hospital mortality
Between-study heterogeneity was highly represented in the sensitivities and specificities among the studies (Fig. 2). Table 2 shows the results of univariate meta-regression analyses in identifying potential sources of heterogeneity. For studies in which researchers evaluated the prognostic performance of positive qSOFA scores, study location, overall mortality rate, timing of the qSOFA score measurement, and disease severity were probable sources of heterogeneity. For these four potential sources of heterogeneity, meta-regression analyses using the model weighted by the inverse of the variance revealed that overall mortality ≥ 10% and timing of the qSOFA score measurement were independently associated with between-study heterogeneity (relative diagnostic OR [RDOR], 0.71; 95% CI, 0.53–0.96; P = 0.03; and RDOR, 0.59; 95% CI, 0.43–0.81; P < 0.01, respectively) (Table 3). For studies with overall mortality ≥ 10% and < 10%, the AUCs were 0.73 (95% CI, 0.67–0.79) and 0.78 (95% CI, 0.76–0.83), respectively. For positive qSOFA scores measured at the time of initial suspicion of infection and the worst values, the AUCs were 0.73 (95% CI, 0.69–0.77) and 0.76 (95% CI, 0.72–0.80), respectively.
Diagnostic accuracy for acute organ dysfunction using positive qSOFA scores and SIRS criteria
We could retrieve ten data from nine studies regarding the prognostic performance of positive qSOFA scores in predicting acute organ dysfunction [19, 23, 25, 30, 31, 33,34,35, 39]. Researchers in four studies reported the performance of positive SIRS criteria in predicting acute organ dysfunction [19, 25, 33, 39]. In the pooled estimates, patients with positive qSOFA scores and SIRS criteria were associated with acute organ dysfunction in 82.8% (2433 of 2936 patients) and 36.2% (1830 of 5047 patients), respectively. The pooled sensitivity and specificity of positive qSOFA score for acute organ dysfunction were 0.47 (95% CI, 0.28–0.66) and 0.93 (95% CI, 0.88–0.97), respectively. The PLR, NLR, and pooled DOR were 7.13 (95% CI, 4.42–11.49), 0.57 (95% CI, 0.40–0.81), and 12.49 (95% CI, 6.69–23.31), respectively (see Additional file 5). The pooled sensitivity and specificity of positive SIRS criteria were 0.83 (95% CI, 0.71–0.91) and 0.49 (95% CI, 0.29–0.69), respectively. The PLR, NLR, and pooled DOR were 1.64 (95% CI, 1.19–2.26), 0.34 (95% CI, 0.24–0.47), and 4.89 (95% CI, 3.11–7.67), respectively (see Additional file 6). Figure 3c and d show HSROC curves for both tools in predicting acute organ dysfunction. The AUC was 0.86 (95% CI, 0.83–0.89) for positive qSOFA score and 0.76 (95% CI, 0.73–0.80) for positive SIRS criteria. In a comparison of the prognostic performance of the two tools for acute organ dysfunction, the AUC for positive qSOFA score was higher than that for positive SIRS criteria (P < 0.001).
Diagnostic accuracy for ICU admission using positive qSOFA scores and SIRS criteria
We could retrieve data from ten studies regarding the prognostic performance of positive qSOFA scores in predicting ICU admission [20, 21, 25, 26, 30,31,32, 35, 36, 38]. Researchers in three studies reported the performance of positive SIRS criteria in predicting ICU admission [21, 25, 26]. In the pooled estimates, patients with positive qSOFA scores and SIRS criteria were associated with ICU admission of 37.0% (5325 of 14,384 patients) and 24.3% (6741 of 27,759 patients), respectively. The pooled sensitivity and specificity of positive qSOFA score for ICU admission were 0.53 (95% CI, 0.52–0.54) and 0.75 (95% CI, 0.75–0.76), respectively (see Additional file 7). The PLR, NLR, and pooled DOR were 2.24 (95% CI, 1.91–2.77), 0.74 (95% CI, 0.67–0.83), and 3.16 (95% CI, 2.42–4.11), respectively. The pooled sensitivity and specificity for positive SIRS criteria were 0.91 (95% CI, 0.90–0.92) and 0.14 (95% CI, 0.13–0.14), respectively. The PLR, NLR, and pooled DOR were 1.11 (95% CI, 0.96–2.26), 0.61 (95% CI, 0.39–0.95), and 1.83 (95% CI, 1.02–3.30), respectively (see Additional file 8). Positive qSOFA scores tended to be inferior to positive SIRS criteria in predicting ICU admission, although this was not statistically significant (AUC, 0.63; 95% CI, 0.62–0.64; vs. AUC, 0.78; 95% CI, 0.58–0.98; P = 0.121) (see Additional file 9).
Discussion
In the present systematic review and meta-analysis, we analyzed the prognostic performance of positive qSOFA scores for predicting in-hospital mortality in patients with suspected or confirmed infection outside the ICU. We found that positive qSOFA scores had a sensitivity of 0.51 and a specificity of 0.83 for in-hospital mortality as compared with a sensitivity of 0.86 and a specificity of 0.29 for positive SIRS scores. Positive qSOFA scores and SIRS criteria showed similar discrimination for in-hospital mortality (AUC, 0.74 vs. 0.71; P = 0.816). Considerable heterogeneity was found in the pooled estimates among the positive qSOFA scores. Using meta-regression analysis, potential sources of heterogeneity were overall mortality and the timing of the qSOFA score measurement. In addition, although the discriminatory capacity of acute organ dysfunction using positive qSOFA score was good, the sensitivity was very low. The sensitivity of positive qSOFA scores in predicting ICU admission was also low.
In two international consensus conferences in 1991 and 2001, sepsis was defined as a suspected source of infection in the setting of SIRS criteria ≥ 2 [8, 9]. For over two decades, the SIRS criteria have been used to be identify sepsis. However, the SIRS criteria have not been useful in differentiating patients with infection outside the ICU from those patients outside the ICU with noninfectious diseases, such as severe trauma, burns, pancreatitis, and ischemia-reperfusion injury [40, 41]. Also, researchers in previous studies reported that 93% of ICU patients and 47% of ward patients who were hospitalized developed positive SIRS at least once during their hospital stay [40, 42]. A large retrospective study showed that a positive SIRS score missed one in eight patients with infection and organ dysfunction [5]. Because of its poor specificity, the SIRS criteria have been regarded as impractical for the screening of sepsis [40, 42].
In the Sepsis-3 guidance, the 2016 SCCM/ESICM proposed the concept of the qSOFA score to predict poor outcomes in patients with suspected infection, and the SIRS criteria were no longer recommended as part of the clinical criteria for sepsis [1]. From the introduction of the new concept, there has been a need to evaluate the prognostic value of qSOFA for predicting outcomes. Several validation studies have followed, and the ability of the qSOFA score to predict in-hospital mortality has been greater than that of the SIRS criteria among patients with suspected infection outside the ICU [6, 28]. We found that patients with positive qSOFA scores were associated with in-hospital mortality of 12.9%, acute organ dysfunction of 82.8%, and ICU admission of 37.0% after the initiation of therapy. In addition, our pooled estimates demonstrated that positive qSOFA scores had high specificity for early risk assessment but poor sensitivity. The qSOFA score would provide great value as a clinical tool to promptly identify patients with infection likely to develop adverse outcomes outside the ICU.
However, we observed wide heterogeneity among the included studies. An important objective of meta-analysis is to investigate the evidence of heterogeneity among studies and to determine whether differences in study design explain the heterogeneity. We found that these findings could be explained partly by potential sources of bias. First, there is the timing of the qSOFA score measurement. Measurement of the qSOFA score at the time of initial suspicion of infection seemed to be easy and clear to apply in clinical practice. However, in pooled estimates, the diagnostic performance of positive qSOFA scores for predicting in-hospital mortality was low at the time of initial suspicion of infection. The use of the worst qSOFA score during the entire stay of the patient enhanced sensitivity. Considering that sepsis is a dynamic, heterogeneous disease, these findings highlight the importance of serial reassessment of the qSOFA score. Second, the severity of infection may affect diagnostic accuracy. When critically ill patients with sepsis or septic shock were included in the meta-analysis, the sensitivity of a positive qSOFA score was enhanced. Otherwise, in pooled estimates targeting patients with common suspected or confirmed infections, the sensitivity of a positive qSOFA score was low. Similarly, pooled estimates for trials that included an overall mortality > 10% increased the sensitivity of a positive qSOFA score. Third, study location may be a factor in heterogeneity. The differences in the results between studies may be explained by differences in the healthcare systems of each country. Specifically, high health care accessibility is likely to be biased toward low disease severity.
Early recognition of sepsis and promptly providing aggressive fluid resuscitation and administration of antimicrobials is crucial to improving outcomes and decreasing sepsis-related mortality [43]. The qSOFA score has an advantage as a simple tool; namely, it has few variables and no necessary laboratory results, and it can be assessed repeatedly over time. However, the qSOFA score reflects only some of the variables in the new sepsis definition. In our pooled estimates, its low sensitivity, which may lead to delays in initiation of adequate management for some patients, has resulted in concerns about its role as a bedside tool outside the ICU [23]. To facilitate the early recognition of patients at higher risk for poor outcomes, some specificity of the qSOFA score would need to be sacrificed to increase sensitivity [23]. Therefore, its ability to predict mortality may be enhanced when combined with other clinical factors that are correlated with higher risk of death and acute organ dysfunction, such as age, nursing home residence, arterial pH, and lactate and end-tidal carbon dioxide concentrations [23, 27, 28]. In addition, a recent retrospective study reported that the diagnostic accuracy was highest in predicting acute organ dysfunction in the ED when the cutoff qSOFA score was ≥ 1 point [34]. However, in our pooled estimates of the qSOFA score ≥ 1 point for in-hospital mortality, although the pooled sensitivity increased, specificity largely decreased. The findings from a recent observational cohort study were consistent with our results [21]. Also, the qSOFA score ≥ 1 point had diagnostic accuracy similar to positive SIRS criteria for in-hospital mortality or ICU transfer, which suggested that this lower cutoff could be used to enhance the sensitivity of the qSOFA score [21]. This study also reported that other early warning scores such as the Modified Early Warning Score and the National Early Warning Score were more accurate than the qSOFA score for predicting adverse outcomes outside the ICU, and, owing to the costs, its authors did not recommend changing from these other early warning scores to the qSOFA score [21].
The strengths of our study are that we (1) followed a standard protocol using a comprehensive search strategy, (2) applied a bivariate random effects model and HSROC analyses to the data, and (3) identified potential sources of bias by adding covariates to the bivariate model for meta-regression. Our findings could be useful for physicians implementing qSOFA outside the ICU. Meanwhile, there are some study limitations. First, there was significant heterogeneity among the included studies, although large heterogeneities are commonly seen in systematic reviews of diagnostic test accuracy studies [44]. Second, although we performed meta-regression analysis to determine which studies contributed to the observed heterogeneity, the results of this analysis should be interpreted with caution owing to limited statistical power. Third, we found only four and three studies using positive SIRS criteria for acute organ dysfunction and ICU admission, respectively. Although our results reveal that the discriminatory capacity for acute organ dysfunction of positive qSOFA scores was higher than positive SIRS criteria, limited data did not allow us to draw a robust conclusion. Finally, although the qSOFA score was a bedside criterion targeting patients with suspected infection, a considerable number of patients who were included in this meta-analysis had already-confirmed infections. This could lead to an overestimation of the predictive ability of positive qSOFA scores as well as positive SIRS criteria.
Conclusions
We found that positive qSOFA scores had high specificity but poor sensitivity for predicting in-hospital mortality, acute organ dysfunction, and ICU admission in patients with infection outside the ICU. Therefore, a positive qSOFA score seemed to be limited in the early identification of poor outcomes in these patients in routine clinical practice. Meanwhile, positive SIRS criteria were found to be too sensitive and insufficiently specific to predict in-hospital mortality. In the present study, between-study heterogeneity was highly represented, and an overall mortality rate ≥ 10% and timing of qSOFA score measurement could be significant factors in this heterogeneity. Our findings indicate that the development of enhanced or modified bedside tools may be necessary.
Abbreviations
- CIS:
-
Clinical Impression Score
- CRB:
-
Confusion, respiratory rate ≥ 30/minute, systolic blood pressure < 90 mmHg or diastolic blood pressure ≤ 60 mmHg
- CRB-65:
-
Confusion, respiratory rate ≥ 30/minute, systolic blood pressure < 90 mmHg or diastolic blood pressure ≤ 60 mmHg, age ≥ 65 years
- CURB-65:
-
Confusion, urea nitrogen, respiratory rate ≥ 30/minute, systolic blood pressure < 90 mmHg or diastolic blood pressure ≤ 60 mmHg, age ≥ 65 years
- DOR:
-
Diagnostic OR
- ED:
-
Emergency department
- HSROC:
-
Hierarchical summary ROC
- ICU:
-
Intensive care unit
- MODS:
-
Multiple organ dysfunction syndrome
- mSOFA:
-
Modified Sequential (Sepsis-related) Organ Failure Assessment
- NA:
-
Not available
- NLR:
-
Negative likelihood ratio
- PIRO:
-
Predisposition, infection, response, organ dysfunction model
- PLR:
-
Positive likelihood ratio
- qSOFA:
-
Quick Sequential (Sepsis-related) Organ Failure Assessment
- QUADAS-2:
-
Quality Assessment of Diagnostic Accuracy Studies 2 tool
- RDOR:
-
Relative diagnostic OR
- SCCM/ESICM:
-
Society of Critical Care Medicine/European Society of Intensive Care Medicine
- SENS:
-
Sensitivity
- Sepsis-3:
-
SCCM/ESICM Third International Consensus Definitions for Sepsis and Septic Shock
- SIRS:
-
Systemic inflammatory response syndrome
- SK:
-
“Sepsis Kills” program clinical excellence committee
- SOFA:
-
Sequential (Sepsis-related) Organ Failure Assessment
- SPEC:
-
Specificity
- SROC:
-
Summary ROC
- UPMC:
-
University of Pittsburgh Medical Center
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801–10.
Liu V, Escobar GJ, Greene JD, Soule J, Whippy A, Angus DC, Iwashyna TJ. Hospital deaths in patients with sepsis from 2 independent cohorts. JAMA. 2014;312:90–2.
Bhattacharjee P, Edelson DP, Churpek MM. Identifying patients with sepsis on the hospital wards. Chest. 2017;151:898–907.
Vincent JL, Opal SM, Marshall JC, Tracey KJ. Sepsis definitions: time for change. Lancet. 2013;381:774–5.
Kaukonen KM, Bailey M, Pilcher D, Cooper DJ, Bellomo R. Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med. 2015;372:1629–38.
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, Rubenfeld G, Kahn JM, Shankar-Hari M, Singer M, et al. Assessment of clinical criteria for sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:762–74.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003;29:530–8.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ, ACCP/SCCM Consensus Conference Committee. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101:1644–55.
Borzecki AM, Christiansen CL, Chew P, Loveland S, Rosen AK. Comparison of in-hospital versus 30-day mortality assessments for selected medical conditions. Med Care. 2010;48:1117–21.
Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25.
Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58:982–90.
Rutter CM, Gatsonis CA. A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med. 2001;20:2865–84.
Thompson SG. Why sources of heterogeneity in meta-analysis should be investigated. BMJ. 1994;309:1351–5.
Lijmer JG, Mol BW, Heisterkamp S, Bonsel GJ, Prins MH, van der Meulen JH, Bossuyt PM. Empirical evidence of design-related bias in studies of diagnostic tests. JAMA. 1999;282:1061–6.
Moses LE, Shapiro D, Littenberg B. Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic approaches and some additional considerations. Stat Med. 1993;12(14):1293–316.
Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58:882–93.
April MD, Aguirre J, Tannenbaum LI, Moore T, Pingree A, Thaxton RE, Sessions DJ, Lantry JH. Sepsis clinical criteria in emergency department patients admitted to an intensive care unit: an external validation study of quick Sequential Organ Failure Assessment. J Emerg Med. 2017;52:622–31.
Askim Å, Moser F, Gustad LT, Stene H, Gundersen M, Åsvold BO, Dale J, Bjørnsen LP, Damås JK, Solligård E. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality – a prospective study of patients admitted with infection to the emergency department. Scand J Trauma Resusc Emerg Med. 2017;25:56.
Chen YX, Wang JY, Guo SB. Use of CRB-65 and quick Sepsis-related Organ Failure Assessment to predict site of care and mortality in pneumonia patients in the emergency department: a retrospective study. Crit Care. 2016;20:167.
Churpek MM, Snyder A, Han X, Sokol S, Pettit N, Howell MD, Edelson DP. Quick Sepsis-related Organ Failure Assessment, systemic inflammatory response syndrome, and early warning scores for detecting clinical deterioration in infected patients outside the intensive care unit. Am J Respir Crit Care Med. 2017;195:906–11.
Donnelly JP, Safford MM, Shapiro NI, Baddley JW, Wang HE. Application of the Third International Consensus Definitions for Sepsis (Sepsis-3) classification: a retrospective population-based cohort study. Lancet Infect Dis. 2017;17:661–70.
Dorsett M, Kroll M, Smith CS, Asaro P, Liang SY, Moy HP. qSOFA has poor sensitivity for prehospital identification of severe sepsis and septic shock. Prehospital Emerg Care. 2017;21:489–97.
Finkelsztein EJ, Jones DS, Ma KC, Pabon MA, Delgado T, Nakahira K, Arbo JE, Berlin DA, Schenck EJ, Choi AM, et al. Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit Care. 2017;21:73.
Forward E, Konecny P, Burston J, Adhikari S, Doolan H, Jensen T. Predictive validity of the qSOFA criteria for sepsis in non-ICU inpatients. Intensive Care Med. 2017;43:945–6.
Freund Y, Lemachatti N, Krastinova E, Van Laer M, Claessens YE, Avondo A, Occelli C, Feral-Pierssens AL, Truchot J, Ortega M, et al. Prognostic accuracy of Sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA. 2017;317:301–8.
Giamarellos-Bourboulis EJ, Tsaganos T, Tsangaris I, Lada M, Routsi C, Sinapidis D, Koupetori M, Bristianou M, Adamis G, Mandragos K, et al. Validation of the new Sepsis-3 definitions: proposal for improvement in early risk identification. Clin Microbiol Infect. 2017;23:104–9.
Henning DJ, Puskarich MA, Self WH, Howell MD, Donnino MW, Yealy DM, Jones AE, Shapiro NI. An emergency department validation of the SEP-3 sepsis and septic shock definitions and comparison with 1992 consensus definitions. Ann Emerg Med. 2017;70(4):544–52.e5. doi: https://doi.org/10.1016/j.annemergmed.2017.01.008.
Huson MA, Kalkman R, Grobusch MP, van der Poll T. Predictive value of the qSOFA score in patients with suspected infection in a resource limited setting in Gabon. Travel Med Infect Dis. 2017;15:76–7.
Hwang SY, Jo IJ, Lee SU, Lee TR, Yoon H, Cha WC, Sim MS, Shin TG. Low accuracy of positive qSOFA criteria for predicting 28-day mortality in critically ill septic patients during the early period after emergency department presentation. Ann Emerg Med. 2018;71(1):1–9.e2. doi: https://doi.org/10.1016/j.annemergmed.2017.05.022.
Kim M, Ahn S, Kim WY, Sohn CH, Seo DW, Lee YS, Lim KS. Predictive performance of the quick Sequential Organ Failure Assessment score as a screening tool for sepsis, mortality, and intensive care unit admission in patients with febrile neutropenia. Support Care Cancer. 2017;25:1557–62.
Kolditz M, Scherag A, Rohde G, Ewig S, Welte T, Pletz M, CAPNETZ Study Group. Comparison of the qSOFA and CRB-65 for risk prediction in patients with community-acquired pneumonia. Intensive Care Med. 2016;42:2108–10.
Mellhammar L, Wullt S, Lindberg A, Lanbeck P, Christensson B, Linder A. Sepsis incidence: a population-based study. Open Forum Infect Dis. 2016;3:ofw207.
Park HK, Kim WY, Kim MC, Jung W, Ko BS. Quick Sequential Organ Failure Assessment compared to systemic inflammatory response syndrome for predicting sepsis in emergency department. J Crit Care. 2017;42:12–7.
Peake SL, Delaney A, Bailey M, Bellomo R, ARISE Investigators. Potential impact of the 2016 Consensus Definitions of Sepsis and Septic Shock on future sepsis research. Ann Emerg Med. 2017;70(4):553–61.e1. https://doi.org/10.1016/j.annemergmed.2017.04.007.
Quinten VM, van Meurs M, Wolffensperger AE, Ter Maaten JC, Ligtenberg JJM. Sepsis patients in the emergency department: stratification using the Clinical Impression Score, Predisposition, Infection, Response and Organ dysfunction score or quick Sequential Organ Failure Assessment score? Eur J Emerg Med. 2017. https://doi.org/10.1097/MEJ.0000000000000460.
Ranzani OT, Prina E, Menéndez R, Ceccato A, Cilloniz C, Méndez R, Gabarrus A, Barbeta E, Li Bassi G, Ferrer M, et al. New sepsis definition (Sepsis-3) and community-acquired pneumonia mortality: a validation and clinical decision-making study. Am J Respir Crit Care Med. 2017;196(10):1287–97. doi: https://doi.org/10.1164/rccm.201611-2262OC.
Wang JY, Chen YX, Guo SB, Mei X, Yang P. Predictive performance of quick Sepsis-related Organ Failure Assessment for mortality and ICU admission in patients with infection at the ED. Am J Emerg Med. 2016;34:1788–93.
Williams JM, Greenslade JH, McKenzie JV, Chu K, Brown AFT, Lipman J. Systemic inflammatory response syndrome, quick Sequential Organ Function Assessment, and organ dysfunction: insights from a prospective database of ED patients with infection. Chest. 2017;151:586–96.
Churpek MM, Zadravecz FJ, Winslow C, Howell MD, Edelson DP. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015;192:958–64.
Jaimes F, Garces J, Cuervo J, Ramirez F, Ramirez J, Vargas A, Quintero C, Ochoa J, Tandioy F, Zapata L, et al. The systemic inflammatory response syndrome (SIRS) to identify infected patients in the emergency room. Intensive Care Med. 2003;29:1368–71.
Sprung CL, Sakr Y, Vincent JL, Le Gall JR, Reinhart K, Ranieri VM, Gerlach H, Fielden J, Groba CB, Payen D. An evaluation of systemic inflammatory response syndrome signs in the Sepsis Occurrence in Acutely Ill Patients (SOAP) study. Intensive Care Med. 2006;32:421–7.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Dinnes J, Deeks J, Kirby J, Roderick P. A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy. Health Technol Assess. 2005;9(12).
Acknowledgements
Not applicable.
Funding
This work was supported by a research grant from the Jeju National University Hospital Development Fund in 2017.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Disclaimer
The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
JUS and CKS contributed to data acquisition, data interpretation, and statistical analysis and drafted the manuscript. HKP contributed to statistical analysis and manuscript revision. SRS completed the statistical analysis. JL contributed to the study design, data acquisition, data interpretation, statistical analysis, writing of the manuscript, and critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Study protocol, search strategies, and quality assessment. (PDF 115 kb)
Additional file 2:
Summary for risk of bias of included studies and risk of bias graph for the included studies. (PDF 32 kb)
Additional file 3:
Funnel plot for publication bias assessment of studies for (a) positive qSOFA score and (b) positive SIRS criteria score for the prediction of in-hospital mortality. (PDF 97 kb)
Additional file 4:
Paired forest plots of sensitivity and specificity of positive SIRS criteria in predicting in-hospital mortality of infected patients outside the intensive care unit. (PDF 268 kb)
Additional file 5:
Paired forest plots of sensitivity and specificity of positive qSOFA score in identifying organ dysfunction in infected patients outside the intensive care unit. (PDF 263 kb)
Additional file 6:
Paired forest plots of sensitivity and specificity of positive SIRS criteria score in identifying organ dysfunction in infected patients outside the intensive care unit. (PDF 83 kb)
Additional file 7:
Paired forest plots of sensitivity and specificity of positive qSOFA score in identifying ICU admission in infected patients outside the intensive care unit. (PDF 170 kb)
Additional file 8:
Paired forest plots of sensitivity and specificity of positive SIRS criteria in identifying ICU admission in infected patients outside the intensive care unit. (PDF 107 kb)
Additional file 9:
Summary receiver operating characteristic curves for (a) positive qSOFA score and (b) positive SIRS criteria for predicting ICU admission in infected patients outside the intensive care unit. (PDF 77 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Song, JU., Sin, C.K., Park, H.K. et al. Performance of the quick Sequential (sepsis-related) Organ Failure Assessment score as a prognostic tool in infected patients outside the intensive care unit: a systematic review and meta-analysis. Crit Care 22, 28 (2018). https://doi.org/10.1186/s13054-018-1952-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-018-1952-x